Introduction
Langerhans cell histiocytosis (LCH) in the lumbar
spine of adults is uncommon (1,2). A
variety of treatment modalities have been reported for the
management of LCH of the spine, including conservative treatments,
systemic chemotherapy, curettage (with or without bone grafting),
internal fixation and fusion, percutaneous vertebroplasty (PVP),
corticosteroid injection into the lesion and radiotherapy (3). Although the clinical results are
largely satisfactory, there is not a defined therapeutic algorithm.
In the present study, the case of a 51-year-old male with LCH of
the fourth lumar vertebra (L4) is reported.
Case report
The 51-year-old male patient exhibited a 10-day
history of low back pain, limited waist motion and right lower limb
numbness. The patient reported no pain at other sites, exhibited no
fever or night sweats and was unable to recall any recent injury.
The patient’s past medical history was unremarkable for trauma or
other bone diseases. A physical examination demonstrated localized
tenderness and percussion pain over the L4 spinous process,
restricted waist motion and numbness of the right leg. Laboratory
tests, including full blood cell count, serum electrolytes, renal
and liver function tests, erythrocyte sedimentation rate (ESR) and
C-reactive protein (CRP), did not reveal any abnormalities. An
X-ray revealed that the lesion was limited to the left lateral mass
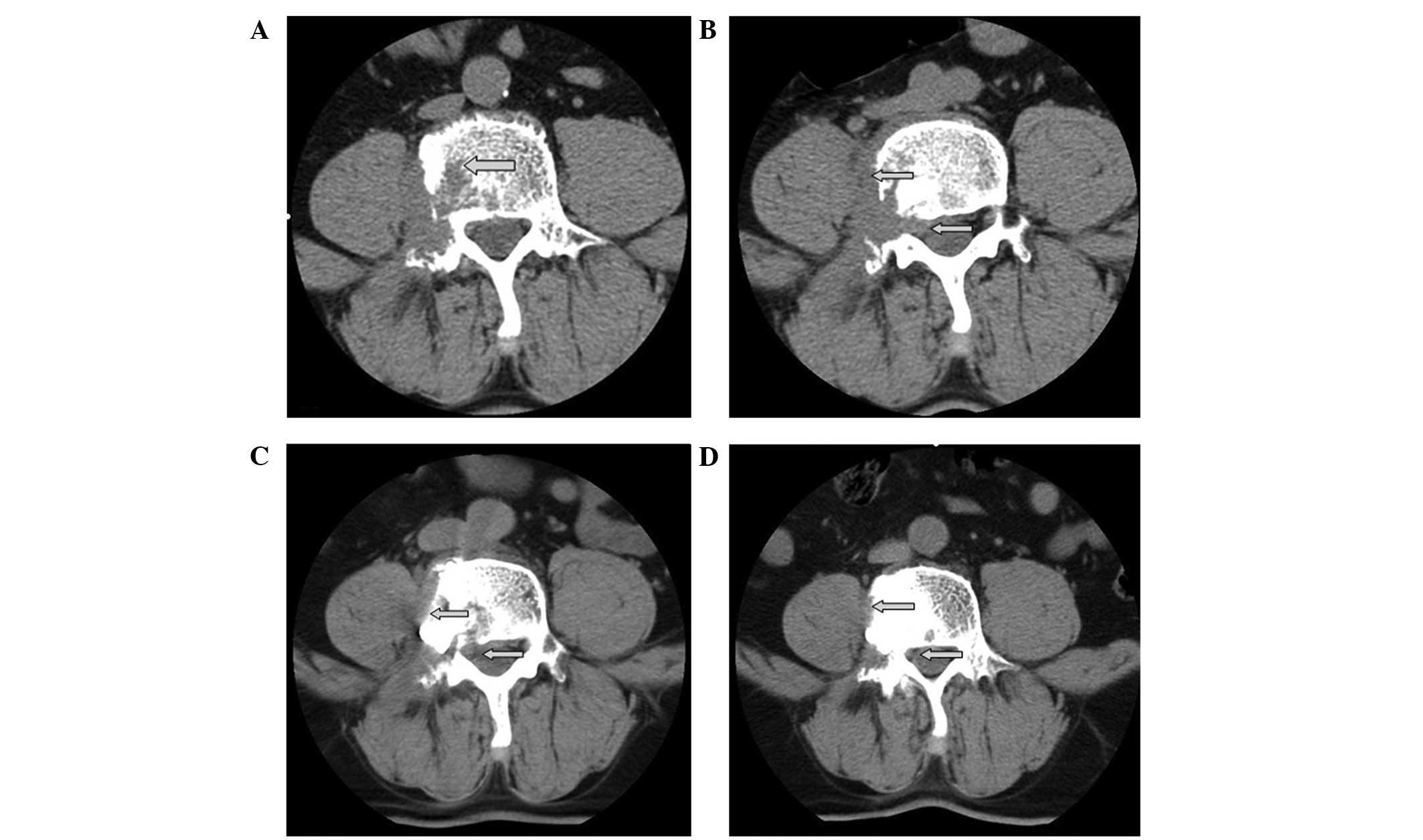
of the atlas, causing a potential instability (Fig. 1A and B). Computed tomography (CT)
revealed an osteolytic lesion in the right lateral mass of the L4
and accessories, accompanied by a paravertebral and intraspinal
