Introduction
Pulmonary contusion occurs when an external force is
exerted on lung tissues, which is usually associated with a closed
chest injury frequently resulting from a traffic accident, free
fall from a height or blunt trauma. The strong force on the chest
wall reduces the thoracic volume and consequently increases
intrathoracic pressure, which compresses lung tissues, leading to
pulmonary parenchymal hemorrhage and edema, pulmonary capillary
injuries, interstitial and alveolar effusion, interstitial edema
and the infiltration of inflammatory cells. These pathological
changes result in decreased ventilation and gas exchange, severe
ventilation-perfusion imbalance, hypoxia and poor pulmonary
compliance. Pulmonary contusion is one of the major causes of acute
lung injury and acute respiratory distress syndrome and can
develops into systemic inflammatory response syndrome and multiple
organ dysfunction syndrome, resulting in a high incidence of
mortality. Recently, numerous theoretical and clinical studies on
pulmonary contusion have been carried out, particularly concerning
the role of inflammatory cytokines. Following contusion, lung
tissues are exposed to a potent inflammatory response in which
alveolar epithelial and endothelial cells become extensively
degenerated and necrotic, compromising the gas exchange in alveoli.
This inflammatory pathogenesis can be accelerated by inflammatory
cytokines into a response cascade. Moreover, cytokines are believed
to play their roles by interacting through a complex network.
The evaluation of trauma severity is critical for
the diagnosis, treatment and prediction of prognosis of the trauma
patient. Based on the Abbreviated Injury Scale (AIS), the Injury
Severity Score (ISS) is the most commonly used hospital trauma
scoring system and plays an important role in trauma rescue. ISS
includes the comprehensive evaluation of multiple traumas by a
general overview of anatomical injury and predicts the probability
of patient survival. However, this scoring system has its innate
limits in clinical practice. For example, for a single site of
multiple trauma, the maximum AIS (mAIS) alone does not reflect the
severity of the injury. In addition to ISS, a specific chest injury
scoring system is required for assessment of patients with multiple
trauma complicated by chest injury. Pape et al (4) proposed the Thoracic Trauma Severity
Score (TTS) for the early evaluation of chest injury. The primary
measures of TTS consist of the severity of chest and thoracic
injury, oxygenation index and patient age. The use of TTS, as a
newly emerging chest injury scoring system in clinical practice to
supplement other currently available scoring tools, should be
justified in further clinical studies.
In the present study, we examined the dynamic
changes in the serum levels of tumor necrosis factor (TNF)-α
interleukin (IL)-6 and IL-10 in patients suffering from closed
chest injuries and concomitant pulmonary contusions. Additionally,
changes in pro- and anti-inflammatory cytokines were assessed.
Differences in cytokine levels between patients with and without
pulmonary contusion sharing similar ISS were determined, and the
correlation of cytokine levels with trauma scores was analyzed. The
assay of cytokine levels in combination with TTS and ISS may be an
effective tool for evaluating the severity of injury in patients
suffering from closed chest injury and concomitant pulmonary
contusions. Justification of the use of TTS in clinical practice
for the estimation of chest injury as a supplementary measure to
the systemic trauma evaluation system was herein attempted.
Patients and methods
Patient characteristics
Patients suffering from multiple trauma (n=41) who
were hospitalized in our surgical unit between January 2007 and
January 2008 were studied. The patients included 33 males and 8
females, aged 20–85 years (mean 46.93±15.10). The cause of trauma
consisted of traffic accident (n=30), free fall from a height (n=6)
and heavy weight blunt injury (n=5). The inclusion criterion of
multiple trauma patients was ISS ≥16. Twenty-one patients were
afflicted with closed chest injury and pulmonary contusion, whereas
the remaining 20 patients were not complicated by pulmonary
contusion. The two groups did not differ significantly in ISS. The
general characteristics of the two groups are shown in Table I. No deaths occurred during
hospitalization. Healthy volunteers (n=15) were enrolled
simultaneously as controls, including 12 males and 3 females (mean
age 47.67±17.06 years; range 21–80).
 | Table I.General characteristics of the
patients with or without pulmonary contusion. |
Table I.
