Introduction
Juvenile nasopharyngeal angiofibroma (JNA) is a rare
benign neoplasm characterized by proliferating irregular vascular
channels within a fibrous stroma composed of spindle cells in a
dense collagen matrix (1,2). Despite being classified as benign
tumors, JNAs often exhibit an aggressive growth pattern with
possible intracranial spreading. These features have stimulated
numerous theories on tumor origin, focusing on the vascular or the
stromal component (3).
Nevertheless, the implicated neoplastic cell responsible for
sustained growth remains a matter of debate (1,3,4).
Recent studies based on vascular irregularities
(thickness of the vessel walls, discontinuous vascular basal
laminae and focal lack of pericytes) have led to the hypothesis
that JNA is a vasoproliferative malformation (2,3).
This suggestion of a vascular tumor origin is supported by an
embryological explanation, based on the involvement of plexus
remnants deriving from incomplete regression of the first branchial
arch artery, which were incorporated into the vascular tumor
component (3,4).
The presence of proteins such as merosin (laminin
α2) and collagens type VI and 1A2, which were recently described as
being highly expressed in JNA vessels, is suggestive of vessels in
an early developmental vascular differentiation state (5–7).
Notably, merosin and type VI collagen were also elevated in several
types of cancer and in proliferative hemangiomas. The latter are
vascular lesions characterized by abnormal excessive endothelial
cell proliferation (5–9).
A series of immunohistochemical studies have been
performed to analyze angiogenic activators and vessel growth
promoting factors in JNA samples. Vascular markers, such as CD31,
CD34 and von Willebrand factor (vWF), were previously documented in
JNAs. However, such pan endothelium biomarkers did not discriminate
between vascular and lymphatic cells, and some are not restricted
to blood vessels (10). TGFβ1,
FGF, vascular endothelial growth factor (VEGF A) and its receptors,
VEGFR1 (Flt-1) and VEGFR2 (KDR), were also reported to be expressed
in JNA endothelial cells (11–19).
Of note, several of these growth factors were also elevated in both
hemangiomas and in tumor-associated blood vessels (8,20).
Thus, is would appear that JNA vessels exhibit
malformative and endothelial proliferative features, as well as
neoplastic markers, although they maintain benign characteristics.
Similar aspects of angiogenesis in vascular anomalies and tumors
were recently discussed (4).
Given that the most conspicuous feature of JNAs is
the endothelial proliferative state, inhibition of angiogenesis is
thought to be a promising strategy for their treatment. Our
research has focused on identifying other markers that may provide
additional information regarding the abnormal vascular component of
JNAs. The first step in the present study was to evaluate the
expression of endothelial markers involved in cell differentiation
and cell growth, such as friend leukemia integration-1 (Fli-1) and
endoglin. Fli-1 is a nuclear transcription factor that is
considered to be a very reliable marker of endothelial
differentiation. Fli-1 was reported to be involved in cellular
proliferation and tumorigenesis, as well as in the suppression of
the expression of genes such as Rb and Bcl-2 protein (21,22).
Endoglin (CD105) is a transmembranic glycoprotein that is a marker
of activated endothelium; its vascular expression is limited to
proliferating endothelial cells, with no expression in normal
vessels (23). To investigate the
vascular differentiation state of JNA endothelial cells, specific
markers of lymphatic vessels, such as podoplanin and VEGFR3 and its
ligand VEGFC (24,25), were also analyzed. The erythrocyte
transporter (GLUT-1) was described in fetal endothelial cells
(26) in solid tumors with
enhanced glycolitic demand (27),
and is a universal trait of hemangiomas, discriminating these
tumors from vascular malformations (28). Thus, we evaluated the
immunohistochemical expression of GLUT-1 in JNAs and compared its
expression to that displayed by hemangiomas and vascular
malformations used as the control.
Studies focused on differences in gene expression in
endothelial cells derived from tumor tissues have revealed the
enrichment of genes involved in tissue remodeling, a hallmark of
post developmental angiogenesis, such as stromelysin 3 (ST3) and
secreted acid protein rich in cysteine (SPARC; or osteonectin).