soft tissue extension (Fig. 2A and
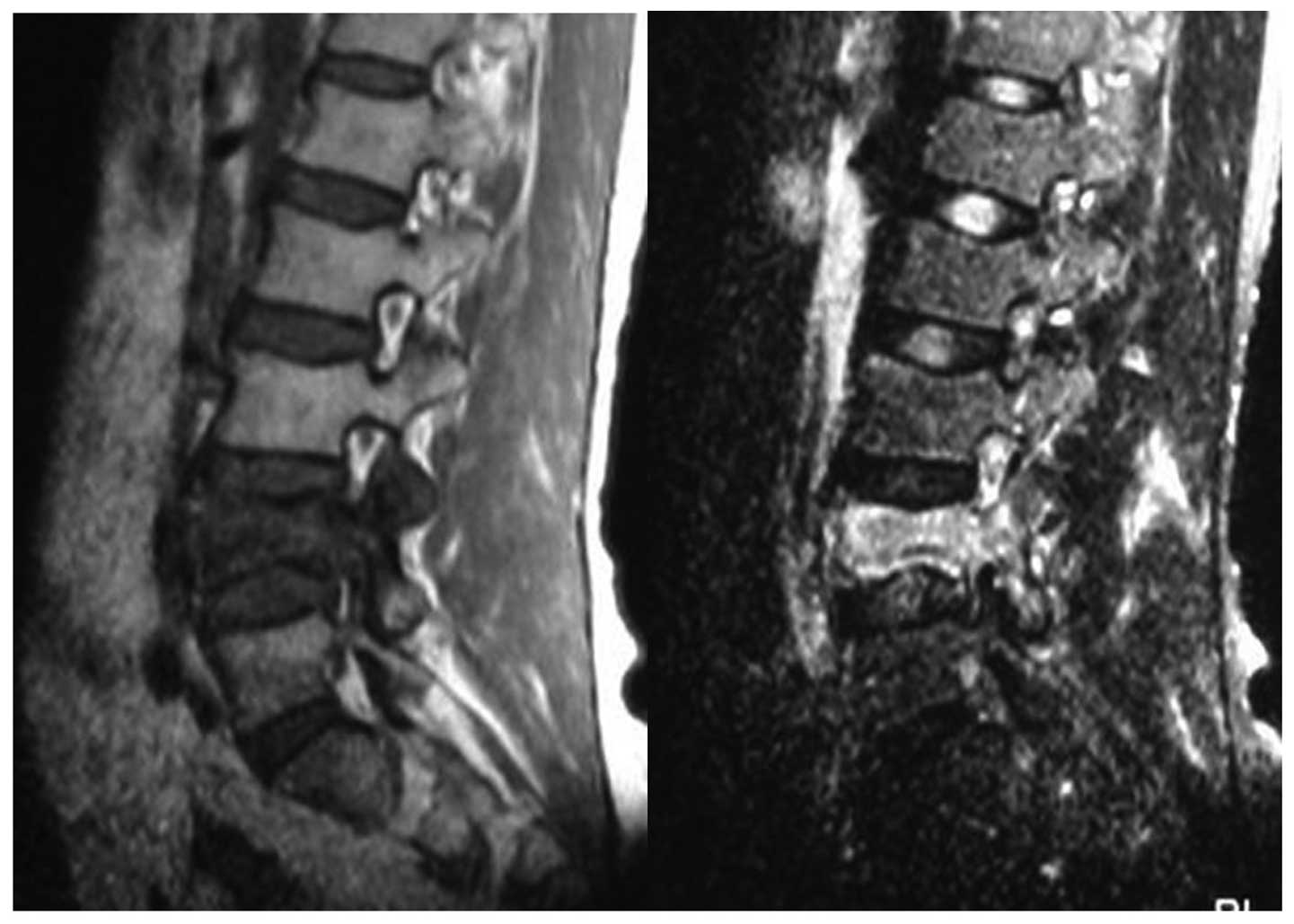
B). Magnetic resonance imaging (MRI) revealed osteolytic
destruction of the vertebral body associated with a mild
compression fracture that exhibited hypointensity on T1-weighted
(T1-W) images and hyperintensity on T2-weighted (T2-W) images
(Fig. 3). On the basis of the
radiological features of the lesion, there was a high possibility
that the patient had a neoplastic lesion. However, the radiological
features of the lesion were not sufficient to establish the
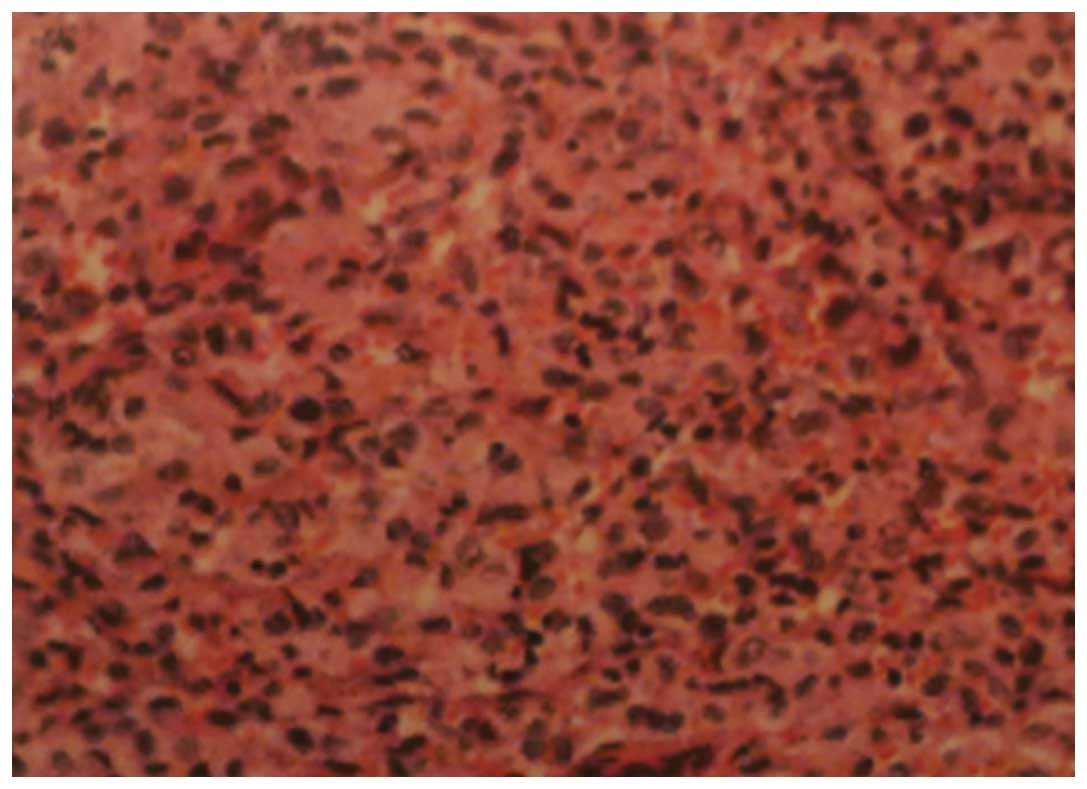
diagnosis of LCH with certainty. A C-arm X-ray machine-guided
needle biopsy of the vertebral body was performed and the
histopathological diagnosis was LCH. Immunohistochemical staining
was positive for CD1a and S-100 (Fig.