General characteristics of the
patients with or without pulmonary contusion.
| With contusion
(n=21) | Without contusion
(n=20) |
|---|
| Gender (M/F) | 16/5 | 17/3 |
| Age, mean (range), in
years | 45.62±17.74
(21–85) | 48.30±12.04
(20–73) |
| Inclusion
criteria | i) ISS ≥16; ii) Shows
patchy and obscure shadows on chest radiograph and CT scan within
24 h of trauma | i) ISS ≥16 |
| ISS (range) | 29.00±8.26
(17–50) | 29.95±7.89
(18–48) |
| TTS (range) | 9.76±2.79 (5–16) | 3.57±1.99 (1–7) |
| Cause of trauma | | |
| Traffic
accident | 13 | 17 |
| Free fall from
injury | 4 | 2 |
| Heavy weight
injury | 4 | 1 |
Sample collection and measurement
Venous blood samples (5 ml) were collected from all
of the post-traumatic patients on days 1, 2, 3, 5 and 7 following
trauma, whereas peripheral venous blood samples were also collected
from fasting control patients simultaneously. Blood samples were
separated at room temperature and stored at −20˚C for further batch
assay using an avidin-biotin complex ELISA kit as recommended by
the manufacturer.
Statistical analysis
Data were processed by using SPSS 13.0 statistical