These are up-regulated in a number of pathological processes
(29–31). ST3 (MMP11) is a member of the
metalloprotease (MMP) family and is an established connective
tissue-derived factor associated with embryogenesis, wound healing
and tissue involution (31). SPARC
is a matricellular glycoprotein that has counter adhesive and
antiproliferative functions and is associated with developing
vessels and tumor blood vessels (32). Its importance in the angiogenic
events in JNAs has been previously hypothesized (33). Thus, the expression of ST3 and
SPARC was investigated in the present study.
Materials and methods
Case selection
Twenty-two patients with JNA who underwent surgery
between 2000 and 2006 at the Hospital das Clínicas da Faculdade de
Medicina da Universidade de São Paulo were selected for this study.
All patients were male and between 12 and 25 years of age at the
time of surgery (median 16 years). Since the study was
retrospective, informed patient consent was waived. However, any
form of patient identification was avoided. The study was approved
by the Ethical Committee for Research Projects of the Hospital das
Clínicas da Faculdade de Medicina da Universidade de São Paulo.
The tumors were staged using the Fisch system and
ranged from stage II to IIIa. Recurrence was observed in 20% of the
cases. Frozen tumor samples were obtained from 18 of the patients
with JNAs; samples of paired turbinate tissues were obtained from
15 of the 18 patients and used for ST3 mRNA determination by
Northern blot analysis.
In addition, 124 cases of proliferative hemangioma
and 135 cases of vascular malformation excised at the Hospital do
Câncer A.C. Camargo (São Paulo, Brasil) were examined. The age of
the patients at surgery ranged from 1 to 208 months (median 42),
and there was a predominance of female patients (69.5%).
The study was approved by the Hospital A.C. Camargo
Institutional Ethics Committee.
Immunohistochemical analysis
A representative paraffin block was selected from
each case, and 3 μm-thick sections were prepared for
immunohistochemical staining.
Sections were deparaffinized and rehydrated through
a graded series of ethanol. Antigen retrieval was performed in a
pressure cooker using citrate buffer at a pH of 6.0. Endogen
peroxidase activity was blocked by 3% perhidrol. Slides were rinsed
with PBS (pH 7.4) and incubated at 4°C for 18 h with the primary
antibodies (Table I). This was
followed by incubation with the respective appropriate secondary
antibodies against podoplanin, GLUT-1, ST3, FLI-1, SPARC, endoglin,
VEGFA and VEGFC, as well as their receptors (VEGFR1 and VEGFR3) and
CD34, CD31 and vWF (factor VIII-related antigen).
 | Table I.Antibodies used for
immunohistochemical analysis. |
Table I.
Antibodies used for
immunohistochemical analysis.
| Antibodies | Clones | Sources | Dilutions |
|---|
| CD34 | QBEnd 10 | M7165; Dako,
Glostrup, Denmark | 1:100 |
| CD31 | JC/70A | M0823; Dako | 1:50 |
| Factor VIII | Polyclonal | A0082; Dako | 1:300 |
| VEGF (A-20) | Polyclonal | sc152; Santa Cruz
Biotechnology, Santa Cruz, CA, USA | 1:600 |
| GLUT-1 | Polyclonal | A3536; Dako | 1:500 |
| Podoplanin | 18H5 | DM3500; Acris
antibodies, Hiddenhausen, Germany | 1:200 |
| VEGFC | Goat
polyclonal | sc1881; Santa Cruz
Biotechnology | 1:100 |
| ST3/MMP11 | SL3.05 | MS1035P;
NeoMarkers, Fremont, CA, USA | 1:100 |
| VEGFR3 (FLT4) | Rabbit
polyclonal | RB1527; Thermo
Scientific, Fremont, CA, USA | 1:400 |
| VEGFR1 (Flt-1) | Rabbit
polyclonal | RB9255; Thermo
Scientific | 1:100 |
| FLI-1 | Mouse
monoclonal | LLC CM274A,B;
Biocare Medical, Concord, CA, USA | 1:30 |
| SPARC | Rabbit
polyclonal | Ab1858; Chemicon,
Temecura, CA, USA | 1:2,000 |
| Endoglin | SN6H | MS1290;
NeoMarkers | 1:100 |
StreptABComplex – HRP Duet mouse/rabbit (K0492;
Dako) diluted 1:200 in PBS was used as the detection system. Slides
were developed in diaminobenzidine solution and counterstained with
Harris hematoxylin.