4). Further diagnostic evaluation included a bone scan, CT of
the lungs, pituitary hormonal evaluation and brain CT and abdominal
ultrasound evaluation. No other LCH infiltration was identified in
the patient and the patient was treated as suffering from a
single-system and single-site disease.
The patient underwent PVP (Stryker, Inc., Meyzieu,
France) under local anesthesia in the prone position with the belly
suspended in midair, under C-arm imaging guidance (Fig. 5). The amount of bone cement used to
fill in the L4 was 3.6 ml. The blood loss during surgery was 5 ml.
The spread of the cement was ideal with the exception of a small
amount of paravertebral leakage of cement (Fig. 2C) which did not cause any symptoms.
No complications were observed during the surgery or follow-up.
After lying in bed for 6 h, the patient was able to sit freely and
24 h postoperatively, the patient was allowed to walk freely.
Following the procedure, the low back pain was resolved completely
and the patient’s neurological symptoms were rapidly alleviated and
then gradually continued to be alleviated. The patient required the
use of a weak opioid prior to the PVP but did not receive an
analgesic afterwards. Notably, CT revealed a significant decrease
in the paravertebral and intraspinal soft tissue extension 5 days
after the PVP (Fig. 2C).
The patient received chemotherapy following PVP. The
chemotherapy regime was 100 mg etoposide (days 1–3) and 60, 40 and
20 mg prednisone (days 1–7, 8–14 and 15–21, respectively) for 3
cycles. There were no serious side-effects of the chemotherapy. CT
revealed that the paravertebral and intraspinal soft tissue
extension disappeared after 3 cycles (Fig. 2D). The height of the vertebral body
remained stable without further collapse and lumbar kyphosis did
not occur. There was no recurrence and no other complaints over a
6-month follow-up period (Fig. 1C and
D).
Discussion
LCH is a rare disease associated with the
proliferation of Langerhans cells (1,2). The
incidence rate of LCH is approximately 1:1,500,000 (3). Although LCH mostly occurs during
childhood, it may affect patients of any age from infants to
elderly individuals. LCH is characterized by the clonal
accumulation and/or proliferation of specific dendritic cells that
resemble the normal epidermal Langerhans cell and are capable of
infiltrating almost any organ (4).
Although the cell of origin in this disease has now been defined,
the exact etiology of LCH remains unknown. It is considered to be a
neoplasm or infectious disease caused by a disorder during the
immaturity of the immune system (5). LCH has 3 classic clinical syndromes
that are considered to be variations of the same disease: i)
eosinophilic granuloma; ii) Hand-Schüller-Christian disease; and
iii) Letterer-Siwe disease (5).
The most frequent sites of the bony lesions of LCH
are the skull, femur, mandible, pelvis and spine (3,6). LCH
in the spine is reported to occur in between 6.5 and 25% of cases
(7), with the most frequent site
being the thoracic vertebrae (54%), followed by the lumbar (35%)
and cervical (11%) vertebrae (5).
Soft tissue extension has been reported in 50% of cases (6) and posterior arch extension in 65%
(8).
The characteristic symptoms of LCH of the lumbar
spine of adults are back pain, restricted range of motion and
neurological symptoms, although neurological deficits are uncommon
(9). Pain is explained by the
onset of a collapse of the vertebral body with osteolysis.
Neurological symptoms may be caused by the soft tissue extension.
