Introduction
Hepatitis C virus (HCV) infection has become a
worldwide health problem (1). More
than 170 million persons are infected with HCV. After HCV
infection, more than 80% of infected patients progress to chronic
hepatitis and other hepatic diseases (2). Pegylated-interferon (Peg-IFN) and
ribavirin (RBV) combination therapy, which is the most effective
initial therapy for viral clearance, has been recognized as a
standard treatment for HCV infection. Unfortunately, this standard
therapy produces sustained virological response (SVR) in only 50%
of patients.
Many host and viral factors (3–5),
particularly associated with racial descent, the genotype of HCV
and variation in certain genes, influence the treatment response to
Peg-IFN and RBV combination therapy. Recent genome-wide association
studies (11–14) have shown that genetic variation
(rs8099917 and rs12979860) in the IL28B gene is strongly associated
with spontaneous clearance of HCV and treatment response to
standard therapy in HCV-infected patients. In addition, previous
studies (4,6,7)
suggest that African-American ancestry is a powerful negative
predictive factor for SVR. Moreover, patients with HCV1 infection
were found to have a lower SVR rate than those with HCV2/3
infection (8–10). However, the association between
IL28B polymorphisms and SVR to standard treatment in different
racial populations or in patients infected with different genotypes
of HCV has not yet been elucidated.
Ge et al (12) found that Asian patients have the
highest C allele frequency at rs12979860, followed by European
patients and African patients. The SVR rates across different
population groups displayed a striking concordance with C allele
frequency at rs12979860. This finding partly elucidates the
differential treatment response in patients of different racial
descent. However, is the common allele frequency the only reason
for the different SVR rates across different population groups? It
is still not clear whether racial descent itself contributes to the
different SVR rates across different population groups. Moreover,
previous studies (8–10) suggest that treatment with Peg-IFN
and RBV results in a lower SVR rate in patients with HCV genotype 1
(HCV1) than in patients with HCV genotypes 2 and/or 3 (HCV2/3).
However, the inner factors, which contribute to this difference,
are yet unclear. Therefore, an investigation of the polymorphisms
of the IL28B gene may partly elucidate this difference.
The present meta-analysis was conducted to provide
an accurate estimation of the association between the two
polymorphisms and SVR to standard treatment in patients of
different racial descent infected with different genotypes of HCV,
and also to investigate the possible factors associated with the
interleukin 28B (IL28B) gene that may contribute to the different
SVR rates of patients with different subtypes of HCV infection
across different populations. Notably, we found that both the
common allele frequency and racial descent itself contributed to
the difference in SVR rates across different population groups, and
the common allele frequency may partly explain the difference in
SVR rates in patients with different genotypes of HCV.
Materials and methods
Literature search strategy
This meta-analysis was performed as described
previously (15,16). The electronic PubMed database was
searched (updated on March 30, 2011) using the following terms:
IL28B and interferon λ3 (IFN λ3), combined with hepatitis C and
HCV. Two reviewers (Wu and Wang) evaluated the titles and abstracts
of the identified studies and references in the articles, and
previous reviews for possible inclusion, respectively. Only studies
published in English with full text articles were included in our
study. The eligibility criteria included i) studies with available
data to evaluate treatment success; ii) studies that examined the
association between IL28B polymorphisms and treatment response of
hepatitis C; iii) studies involving patients treated with standard
therapy for HCV; iv) studies demonstrating treatment success based
on an SVR, which was defined as undetectable HCV-RNA levels at 24
weeks post-treatment; v) studies with data that could be divided
into an SVR group and non-SVR group; and vi) studies with
sufficient and accurate data that could be extracted and calculated
for estimating an odds ratio (OR) with 95% confidence interval
(CI). For overlapping studies, only the study with the largest
sample size was selected.
Data extraction
The following information was carefully extracted
from the eligible studies independently by two reviewers (Wu and
Wang): first author’s name, year of publication, racial descent of
the study population (categorized as Asian, European and African
populations), number of different genotypes in the SVR group and
non-SVR group, Hardy-Weinberg equilibrium (HWE) and genotype of
HCV. Consensus was reached concerning all data by discussion.