analysis software. The quantitative data were expressed as the
means ± SD for the analysis of variance and correlation analysis.
P<0.05 was considered statistically significant, whereas
P<0.01 was highly significant.
Results
Statistical analyses showed that the serum levels of
TNF-α, IL-6 and IL-10 in patients with traumas complicated by
pulmonary contusion were significantly higher than those in
patients without pulmonary contusion and healthy control patients
on days 1, 2, 3, 5 and 7 after trauma (both P<0.01) (Table II).
 | Table II.Changes in the serum TNF-α, IL-6 and
IL-10 levels (mean ± SD) in the trauma patients. |
Table II.
Changes in the serum TNF-α, IL-6 and
IL-10 levels (mean ± SD) in the trauma patients.
| Post-trauma time
(days) | Group | TNF-α (pg/ml) | IL-6 (pg/ml) | IL-10 (pg/ml) |
|---|
| Control | 25.46±5.08 | 17.55±0.97 | 10.37±5.12 |
| 1 | With contusion |
130.16±38.12a,b |
102.28±31.50a,b |
95.06±29.86a,b |
| 1 | Without
contusion | 97.63±21.12 | 77.35±18.39 | 71.25±19.19 |
| 2 | With contusion |
113.77±33.85a,b |
117.18±34.18a,b |
108.86±30.98a,b |
| 2 | Without
contusion | 82.18±19.84 | 89.78±19.74 | 83.62±21.23 |