Spinal LCH is easy to misdiagnose as malignant tumors, lymphoma or
tuberculosis. LCH should be included in the differential diagnosis
of osteolytic and osteoblastic vertebral lesions. Although
radiological studies and clinical characteristics may indicate the
disease, these alone cannot result in a definitive diagnosis.
Histopathological confirmation is essential. The histopathological
diagnostic criteria require the expression of CD1a and S-100
antigen on the lesion cell surface for a definitive diagnosis
(10).
There are various treatment modalities for LCH of
the spine reported in the literature. Conservative measures are
appropriate for mild isolated involvement of the spine without a
risk of neurological damage or spinal instability, including simple
observation, prolonged immobilization, nonsteroidal
anti-inflammatory drugs or casting with or without initial bed rest
(11–13). Open surgery should be reserved for
patients with severe mechanical instability or deformity and/or
neurological deficits caused by the compression (8,11).
Due to the potential for secondary malignancy and vertebral
growth-plate damage in the skeletally immature patients,
radiotherapy appears to be overtreatment in isolated osseous cases
(7,14,15).
In cases where the patient is a child, radiotherapy may lead to the
early closure of vertebral growth (16). Chemotherapy is suggested for
treating disseminated LCH, such as multiple bone lesions or
multi-system disease (3). It has
been reported that chemotherapy is safe and effective for the
management of LCH of the spine in patients with soft tissue
extension (6) and may
significantly reduce recurrence rates (17). Although these treatments were
reported to produce satisfactory results with a recurrence rate of
less than 20%, there has been no evidence suggesting that any one
treatment is more advantageous than another (18–22).
PVP was developed by Galibert et al(23) and appears to offer an alternative
to the preceeding treatments. The minimally invasive vertebroplasty
apparatus consists of an introducing cannula, operative cannula,
Kirschner guidewires, manual drill and reconstituted acrylic
polymethylmethacrylate which is used to fill the vertebra via a
transpedicular approach under C-arm imaging guidance. PVP is able
to effectively relieve pain and strengthen the vertebra weakened by
the disease, allowing spinal stabilization. PVP has been generally
accepted as a safe and effective treatment option for patients with
vertebral haemangioma (23),
osteoporotic vertebral compression fractures (24) and spinal tumors (25). PVP is a new technique with a number
of advantages; it is minimally invasive and does not require
implants or open surgery and patients may recover rapidly. PVP is
capable of relieving pain quickly and stabilizing the fracture by
enhancing the rigidity and intensity of vertebra to allow early
weight-bearing movements.
Only 3 cases concerning the treatment of LCH in the
spine with PVP have been reported previously in the literature. Tan
et al(26) performed PVP in
a child with cervical LCH and the patient recovered well. Cardon
et al used PVP in an adult with lumbar spine LCH and
reported a good clinical result (27). Kevane et al performed PVP in
an adult lumbar spine LCH case with marked symptomatic relief
(28).
Although the mechanism of pain relief following PVP
remains unclear, the majority of studies speculate that it may be
due to: i) the heat generated during cement consolidation
destroying the nerve endings in the surrounding tissues and killing
tumor cells (29); ii) the
injected bone cement improving the strength of the vertebral bodies
and the stability of the spine, redistributing the mechanical
forces, reducing the irritation to vertebral nerves (30,31);
and iii) the cytotoxicity of the polymethylmethacrylate in the
cement destroying nerve terminals and killing tumor cells (32–35).
In conclusion, when conservative treatments are not
feasible and open surgical treatment is an overtreatment, PVP is a
suitable alternative for treating patients with the progressive
lesions of LCH in the spine and the potential risk of progressive
vertebral compression fractures and neural compression, and may be
new indicators of PVP. PVP relieves pain quickly and stabilizes the
fracture of the vertebra with minimal invasion. Patients are able
to recover rapidly and make early weight-bearing movements.
Combination chemotherapy for treating the paravertebral and
intraspinal soft tissue extension is safe and effective and may
also reduce recurrence. Although the short-term results of PVP for
LCH of the spine are promising, long-term follow-ups are essential
for demonstrating the efficacy of PVP in cases of spinal LCH.