Statistical analysis
Crude ORs with 95% CI were used to assess the
association between IL28B polymorphisms and treatment response of
hepatitis C. For meta-analysis of the association (case-control)
studies, patients with SVR were considered as case patients, and
patients without SVR were considered as control patients (17). Q statistics (18) was used to test the between-study
heterogeneity. Between-study heterogeneity was considered to be
significant at a P-value <0.10. When between-study heterogeneity
existed, a random-effects model (the DerSimonian and Laird method)
(19) was selected. Otherwise, the
fixed-effects model (the Mantel-Haenszel method) (20) was used. Publication bias was tested
by Funnel plots and Egger’s linear regression (P<0.05 considered
statistical significance). Fisher’s exact test was used to compare
the frequency of the genotypes at rs8099917 and rs12979860 in
different patients. All analyses were performed using the software
Stata version 11.0 (Stata Corporation, College Station, TX,
USA).
Results
Eligible studies
Twenty-six studies (4,10,13,17,21–42)
were included in this meta-analysis (Fig. 1). As shown in Table I, 16 studies (10,13,21–34)
were eligible for examining the association between the IL28B
polymorphism rs8099917 and treatment response of hepatitis C,
including 3,540 cases with SVR and 2,208 cases with non-SVR. As
shown in Table II, 17 studies
(4,10,17,21,27–29,33–42)
were eligible for examining the association between the IL28B
polymorphism rs12979860 and treatment response of hepatitis C,
including 2,951 cases with SVR and 2,506 cases with non-SVR.
 | Table I.Characteristics of the studies
included for the association between IL28B polymorphism rs8099917
and treatment response of hepatitis C. |
Table I.
Characteristics of the studies
included for the association between IL28B polymorphism rs8099917
and treatment response of hepatitis C.
| Authors (Ref.) | Racial descent | Year | SVR
| Non-SVR
| P-value of HWE | HCV genotype |
|---|
| TT | Non-TT (TG/GG) | TT | Non-TT (TG/GG) |
|---|
| Suppiah et
al (13) | European | 2009 | 247 | 145 (130/15) | 195 | 261 (227/34) | NA | 1 |
| Hayes et al
(21) | Asian | 2011 | 311 | 54 (51/3) | 277 | 170 (148/22) | NA | 1 |
| Rauch et al
(22) | European | 2010 | 201 | 96 (86/10) | 71 | 97 (85/12) | NA | 1–4 |
| Aparicio et
al (23) | European | 2010 | 56 | 11 | 48 | 45 | >0.05 | 1,3,4; HIV |
| Grebely et
al (24) | Europeanb | 2010 | 18 | 16 (13/3) | 11 | 9 (9/0) | >0.05 | 1–4a |
| Yu et al
(25) | Asian | 2011 | 386 | 43 | 46 | 7 | >0.05 | 2 |
| Hsu et al
(26) | Asian | 2011 | 67 | 7 (7/0) | 10 | 7 (7/0) | NA | 1,2 |
| Moghaddam et
al (27) | European | 2011 | 161 | 65 (59/6) | 40 | 15 (14/1) | >0.01 | 3 |
| Chen et al
(28) | Asian | 2011 | 517 | 42 (42/0) | 135 | 34 (33/1) | <0.05 | Multiple |
| Scherzer et
al (29) | European | 2011 | 29 | 24 (24/0) | 10 | 6 (5/1) | NA | 3 |
| Sakamoto et
al (30) | Asian | 2011 | 81 | 17 | 19 | 12 | NA | 2 |
| Lagging et
al (10) | European | 2011 | 54 | 34 | 43 | 37 | <0.05 | 1 |
| Kurosaki et
al (31) | Asian | 2011 | 173 | 20 (20/0) | 172 | 131 (126/5) | NA | 1 |
| Kawaoka et
al (32) | Asian | 2011 | 372 | 70 | 180 | 66 | NA | 2 |
| Bochud et al
(33) | European | 2011 | 47 | 16 (15/1) | 6 | 3 (3/0) | >0.05 | 2,3 |
| Sarrazin et
al (34) | European | 2011 | 99 | 61 (54/7) | 24 | 21 (20/1) | >0.05 | 2,3 |
 | Table II.Characteristics of the studies
included for the association between IL28B polymorphism rs12979860
and treatment response of hepatitis C. |
Table II.