| 3 | With contusion |
98.26±38.95a,b |
89.44±25.25a,b |
84.12±24.00a,b |
| 3 | Without
contusion | 67.92±17.54 | 61.10±16.96 | 54.13±15.39 |
| 5 | With contusion |
76.00±24.18a,b |
73.53±32.49a,b |
66.59±18.95a,b |
| 5 | Without
contusion | 50.84±13.84 | 45.72±11.92 | 39.66±9.96 |
| 7 | With contusion |
55.95±16.94a,b |
48.39±14.40a,b |
40.31±10.84a,b |
| 7 | Without
contusion | 38.03±8.29 | 32.78±6.34 | 27.91±5.71 |
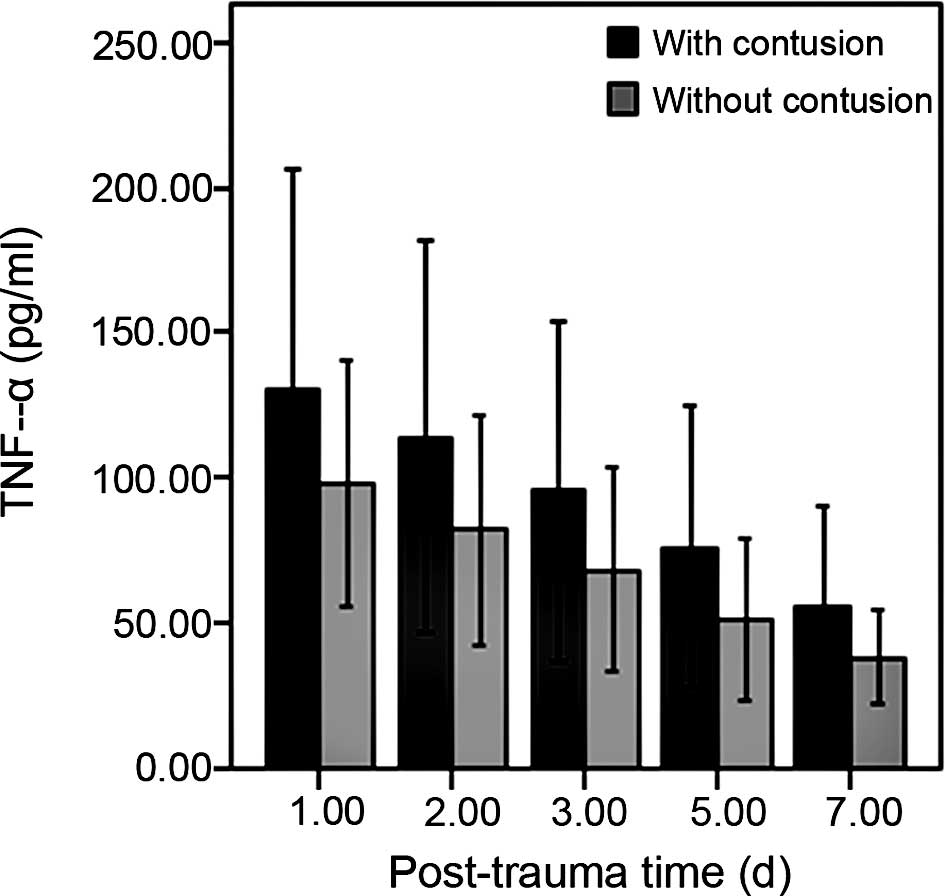
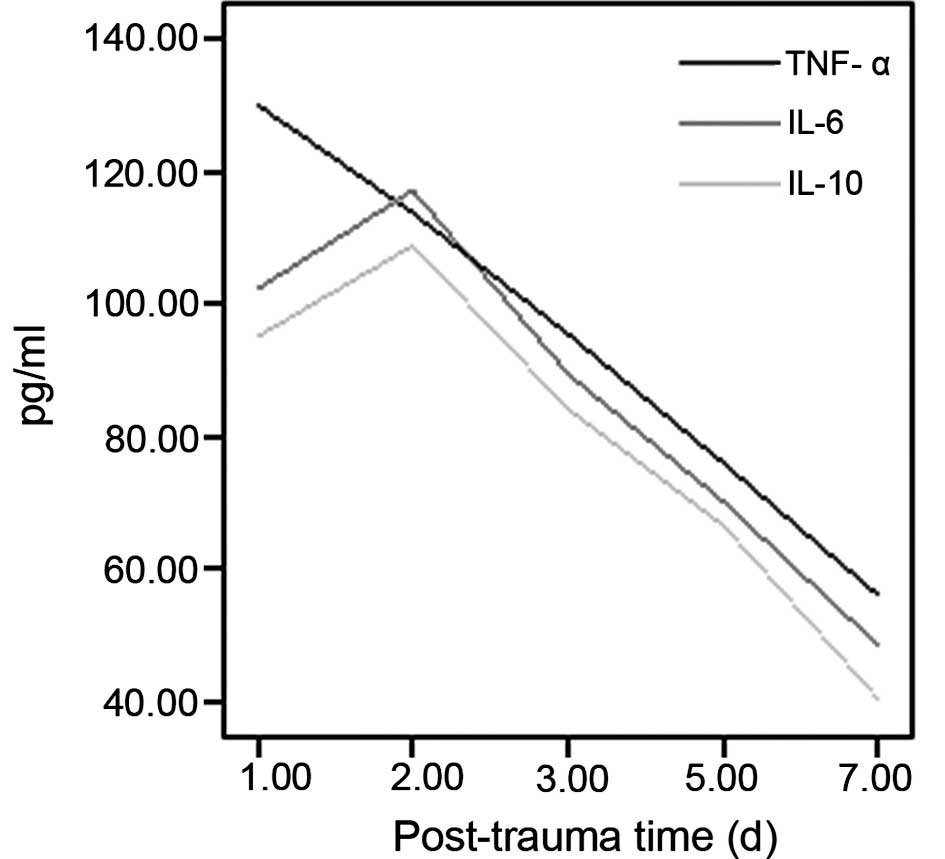
The serum TNF-α level significantly increased and
reached a peak in the patients with traumas complicated by
pulmonary contusion within 1 day after trauma, and these levels
exhibited a progressively decreasing trend throughout days 2, 3, 5
and 7 (Fig. 1). The serum levels
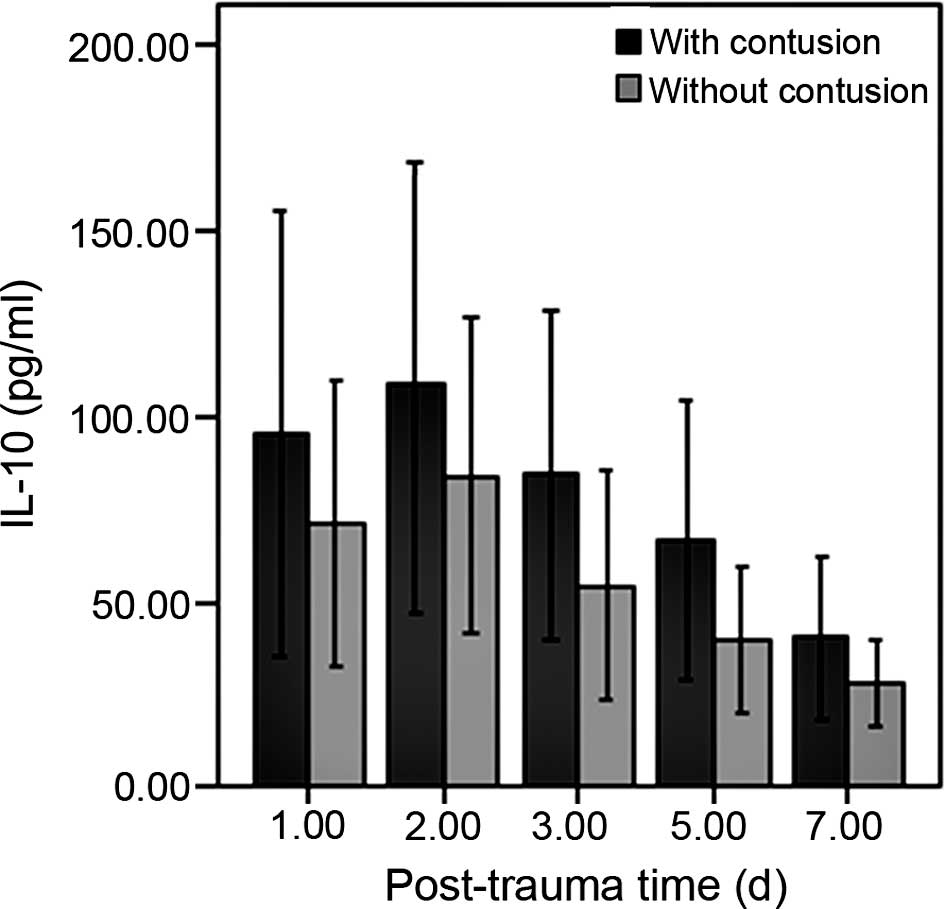
of IL-6 and IL-10 were significantly increased within 1 day after
trauma, both of which generally reached peaks on day 2, whereas
both markers decreased daily throughout days 3, 5 and 7 after
trauma (Figs. 2 and 3). On day 7 after trauma, the levels of
the three cytokines were still higher than the normal limits
(Fig. 4).