References
|
1
|
Aster J and Kumar V: White cells, lymph
nodes, spleen, and thymus. Robbins Pathologic Basis of Disease.
Cotran RS, Kumar V, Collins T and Robbins SL: Saunders;
Philadelphia, PA: pp. 644–686. 1999
|
|
2
|
Cheyne C: Histiocytosis X. J Bone Joint
Surg Br. 53:366–382. 1971.PubMed/NCBI
|
|
3
|
Zhong WQ, Jiang L, Ma QJ, Liu ZJ, Liu XG,
Wei F, Yuan HS and Dang GT: Langerhans cell histiocytosis of the
atlas in an adult. Eur Spine J. 19:19–22. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Weitzman S and Egeler RM: Histiocytic
Disorders of Children and Adults: Basic Science, Clinical Features
and Therapy. Cambridge University Press; Cambridge: 2005,
View Article : Google Scholar
|
|
5
|
Azouz EM, Saigal G, Rodriguez MM and Podda
A: Langerhans’ cell histiocytosis: pathology, imaging and treatment
of skeletal involvement. Pediatr Radiol. 35:103–115. 2005.
|
|
6
|
Peng XS, Pan T, Chen LY, Huang G and Wang
J: Langerhans’ cell histiocytosis of the spine in children with
soft tissue extension and chemotherapy. Int Orthop. 33:731–736.
2009.
|
|
7
|
Garg S, Mehta S and Dormans JP: Langerhans
cell histiocytosis of the spine in children. Long-term follow-up. J
Bone Joint Surg Am. 86-A:1740–1750. 2004.PubMed/NCBI
|
|
8
|
Liu XG, Zhong WQ, Liu ZJ, Yuan HS, Jiang
L, Ma QJ, Wei F and Dang GT: Diagnosis and treatment of Langerhans
cell histiocytosis of the cervical spine. Zhongguo Ji Zhu Ji Sui Za
Zhi. 19:431–436. 2009.(In Chinese).
|
|
9
|
Tanaka N, Fujimoto Y, Okuda T, Nakanishi
K, Sumida T, Manabe H and Ochi M: Langerhans cell histiocytosis of
the atlas. A report of three cases. J Bone Joint Surg Am.
87:2313–2317. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Aricó M, Girschikofsky M, Géneréau T, et
al: Langerhans cell histiocytosis in adults. Report from the
International Registry of the Histiocyte Society. Eur J Cancer.
39:2341–2348. 2003.PubMed/NCBI
|
|
11
|
Bertram C, Madert J and Eggers C:
Eosinophilic granuloma of the cervical spine. Spine (Phila Pa
1976). 27:1408–1413. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ngu BB, Khanna AJ, Pak SS, et al:
Eosinophilic granuloma of the atlas presenting as torticollis in a
child. Spine (Phila PA 1976). 29:E98–E100. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yeom JS, Lee CK, Shin HY, Lee CS, Han CS
and Chang H: Langerhans’ cell histiocytosis of the spine. Analysis
of twenty-three cases. Spine (Phila PA 1976). 24:1740–1749.
1999.
|
|
14
|
Levy El, Scarrow A, Hamilton RC, Wollman
MR, Fitz C and Pollack IF: Medical management of eosinophilic
granuloma of the cervical spine. Pediatr Neurosurg. 31:159–162.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Floman Y, Bar-On E, Mosheiff R, Mirovsky
Y, Robin GC and Ramu N: Eosinophilic granuloma of the spine. J
Pediatr Orthop B. 6:260–265. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Greenberger JS, Crocker AC, Vawter G,
Jaffe N and Cassady JR: Results of treatment of 127 patients with
systemic histiocytosis. Medicine (Baltimore). 60:311–338. 1981.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
von Stebut E, Schadmand-Fischer S,
Bräuninger W, Kreft A, Doberauer C and Steinbrink K: Successful
treatment of adult multisystemic Langerhans cell histiocytosis with
psoralen-UV-A, prednisolone, mercaptopurine, and vinblastine. Arch
Dermatol. 144:649–653. 2008.PubMed/NCBI
|
|
18
|
Levine SE, Dormans JP, Meyer JS and
Corcoran TA: Langerhans’ cell histiocytosis of the spine in
children. Clin Orthop Relat Res. 323:288–293. 1996.
|
|
19
|
Ladisch S and Gadner H: Treatment of
Langerhans cell histiocytosis - evolution and current approaches.