Immunoreactivity was assessed in both vascular
endothelial cells and in the stroma of JNA cases by staff
pathologists (H.T., H.C. and F.A.S.). The sections were scored
according to the degree of positivity observed in the cells.
According to our grading scale, cases presenting <10% of stained
cells were considered negative. Sections incubated without the
primary antibody served as negative controls.
RNA isolation and Northern blot
analysis
The frozen tissues were pulverized and the total RNA
was isolated by the guanidinium isothyocyanate method. Northern
blot analysis was performed as previously described (34). An ST3 probe was radiolabeled using
a rediprime DNA labeling system with [α-32p]dCTP
(Amersham-Pharmacia). The ST3/MMP11 cDNA probe was donated by Dr P.
Chambon of the Institute of Genetics and Molecular and Cellular
Biology (Strasbourg, France). The autoradiograms were individually
quantified by densitometry, and the ratio of each mRNA to 18S mRNA
was compared to the average ratio of the controls. The mean value
of the expression of the genes in normal turbinates was defined as
the basal or normal expression. An expression of >2-fold above
that found in normal turbinate tissues was defined as
overexpression. Immunohistology was performed to visualize ST3
protein expression in JNAs.
Results
A total of 22 cases of JNA were included in this
study. Results regarding the frequency of positivity of the
antibodies utilized are shown in Table
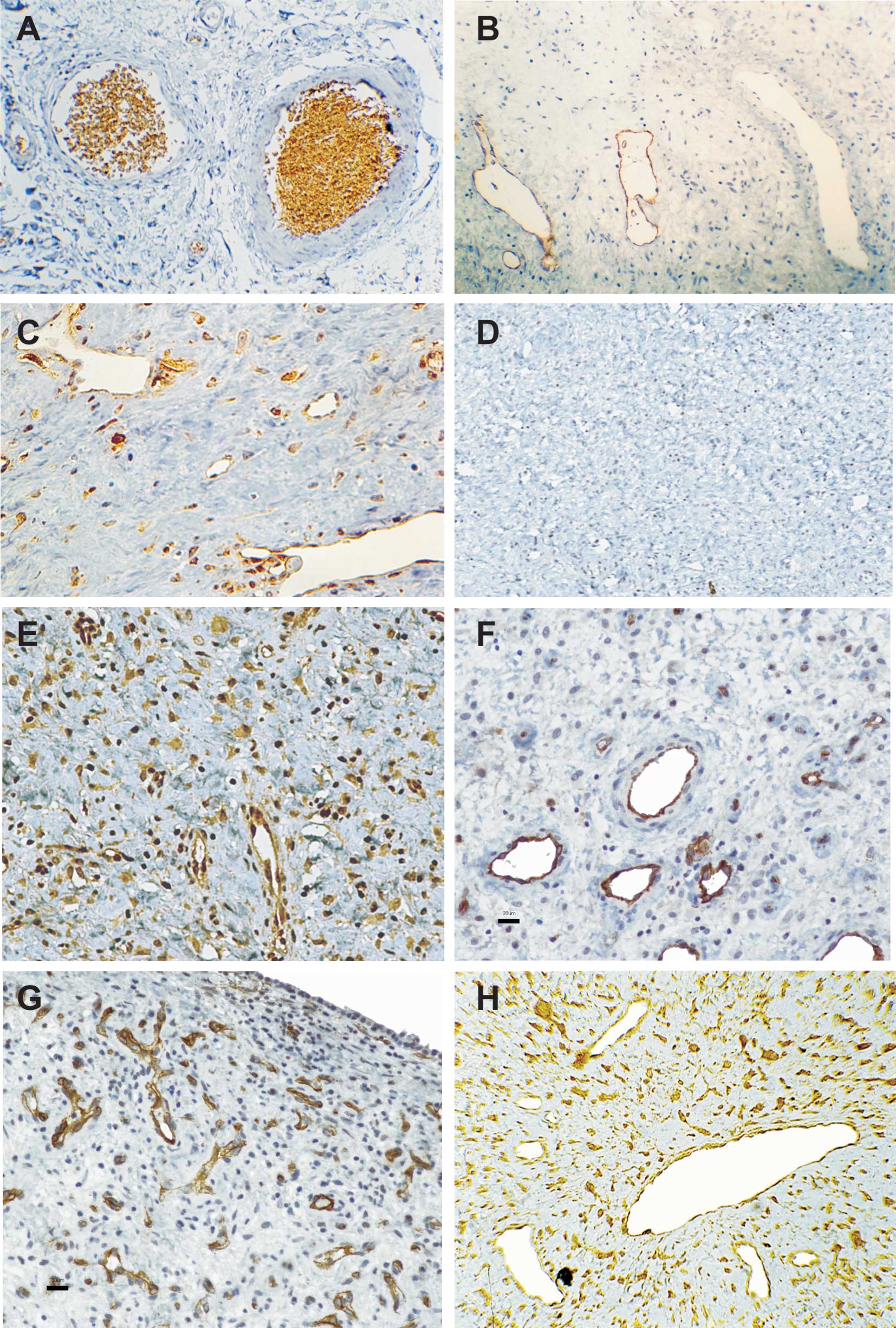
II. Podoplanin was evaluated in the JNAs and, although it was
evident in the endothelial lining of small lymphatic vessels, was
consistently not detected in JNA vessels (Fig. 1B). VEGFC expression was noted in
both stromal and endothelial cells in all cases (Fig. 1C). All cases were uniformly
negative for VEGFR3 (Fig. 1D). The
pan endothelial marker FLI-1 and the marker of activated
endothelium, endoglin (CD105), were positive in the vessels in 100%
of the cases. Endoglin was absent in the stromal cells. Single
cells also stained positively for FLI-1, but it was not clear
whether these cells were endothelial or stromal cells (Fig. 1E and F). SPARC expression was found
primarily in the JNA endothelial cells, but was also observed in
stellated shaped cells of the stroma (Fig. 1G). Of the 15 cases analyzed by