Characteristics of the studies
included for the association between IL28B polymorphism rs12979860
and treatment response of hepatitis C.
| Authors (Ref.) | Racial descent | Year | SVR
| Non-SVR
| P-value of HWE | HCV genotype |
|---|
| CC | Non-CC (CT/TT) | CC | Non-CC (CT/TT) |
|---|
| Mangia et al
(35) | European | 2010 | 82 | 119 (96/23) | 18 | 49 (32/17) | >0.05 | 2,3 |
| Hayes et al
(21) | Asian | 2011 | 311 | 55 (51/4) | 271 | 175 (152/23) | NA | 1 |
| McCarthy et
al (36) | European,
African | 2010 | 43 | 29 (22/7) | 33 | 126 (99/27) | <0.05 | 1,2,3 |
| Pineda et al
(37) | European | 2010 | 48 | 29 (19/10) | 20 | 57 (47/10) | >0.05 | 1–4; HIV |
| Thompson et
al (4) | European,
African | 2010 | 340 | 299 (239/60) | 172 | 776 (559/217) | NA | 1 |
| Montes-Cano et
al (38) | European | 2010 | 68 | 45 | 34 | 72 | >0.05 | 1–4 |
| Honda et al
(39) | Asian | 2010 | 12 | 3 (3/0) | 6 | 11 (10/1) | NA | 1 |
| de Araújo et
al (40) | NA | 2010 | 4 | 3 | 3 | 11 | NA | 1,3; HIV |
| Nattermann et
al (17) | European | 2011 | 83 | 89 (79/10) | 54 | 122 (96/26) | >0.05 | Multiplea |
| Darling et
al (41) | European,
African | 2011 | 55 | 68 (51/17) | 8 | 79 (52/27) | NA | 1 |
| Moghaddam et
al (27) | European | 2011 | 99 | 127 (105/22) | 30 | 25 (24/1) | >0.01 | 3 |
| Chen et al
(28) | Asian | 2011 | 521 | 38 (38/0) | 133 | 36 (35/1) | >0.05 | Multiple |
| Scherzer et
al (29) | European | 2011 | 19 | 34 (31/3) | 6 | 10 (8/2) | NA | 3 |
| Reiberger et
al (42) | European | 2011 | 7 | 10 | 9 | 26 | NA | 1–4 |
| Lagging et
al (10) | European | 2011 | 29 | 59 | 15 | 65 | <0.05 | 1 |
| Bochud et al
(33) | European | 2011 | 41 | 22 (18/4) | 5 | 4 (4/0) | >0.05 | 2,3 |
| Sarrazin et
al (34) | European | 2011 | 76 | 84 (51/33) | 11 | 34 (15/19) | >0.05 | 2,3 |
Meta-analysis
Results of the association between
IL28B polymorphism rs8099917 and treatment response of HCV
For rs8099917, patients with the TT genotype
(2,819/4,106) had a higher rate of SVR than G allele carriers
(721/1,642) from 16 studies (TT vs. TG/GG, OR=2.29, 95% CI
1.74–3.01, P<0.001 for heterogeneity). Of these 16 studies,
seven (21,25,26,28,30–32)
examined the association between IL28B polymorphism rs8099917 and
the SVR rate in an Asian population, and the other nine in a
European population. The SVR rate in Asian patients (2,160/3,426)
was higher than that in European patients (1,380/2,322) (P=0.006).
Compared to the non-TT genotype, Asian (TT vs. TG/GG, OR=3.17, 95%
CI 2.15–4.68, P=0.003 for heterogeneity; Fig. 2) and European (TT vs. TG/ GG,
OR=1.74, 95% CI 1.22–2.48, P=0.005 for heterogeneity; Fig. 2) patients with the TT genotype both
had a significantly higher SVR rate. Furthermore, the frequency of
the TT genotype in Asian patients (2,746/3,426) was higher than
that in the European patients (1,360/2,322) (P<0.001).