Br J Cancer Suppl. 23:S41–S46. 1994.PubMed/NCBI
|
|
20
|
McLelland J, Broadbent V, Yeomans E,
Malone M and Pritchard J: Langerhans cell histiocytosis: the case
for conservative treatment. Arch Dis Child. 65:301–303. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sessa S, Sommelet D, Lascombes P and
Prévot J: Treatment of Langerhans-cell histiocytosis in children:
experience at the Children’s Hospital of Nancy. J Bone Joint Surg
Am. 76:1513–1525. 1994.
|
|
22
|
Womer RB, Raney RB and D’Angio GJ: Healing
rates of treated and untreated bone lesions in histiocytosis X.
Pediatrics. 76:286–288. 1985.PubMed/NCBI
|
|
23
|
Galibert P, Deramond H, Rosat P and Le
Gars D: Preliminary note on the treatment of vertebral angioma by
percutaneous acrylic vertebroplasty. Neurochirurgie. 33:166–168.
1987.(In French).
|
|
24
|
Kobayashi K, Shimoyama K, Nakamura K and
Murata K: Percutaneous vertebroplasty immediately relieves pain of
osteoporotic vertebral compression fractures and prevents prolonged
immobilization of patients. Eur Radiol. 15:360–367. 2005.
View Article : Google Scholar
|
|
25
|
Shimony JS, Gilula LA, Zeller AJ and Brown
DB: Percutaneous vertebroplasty for malignant compression fractures
with epidural involvement. Radiology. 232:846–853. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Tan HQ, Li MH, Wu CG, Gu YF, Zhang H and
Fang C: Percutaneous vertebroplasty for eosinophilic granuloma of
the cervical spine in a child. Pediatr Radiol. 37:1053–1057. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Cardon T, Hachulla E, Flipo RM, et al:
Percutaneous vertebroplasty with acrylic cement in the treatment of
a Langerhans cell vertebral histiocytosis. Clin Rheumatol.
13:518–521. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kevane B, Ryder DQ and Gilligan O:
Percutaneous vertebroplasty in osteoporosis, myeloma and
Langerhans’ cell histiocytosis. Ir Med J. 102:212–215.
2009.PubMed/NCBI
|
|
29
|
Coumans JV, Reinhardt MK and Lieberman IH:
Kyphoplasty for vertebral compression fractures: 1-year clinical
outcomes from a prospective study. J Neurosurg. 99(1 Suppl): 44–50.
2003.PubMed/NCBI
|
|
30
|
Belkoff SM, Mathis JM, Erbe EM and Fenton
DC: Biomechanical evalution of a new bone cement for use in
vertebroplasty. Spine (Phila Pa 1976). 25:1061–1064. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Cotten A, Boutry N, Cortet B, et al:
Percutaneous vertebroplasty: state of the art. Radiographics.
18:311–320. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Cotten A, Dewatre F, Cortet B, et al:
Percutaneous vertebroplasty for osteolytic metastases and myeloma:
effects of the percentage of lesion filling and the leakage of
methyl methacrylate at clinical follow-up. Radiol. 200:525–530.
1996. View Article : Google Scholar
|
|
33
|
Weill A, Chiras J, Simon JM, et al: Spinal
metastases: indications for and results of percutaneous injection
of acrylic surgical cement. Radiology. 199:241–247. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Mathis JM, Barr JD, Belkoff SM, et al:
Percutaneous vertebroplasty: a developing standard of care for
vertebral compression fractures. AJNR Am J Neuroradiol. 22:373–81.
2001.PubMed/NCBI
|
|
35
|
Radin EL, Rubin CT, Thrasher EL, et al:
Changes in the bone-cement interface after total hip replacement:
an in vivo animal study. J Bone Joint Surg Am. 64:1188–1200.
1982.PubMed/NCBI
|