immunohistochemistry, 66.7 and 33.3% showed ST3 positivity,
respectively, in vessels and in numerous single stromal cells
(Fig. 1H). Samples of JNA were
analyzed for GLUT-1, and the rate of positivity was compared to
that found in hemangiomas and in vascular malformation cases.
GLUT-1 immunoreactivity was present in the majority of hemangiomas
tested (Table III, Fig. 1A), but was absent in vascular
malformations and nasofibromas. This difference was highly
significant (p<0.01).
 | Table II.Frequency of endothelial cell markers
in juvenile-nasoangiofibromas vessels. |
Table II.
Frequency of endothelial cell markers
in juvenile-nasoangiofibromas vessels.
| Markers | Frequency (%) |
|---|
| FLI-1 | 22/22 (100) |
| Endoglin
(CD105) | 22/22 (100) |
| Podoplanin | 0/22 (0) |
| VEGFR3 | 0/22 (0) |
| VEGFC | 22/22 (100) |
| ST3 (MMP11) | 10/15 (66.7) |
| SPARC | 22/22 (100) |
| VEGFA | 21/21 (100) |
| CD31 | 22/22 (100) |
| CD34 | 22/22 (100) |
| FVIII | 22/22 (100) |
 | Table III.GLUT-1 immunoreactivity in vascular
lesions. |
Table III.
GLUT-1 immunoreactivity in vascular
lesions.
| GLUT-1 (%) |
|---|
| Vascular
malformations | 0/135 (0) |
| Hemangiomas | 101/124
(81.5)a |
| Angiofibromas | 0/22 (0) |
We also evaluated CD31, CD34 and FVIII, which
highlighted the vascular endothelium in all cases. CD31 and FVIII
were absent in stromal cells, but CD34 showed a weak positivity in
80% of the stromal cells. VEGFA and VEGFR1 were positive in the
endothelial cells in all cases, whereas stromal cells showed a weak
expression of both markers in 79% of the cases (data not
shown).
Northern blotting was performed to analyze the mRNA
for ST3/MMP11, which was expressed in all tumor samples, showing
increased levels as compared to normal turbinates (0.68±0.36 vs.
0.01±0.006) and resulting in significant distribution of these mRNA
values (p<0.001). Representative autoradiographs from Northern
blot analysis of ST3 are shown in Fig.
2.
Discussion
To better characterize the endothelial component of
JNAs, our objective in the present study was to determine
endothelial proliferation and differentiation markers that have not
been previously analyzed in this rare tumor. As it has been
suggested that the irregular vascular basement membrane described
in JNAs and tumors may possibly result from tissue remodeling
(35), we also analyzed the
biomarkers of remodeling.