Of these 16 studies, four (10,13,21,31)
were conducted to investigate the predictive value of IL28B
polymorphism rs8099917 on the effect of standard therapy in
patients with HCV1, and seven (25,27,29,30,32–34)
in patients with HCV2/3. The rate of SVR to treatment in patients
with HCV1 (1,038/2,324) was lower than in those with HCV2/3
(1,471/1,926) (P<0.001). Compared to the non-TT genotype,
HCV1-infected patients with the TT genotype showed a significantly
higher SVR rate (TT vs. TG/GG, OR=2.95, 95% CI 1.74–4.99,
P<0.001 for heterogeneity; Fig.
2). Similar results were observed in the HCV2/3-infected
patients (TT vs. TG/GG, OR=1.56, 95% CI 1.21–2.01, P=0.264 for
heterogeneity; Fig. 2).
Furthermore, the frequency of the TT genotype in patients with HCV1
(1,472/2,324) was less than than in patients with HCV2/3
(1,500/1,926) (P<0.001).
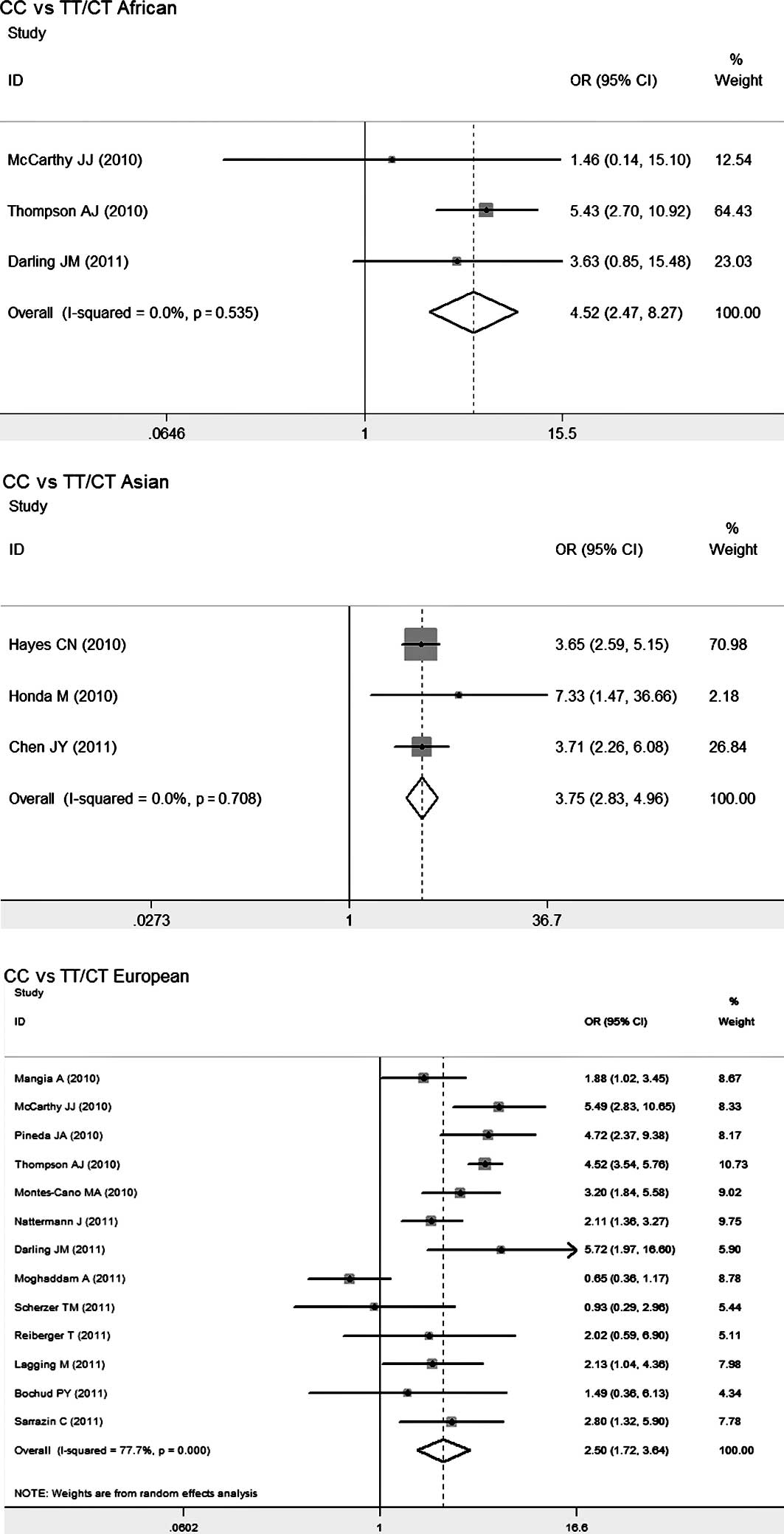
Results of the association between
IL28B polymorphism rs12979860 and treatment response for HCV
This meta-analysis showed that patients with the
homozygous CC genotype (1,838/2,666) had a significantly higher SVR
rate for HCV than T allele carriers (1,113/2,791) (CC vs. CT/TT,
OR=2.91, 95% CI 2.13–3.98, P<0.001 for heterogeneity). Of these
17 studies, three (4,36,41)
examined the association between IL28B polymorphism rs12979860 and
the SVR rate in an African population, three (21,28,39)