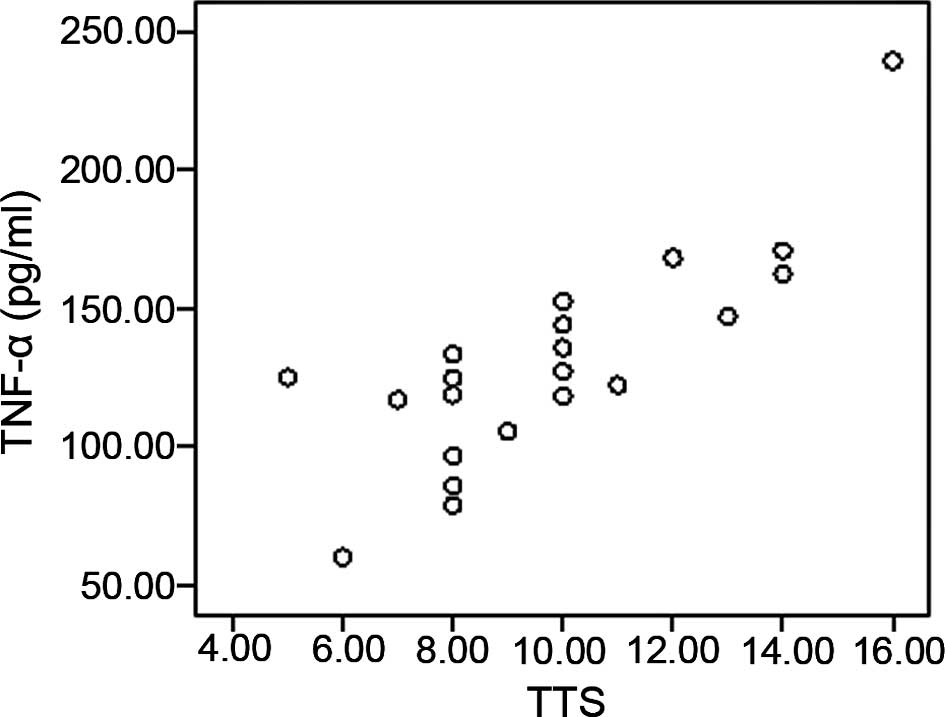
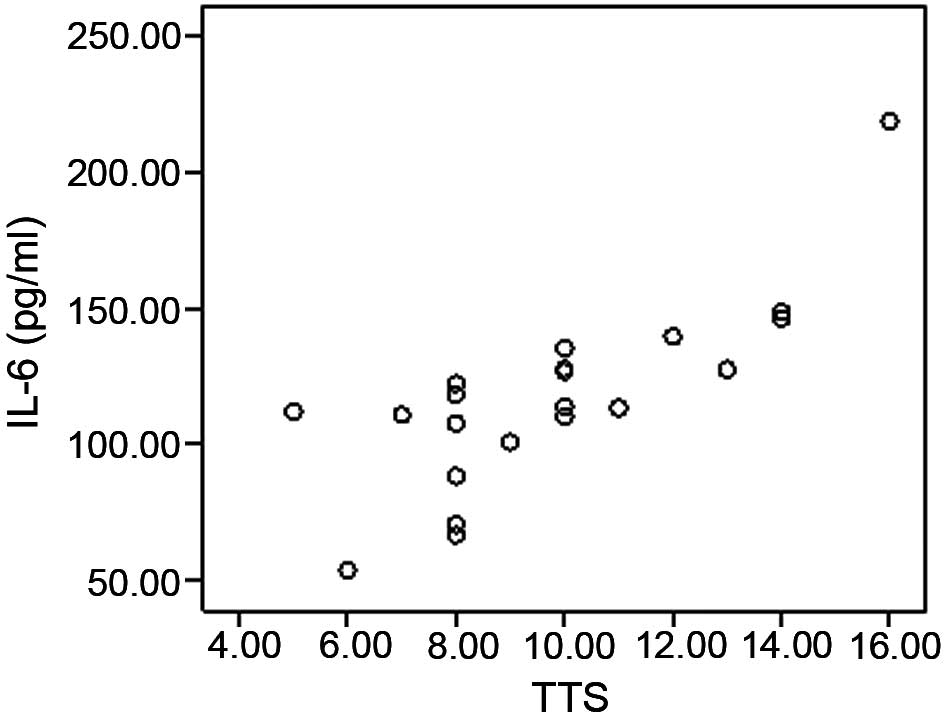
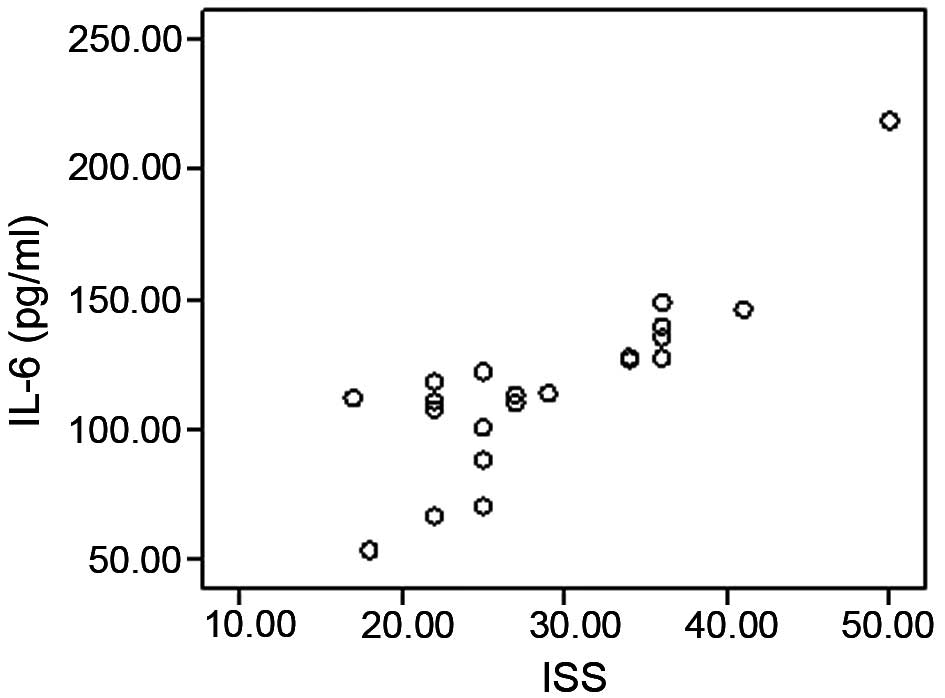
The correlation analysis showed that in patients
with traumas complicated by pulmonary contusion, the serum levels
of TNF-α (Figs. 5 and 6), IL-6 (Figs. 7 and 8) and IL-10 (Figs. 9 and 10) were positively correlated with TTS
and ISS in a statistically significant manner.
Discussion
Patients presenting with closed chest injuries are
usually in a serious condition when their injury is complicated by
pulmonary contusion and consequently are associated with a high
incidence of mortality. A potent inflammatory response occurs in
contused lung tissues, where inflammatory cytokines aggravate
pre-existing injuries through a cascade of reactions. Cytokines are
known to interact with each other, forming a complex cytokine
network, which plays an important role in the response to
post-traumatic inflammatory and immune imbalance (1).
TNF-α is a crucial inflammatory cytokine involved in
the response to severe trauma and demonstrates extensive biological
activity. TNF-α induces the release of other cytokines, such as
IL-6, which mediates the post-traumatic inflammatory response and
exacerbates the injuries to tissues and organs. IL-6 is synthesized
in response to the stimulation of TNF-α, and has no harmful effect
on cells itself, yet promotes the activation and aggregation of
neutrophils, reflecting the severity of tissue injury. IL-10 is a
superpotent, immunocompromising and anti-inflammatory cytokine
which plays an important role in the regulation of the cytokine
network. IL-10 inhibits the release of TNF-α, IL-1, IL-6 and INF-γ
from monocytes, which are stimulated to produce an IL-1 receptor
inhibitor in an anti-inflammatory manner. The expression of IL-10
demonstrates a linear correlation with the expression levels of
TNF-α, IL-6 and IL-8. The progression of injury and inflammation
increases the responsiveness of TNF-α, IL-6 and IL-8, whereas
anti-inflammatory cytokines, IL-1ra, IL-4 and IL-10, increase
simultaneously to antagonize the high levels of pro-inflammatory
factors. The rise in serum IL-10 in post-traumatic patients may
compromise immunity and impair resistance to infection (2). The present study demonstrated that
serum IL-10 reached a peak within 2 days after trauma, suggesting
the onset of an immune imbalance.