Our findings of positive endoglin and Fli-1 staining
in the vessels of the cases analyzed here highlight the endothelial
differentiation as well as the hyper-proliferative state of
angiogenesis in JNAs. Although VEGFC acts primarily as a
lymphangiogenic factor, it may also promote the formation of blood
vessels (36).
The finding that JNA vessels were devoid of the
expression of lymphatic endothelial cell specific markers
(podoplanin and VEGFR3) underscores their blood endothelial cell
characteristic, without expressing lymphatic competence. Lack of
GLUT-1 discriminated JNAs from hemangiomas, which is interesting in
the context of the suggestion that JNAs might represent vascular
malformations (2,3).
Higher levels of ST3 mRNA were found in JNA vessels
as compared to inferior nasal turbinate specimens. Although several
MMPs have been described in JNAs (37), there have been no reports of ST3
expression in this particular type of tumor. ST3 differs from other
MMPs, since its mature form is incapable of cleaving type I and III
collagens, the major components of the stromal and vascular ECM in
JNAs (7). On the contrary, ST3
exhibits a collagenolytic function against the native α3 chain of
collagen VI (38). Prominent
collagen-type VI expression has been previously described in JNA
vessels, possibly exerting growth stimulatory effects on
endothelial cells (6,7).
Several studies reviewed by Clark and Sage (30) indicated that a stressed
microenvironment increases the expression of SPARC, reflecting the
loss of normal tissue homeostasis. The abundance of SPARC in the
late stages of tumor progression and invasion may represent a
failed attempt to restore tissue homeostasis within the tumor
microenvironment.
According to Chlenski et al (39), SPARC has antiangiogenic properties
and is capable of suppressing the activity of VEGF by directly
binding to this ligand through a negative regulatory feedback
mechanism, as VEGF-induced SPARC (40). Alternatively, SPARC enhances tumor
stroma formation, stimulating the production and secretion of
several extracellular matrix proteins, including collagen type I,
thus favoring the increase of the fibrous component observed during
JNA maturation (41). Our results
suggest a role for ST3 and SPARC in altering extracellular matrix
properties during angiogenesis in JNAs.
Of note, ST3 was reported to be induced by TGFβ
(42), and a reciprocal regulatory
loop has been demonstrated for SPARC and TGFβ, since SPARC was
shown to induce TGFβ and vice versa. Endoglin is a type III/TGFβ1
receptor also up-regulated by TGFβ stimulation (23), and TGFβ type II receptor gene
transcription is activated by Fli-1 (21). TGFβ was previously reported in both
the stromal and endothelial cells of JNAs (12,15,16).
Taken together, our data emphasize the potential role of TGFβ1 in
the pathogenesis of JNA.
Acknowledgements
This study was supported by CNPq and
FAPESP. We thank Dr Waldir Carreirão Neto for help with the
collection of samples and the clinical characteristics of the
patients and Dr J.P. Plese from the Neurology Department (FM, USP)
for the careful review of the manuscript.
References
|
1.
|
Coutinho-Camillo CM, Brentani MM and Nagai
MA: Genetic alterations in juvenile nasopharyngeal angiofibromas.
Head Neck. 30:390–400. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Beham A, Beham-Schmid C, Regauer S, et al:
Nasopharyngeal angiofibroma: true neoplasm or vascular
malformation? Adv Anat Pathol. 7:36–46. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Schick B and Urbschat S: New aspects of
pathogenesis of juvenile angiofibroma. Hosp Med. 65:269–273. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Eivazi B, Ardelean M, Bäumler W, et al:
Update on hemangiomas and vascular malformations of the head and
neck. Eur Arch Otorhinolaryngol. 266:187–197. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Starlinger V, Wendler O, Gramann M, et al:
Laminin expression in juvenile angiofibroma indicates vessel's
early developmental stage. Acta Otolaryngol. 127:1310–1315.