in an Asian population and 13 (4,10,17,27,29,33–38,41,42)
in a European population. The SVR rate was highest in the Asian
population (940/1,572), followed by the European population
(1,904/3,412) and African population (100/452) (P<0.001).
Relative to T allele carriers, African patients with the CC
genotype had the highest SVR rate (CC vs. CT/TT, OR=4.52, 95% CI
2.47–8.27, P=0.535 for heterogeneity; Fig. 3), followed by Asian patients (CC
vs. CT/TT, OR=3.75, 95% CI 2.83–4.96, P=0.708 for heterogeneity;
Fig. 3) and European patients (CC
vs. CT/ TT, OR=2.50, 95% CI 1.72–3.64, P<0.001 for
heterogeneity; Fig. 3). Moreover,
the CC genotype (59/452) at rs12979860 was less frequent in the
African patients than that in the European (1,346/3,412) and Asian
patients (1,254/1,572) (P<0.001).
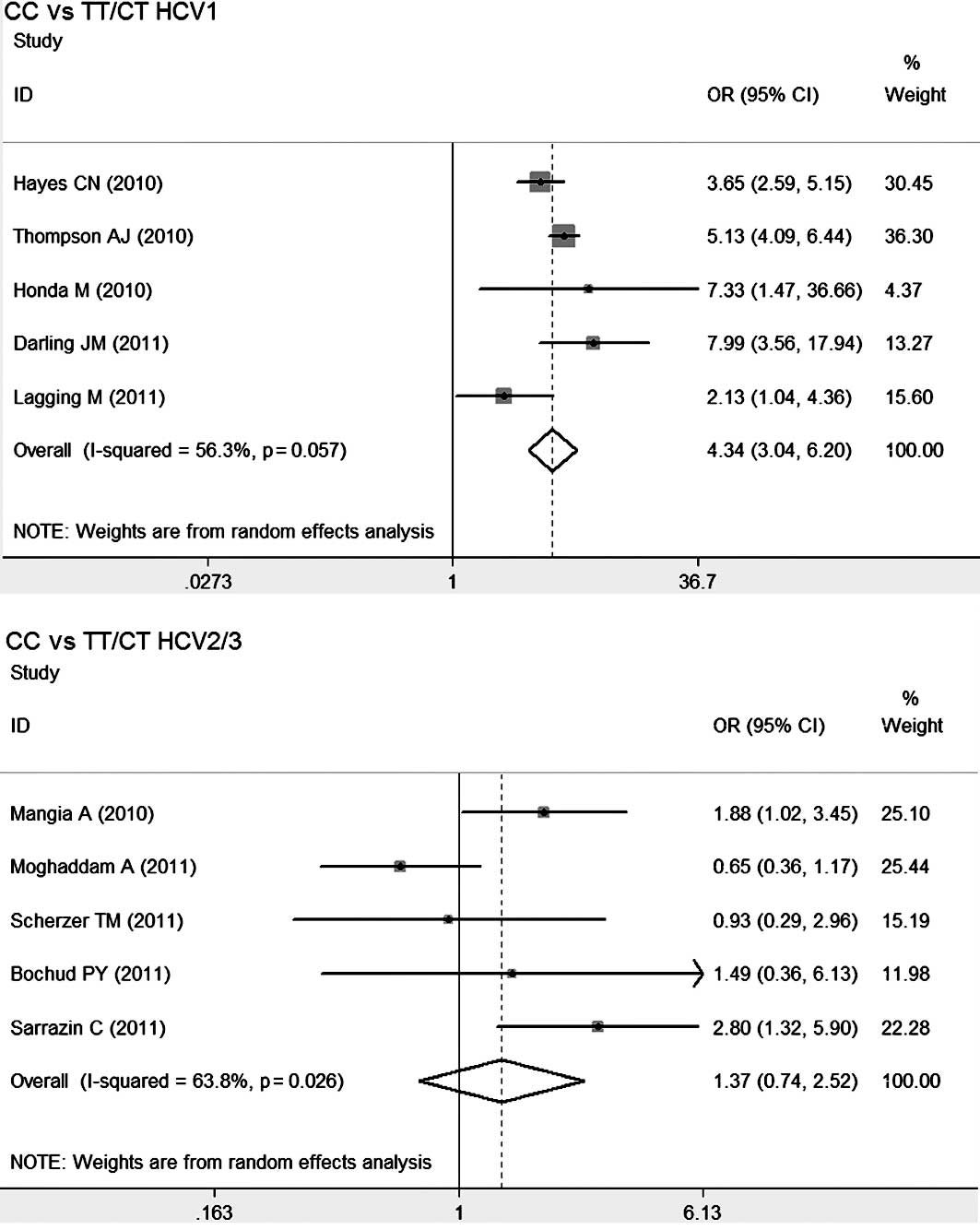
Five studies (4,10,21,39,41)
were conducted to investigate the predictive value of IL28B
polymorphism rs12979860 on the effect of standard therapy in
patients with HCV1, and five (27,29,33–35)
in patients with HCV2/3. The rate of SVR to treatment in patients
with HCV1 (1,231/2,809) was lower than that in patients with HCV2/3
(703/895) (P<0.001). Compared to T allele carriers, the
HCV1-infected patients with the CC genotype (CC vs. CT/TT, OR=4.34,
95% CI 3.04–6.20, P=0.057 for heterogeneity; Fig. 4) appeared to have a higher rate of
SVR compared to that of the HCV2/3-infected patients with the CC