In the present study, TNF-α was found to be released
immediately following trauma. The level of TNF-α peaked on day 1
after trauma and initiated an inflammatory response. IL-6 and IL-10
were released at a later time point and their levels peaked on day
2, but decreased progressively afterwards. Levels of the above
three cytokines remained significantly higher 1 week after trauma
(P<0.01). Perl et al (3)
examined the levels of IL-6, IL-8, IL-10 and IL-12 in lungs,
skeleton, skin, subcutaneous fat and muscle in patients suffering
from a single trauma and found the highest level in lung tissues.
Our study also detected a significant difference in serum TNF-α,
IL-6 and IL-10 levels among trauma patients with pulmonary
contusion, trauma patients without contusion and healthy volunteers
(P<0.01). However, those with and without contusion did not
differ significantly in regards to ISS, suggesting that under
comparable systematic stress, patients with injuries complicated by
pulmonary contusion had a more serious inflammatory response and
higher inflammatory cytokine levels.
ISS is the most commonly used hospital evaluation
tool of trauma, and a higher score indicates a more severe injury
and a higher risk of mortality. It is common clinical practice to
regard ISS ≥16 as severe injury. All of the studied multiple trauma
patients had an ISS ≥16. Due to its limitations, the ISS does not
reflect pathological changes in patients and the effects of health
and age on injury, nor does it discriminate the severity of injury
in patients with comparable ISS or the difference between a single
injury and multiple injuries in a specific site. Inclusion of the
three most seriously injured areas separately is likely to
underestimate the severity of multiple injuries in a specific site.
In the present study, 5 patients suffered from bilateral pulmonary
contusions, whereas ISS only considered the unilateral condition,
failing to accurately reflect the injury. In patients concomitantly
complicated by multiple traumas and pulmonary contusion, ISS cannot
accurately assess the actual severity of injury. A specific scoring
system targeting chest injury is thus required. Pape et al
(4) established an early scoring
system for chest injury, namely TTS, through the analysis of 1,495
multiple trauma patients, which was rarely reported in patients
with injuries complicated with pulmonary contusion. The major
measures of TTS include the severity of chest and thoracic injury,
oxygenation index, patient age and bilateral injury. Such a scoring
system indicates that pulmonary contusion has a more significant
effect on prognosis than rib fracture. However, in patients over 70
years of age, rib fracture is a worse prognostic factor than
pulmonary contusion, and those with bilateral injuries have an even
higher risk of mortality. The severity of pulmonary contusion is
closely associated with prognosis; thus, development of an
objective evaluation tool is necessary. The severity of pulmonary
contusion should be evaluated within 24 h, based on imaging data
and oxygenation index.
Tyburski et al (5) established a pulmonary contusion
scoring system based on chest radiographs, where one third of the
unilateral pulmonary field was appraised as 3 points and entire
involvement of the unilateral field as 9 points. In this system, a
score of less than 3 points was evaluated as mild chest injury, 3–9
points as moderate and 10–18 points as severe chest injury. Chest
CT scan has a higher sensitivity and specificity than chest
radiography, and is a better estimate of the percent volume of
contused lung tissue in relation to the entire lung. It is also
more effective for identifying fractures of the sternum, thoracic
vertebrae and scapulae which are easily missed on radiographs
(6). Offner and Moore (7) characterized the severity of pulmonary
contusion according to grade 0–3 based on the ratio of
PaO2/FiO2, where grade 0 referred to a ratio
>250, grade 1, 175–250, grade 2, 100–174 and grade 3, <100.
Further clinical analysis confirmed that such a ratio was an
important measure for predicting mortality secondary to pulmonary
contusion.
In a simple pulmonary contusion animal model, the
most massive pathological response was found to occur within 8 min
to 24 h following trauma, when arterial oxygenation decreased
aggressively and the IL-6 level in bronchial alveolar lavage fluid
increased rapidly to a peak level (8). Kang et al (9) reported that in traumatized rodents,
middle-aged animals exhibited higher TNF-α, IL-6 and IL-10 levels
than young animals, suggesting the association of cytokine
secretion with age. Wichmann et al (10) reported that patients with
hemorrhagic bone fractures and cartilage injuries secreted more
inflammatory cytokines than those complicated without hemorrhage,
showing an immunocompromised immunity, suggesting the effect of
hemorrhage on the secretion of inflammatory cytokines. TSS involves
measures of the traumatized anatomical site in addition to patient
age, post-trauma physiological index and signs in a comprehensive
and objective manner.