2007.PubMed/NCBI
|
|
6.
|
Gramann M, Wendler O, Haeberle L and
Schick B: Prominent collagen type VI expression in juvenile
angiofibromas. Histochem Cell Biol. 131:155–164. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Gramann M, Wendler O, Haeberle L and
Schick B: Expression of collagen types I, II and III in juvenile
angiofibromas. Cells Tissues Organs. 189:403–409. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Enjolras O, Wassef M and Chapot R:
Introduction: ISSVA Classification In: Color Atlas of Vascular
Tumors and Vascular Malformations. Cambridge University Press; New
York: pp. 3–11. 2007
|
|
9.
|
Tamm E, Jungkunz W, Marsch WC and
Lütjen-Drecoll E: Increase in types IV and VI collagen in cherry
haemangiomas. Arch Dermatol Res. 284:275–282. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Pusztaszeri MP, Seelentag W and Bosman FT:
Immunohistochemical expression of endothelial markers CD31, CD34,
von Willebrand factor, and Fli-1 in normal human tissues. J
Histochem Cytochem. 54:385–395. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Schiff M, Gonzalez AM, Ong M, et al:
Juvenile nasopharyngeal angiofibroma contain an angiogenic growth
factor: basic FGF. Laryngoscope. 102:940–945. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Dillard DG, Cohen C, Muller S, et al:
Immunolocalization of activated transforming growth factor beta1 in
juvenile nasopharyngeal angiofibroma. Arch Otolaryngol Head Neck
Surg. 126:723–725. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Zhang PJ, Weber R, Liang HH, et al: Growth
factors and receptors in juvenile nasopharyngeal angiofibroma and
nasal polyps: an immunohistochemical study. Arch Pathol Lab Med.
127:1480–1484. 2003.PubMed/NCBI
|
|
14.
|
Brieger J, Wierzbicka M, Sokolov M, et al:
Vessel density, proliferation, and immunolocalization of vascular
endothelial growth factor in juvenile nasopharyngeal angiofibromas.
Arch Otolaryngol Head Neck Surg. 130:727–731. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Saylam G, Yücel OT, Sungur A, et al:
Proliferation, angiogenesis and hormonal markers in juvenile
nasopharyngeal angiofibroma. Int J Pediatr Otorhinolaryngol.
70:227–234. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Schuon R, Brieger J, Heinrich UR, et al:
Immunohistochemical analysis of growth mechanisms in juvenile
nasopharyngeal angiofibroma. Eur Arch Otorhinolaryngol.
264:389–394. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Ponti G, Losi L, Pellacani G, et al: Wnt
pathway, angiogenetic and hormonal markers in sporadic and familial
adenomatous polyposis-associated juvenile nasopharyngeal
angiofibromas (JNA). Appl Immunohistochem Mol Morphol. 16:173–178.
2008. View Article : Google Scholar
|
|
18.
|
Montag AG, Tretiakova M and Richardson M:
Steroid hormone receptor expression in nasopharyngeal
angiofibromas. Consistent expression of estrogen receptor beta. Am
J Clin Pathol. 125:832–837. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Pauli J, Gundelach R, Vanelli-Rees A, et
al: Juvenile nasopharyngeal angiofibroma: an immunohistochemical
characterisation of the stromal cell. Pathology. 40:396–400. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Nagy JA, Chang SH, Dvorak AM and Dvorak
HF: Why are tumour blood vessels abnormal and why is it important
to know? Br J Cancer. 100:865–869. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Truong AH and Ben-David Y: The role of
Fli-1 in normal cell function and malignant transformation.
Oncogene. 19:6482–6489. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Folpe AL, Chand EM, Goldblum JR and Weiss
SW: Expression of Fli-1, a nuclear transcription factor,
distinguishes vascular neoplasms from potential mimics. Am J Surg
Pathol. 25:1061–1066. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Dallas NA, Samuel S, Xia L, Fan F, Gray
MJ, Lim SJ and Ellis LM: Endoglin (CD105): a marker of tumor
vasculature and potential target for therapy. Clin Cancer Res.
14:1931–1937. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Breiteneder-Geleff S, Soleiman A, Kowalski
H, et al: Angiosarcomas express mixed endothelial phenotypes of
blood and lymphatic capillaries: podoplanin as a specific marker
for lymphatic endothelium. Am J Pathol. 154:385–394. 1999.