genotype (CC vs. CT/TT, OR=1.37, 95% CI 0.74–2.52, P=0.026 for
heterogeneity; Fig. 4).
Furthermore, the CC genotype in the HCV1-infected patients
(1,219/2,809) was almost the same as that in the HCV2/3-infected
patients (387/895) (P>0.05).
Co-expression of the TT
genotype at rs8099917 and CC genotype at rs12979860
Patients with co-expression of the common homozygote
TT genotype at rs8099917 and CC genotype at rs12979860 appeared to
have a higher SVR rate than the rate in patients with the other
genotypes. Data were obtained from only two studies (29,39).
Patients with the common homozygote CC genotype at rs12979860 and
the TT genotype at rs8099917 had a higher rate of SVR (30/42) than
patients with co-expression of the rare homozygote TT genotype at
rs12979860 and GG genotype at rs8099917 (0/2) and all other
genotypes (38/57), but no significant difference was observed
(P>0.05). More data are required to examine the association
between co-expression of the TT genotype at rs8099917 and CC
genotype at rs12979860 and treatment response to anti-HCV
therapy.
Publication bias
Funnel plot and Egger’s test were performed to
assess the publication bias of studies which examined the
association between IL28B polymorphisms (rs8099917 and rs12979860)
and treatment response of hepatitis C. In the overall studies, no
significant publication bias (P>0.05) was detected (data not
shown).