In patients dying from serious injury, serum
pro-inflammatory cytokines, such as IL-6 and IL-8, remained at a
higher level than those in surviving patients in a relationship
proportional to the severity of the injury (11). Taniguchi et al (12) reported that the ratio of IL-6/IL-10
was positively correlated with ISS in patients suffering from
thoracic and abdominal injuries. This ratio was found to be a
prognostic factor; a higher ratio was associated with poor
prognosis and a lower ratio with a more favorable prognosis. The
present study demonstrated that pro-inflammatory cytokines, such as
TNF-α and IL-6, and anti-inflammatory cytokines, such as IL-10,
were positively correlated with both ISS and TTS. Similar to ISS,
TTS better reflected the severity of injury in a comprehensive and
objective manner, specifically evaluating the severity of chest
injury, independent of the conditions of other sites.
In the present study, serum inflammatory cytokines
increased significantly in patients concomitantly suffering from
closed chest injury and pulmonary contusion, showing a stronger
inflammatory response. TSS may be used as an evaluation tool to
accurately assess the severity of chest injury. For patients with
multiple trauma dominantly involving chest injury, the evaluation
of injury severity should incorporate ISS and TTS, which can
characterize the systemic injury and local condition. The dynamic
monitoring of plasma TNF-α, IL-6 and IL-10 has a significant role
in the prediction of the clinical outcome of patients with closed
chest injuries with pulmonary contusions.
References
|
1.
|
Dinarello CA: Proinflammatory and
anti-inflammatory cytokines as mediators in the pathogenesis of
septic shock. Chest. 112:S321–S329. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Lyons A, Goebel A, Mannick JA and Lederer
JA: Protective effects of early interleukin 10 antagonism on
injury-induced immune dysfunction. Arch Surg. 134:1317–1324. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Perl M, Gebhard F, Knoferl MW, Bachem M,
Gross HJ, Kinzl L and Strecker W: The pattern of preformed
cytokines in tissues frequently affected by blunt trauma. Shock.
19:299–304. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Pape HC, Remmers D, Rice J, Ebisch M,
Krettek C and Tscherne H: Appraisal of early evaluation of blunt
chest trauma: development of a standardized scoring system for
initial clinical decision making. J Trauma. 49:496–504. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Tyburski JG, Collinge JD, Wilson RF and
Eachempati SR: Pulmonary contusions: quantifying the lesions on
chest X-ray films and the factors affecting prognosis. J Trauma.
46:833–838. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Traub M, Stevenson M, McEvoy S, Briggs G,
Lo SK, Leibman S and Joseph T: The use of chest computed tomography
versus chest X-ray in patients with major blunt trauma. Injury.
38:43–47. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Offner PJ and Moore EE: Lung injury
severity scoring in the era of lung protective mechanical
ventilation: the PaO2/FIO2 ratio. J Trauma.
55:285–289. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Raghavendran K, Davidson BA, Woytash JA,
et al: The evolution of isolated bilateral lung contusion from
blunt chest trauma in rats: cellular and cytokine responses. Shock.
24:132–138. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Kang SC, Matsutani T, Choudhry MA,
Schwacha MG, Rue LW, Bland KI and Chaudry IH: Are the immune
responses different in middle-aged and young mice following bone
fracture, tissue trauma and hemorrhage? Cytokine. 26:223–230. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Wichmann MW, Ayala A and Chaudry IH:
Severe depression of host immune functions following closed-bone
fracture, soft-tissue trauma, and hemorrhagic shock. Crit Care Med.
26:1372–1378. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Mimasaka S, Ohtsu Y, Tsunenari S and
Funayama M: Postmortem cytokine levels and severity of traumatic
injuries. Int J Legal Med. 120:265–270. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Taniguchi T, Koido Y, Aiboshi J, Yamashita
T, Suzaki S and Kurokawa A: The ratio of interleukin-6 to
interleukin-10 correlates with severity in patients with chest and
abdominal trauma. Am J Emerg Med. 17:548–551. 1999. View Article : Google Scholar : PubMed/NCBI
|