View Article : Google Scholar
|
|
25.
|
Folpe AL, Veikkola T, Valtola R and Weiss
SW: Vascular endothelial growth factor receptor-3 (VEGFR-3): a
marker of vascular tumors with presumed lymphatic differentiation,
including Kaposi's sarcoma, kaposiform and Dabska-type
hemangioendotheliomas, and a subset of angiosarcomas. Mod Pathol.
13:180–185. 2000.PubMed/NCBI
|
|
26.
|
Harik SI, Hall AK, Richey P, et al:
Ontogeny of the erythroid/HepG2-type glucose transporter (GLUT-1)
in the rat nervous system. Brain Res Dev Brain Res. 72:41–49. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
27.
|
Gillies RJ, Robey I and Gatenby RA: Causes
and consequences of increased glucose metabolism of cancers. J Nucl
Med. 49:S24–S42. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
28.
|
North PE, Waner M, Mizeracki A, et al:
GLUT-1: a newly discovered immunohistochemical marker for juvenile
hemangiomas. Hum Pathol. 31:11–22. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
29.
|
Aird WC: Molecular heterogeneity of tumor
endothelium. Cell Tissue Res. 335:271–281. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
30.
|
Clark CJ and Sage EH: A prototypic
matricellular protein in the tumor microenvironment – where there's
SPARC, there's fire. J Cell Biochem. 104:721–732. 2008.PubMed/NCBI
|
|
31.
|
Rio MC: From a unique cell to metastasis
is a long way to go: clues to stromelysin-3 participation.
Biochimie. 87:299–306. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
32.
|
Podhajcer OL, Benedetti L, Girotti MR,
Prada F, Salvatierra E and Llera AS: The role of the matricellular
protein SPARC in the dynamic interaction between the tumor and the
host. Cancer Metastasis Rev. 27:523–537. 2008. View Article : Google Scholar
|
|
33.
|
Krstulja M, Car A, Bonifacić D, Braut T
and Kujundzić M: Nasopharyngeal angiofibroma with intracellular
accumulation of SPARC – a hypothesis (SPARC in nasopharyngeal
angiofibroma). Med Hypotheses. 70:600–604. 2008.PubMed/NCBI
|
|
34.
|
Mangone FR, Brentani MM, Nonogaki S, et
al: Overexpression of Fos-related antigen-1 in head and neck
squamous cell carcinoma. Int J Exp Pathol. 86:205–212. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
35.
|
Baluk P, Morikawa S, Haskell A, Mancuso M
and McDonald DM: Abnormalities of basement membrane on blood
vessels and endothelial sprouts in tumors. Am J Pathol.
163:1801–1815. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
36.
|
Cao R, Eriksson A, Kubo H, Alitalo K, Cao
Y and Thyberg J: Comparative evaluation of FGF-2-, VEGF-A-, and
VEGF-C-induced angiogenesis, lymphangiogenesis, vascular
fenestrations, and permeability. Circ Res. 94:664–670. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
37.
|
Duerr S, Wendler O, Aigner T, Karosi S and
Schick B: Metalloproteinases in juvenile angiofibroma – a collagen
rich tumor. Hum Pathol. 39:259–268. 2008.
|
|
38.
|
Motrescu ER, Blaise S, Etique N, et al:
Matrix metalloproteinase-11/stromelysin-3 exhibits collagenolytic
function against collagen VI under normal and malignant conditions.
Oncogene. 27:6347–6355. 2008. View Article : Google Scholar
|
|
39.
|
Chlenski A, Liu S, Guerrero LJ, et al:
SPARC expression is associated with impaired tumor growth,
inhibited angiogenesis and changes in the extracellular matrix. Int
J Cancer. 118:310–316. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
40.
|
Kato Y, Lewalle JM, Baba Y, et al:
Induction of SPARC by VEGF in human vascular endothelial cells.
Biochem Biophys Res Commun. 287:422–426. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
41.
|
Sennes LU, Fortes FS, Butugan O, Saldiva
PH and Bernardi FC: Tissue maturation correlating to clinical
manifestations in juvenile angiofibroma. Ann Otol Rhinol Laryngol.
114:705–708. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
42.
|
Delany AM and Canalis E: The
metastasis-associated metalloproteinase stromelysin-3 is induced by
transforming growth factor-beta in osteoblasts and fibroblasts.
Endocrinology. 142:1561–1566. 2001.PubMed/NCBI
|