Discussion
The present meta-analysis provides an accurate
estimation of the association between the two polymorphisms and SVR
to standard treatment in patients of different racial descent
infected with different genotypes of HCV. The frequency of the
common homozygote (TT genotype at rs8099917 and CC genotype at
rs12979860) in Asian patients was higher than that in the European
population. Furthermore, relative to the non-common homozygote
genotype, Asian patients with the common homozygote appeared to
have a higher SVR rate. Not only the frequency of the C allele at
rs12979860 and T allele at rs8099917, but also the racial descent
itself contributed to the high SVR rate in Asian patients. The SVR
rate in patients with HCV1 was lower than that in those with
HCV2/3. A low frequency of the common homozygote appeared to
contribute to the low SVR rate in HCV1-infected patients. Further
clinical trials should be carried out to confirm these significant
findings.
The IL28B gene encodes IFN λ3 (43,44),
whose polymorphisms are strongly associated with treatment
response. Our study confirmed that the common homozygote of the two
polymorphisms had a strong impact on SVR of HCV. IL28B
polymorphisms provide useful pre-treatment stratification of
patients for HCV treatment (12).
We found that Asian patients with the common homozygote (TT
genotype at rs8099917 and CC genotype at rs12979860) attained a
higher rate of SVR when compared with European patients. Moreover,
Asian HCV patients had a higher frequency of the common homozygote.
Therefore, as demonstrated in previous studies (45,46),
Asian HCV patients had a better response to treatment than European
patients in this study. Ge et al (12) found that the SVR rates across
different population groups displayed a striking concordance with C
allele frequency. Our results suggest that not only the frequency
of the C allele at rs12979860 and T allele at rs8099917, but also
racial descent contributed to the different SVR rates across the
different population groups. We found that African patients with
the CC genotype had a higher SVR rate than T allele carriers.
However, the the CC genotype at rs12979860 was far less frequent in
African patients than in European and Asian patients in this
meta-analysis. Thus, African patients still had the poorest
response to treatment in accordance with previous studies (4,6,7).
Previous studies (8–10)
suggest that treatment with Peg-IFN and RBV results in a lower SVR
rate in patients with HCV1 than in patients with HCV2/3. The same
result was observed in this meta-analysis. We found that
HCV1-infected patients with the TT genotype had a higher rate of
SVR compared to patients with HCV2/3. However, the frequency of the
TT genotype at rs8099917 in HCV1 was lower than that in patients
with HCV2/3 (P<0.001). Thus, the patients with HCV2/3 had a
better outcome in our study.
Limitations did exist in the present meta-analysis.
First, unadjusted ORs were obtained, and a more precise estimation
may have be obtained adjusting according to age, gender, racial
descent, genotype of HCV and variation in genes. Second, a
deviation in HWE existed in several studies. However, the
deviation, which may reflect a potential association between
genotype and HCV infection, cannot be attributed to genotyping
error (36). Third, several
patients with HCV infection included in this meta-analysis were
co-infected with HIV and/ or HBV.
In conclusion, this meta-analysis found that
patients with the common homozygote attained a higher rate of SVR
to Peg-IFN and RBV combination therapy. Notably, we found that not
only the frequency of the C allele at rs12979860 and T allele at
rs8099917, but also racial descent contributed to the different SVR
rates across the different population groups. Moreover, a low
frequency of the common homozygote may contribute to a low SVR rate
in HCV1-infected patients.
References
|
1.
|
GM LauerBD WalkerHepatitis C virus
infectionN Engl J
Med3454152200110.1056/NEJM20010705345010711439948
|
|
2.
|
DL ThomasLB SeeffNatural history of
hepatitis CClin Liver
Dis9383398200510.1016/j.cld.2005.05.00316023972
|
|
3.
|
JG McHutchisonEJ LawitzML
ShiffmanPeginterferon alfa-2b or alfa-2a with ribavirin for
treatment of hepatitis C infectionN Engl J
Med361580593200910.1056/NEJMoa080801019625712
|
|
4.
|
AJ ThompsonAJ MuirMS
SulkowskiInterleukin-28B polymorphism improves viral kinetics and
is the strongest pretreatment predictor of sustained virologic
response in genotype 1 hepatitis C
virusGastroenterology139120129.e18201010.1053/j.gastro.2010.04.013
|
|
5.
|
CL ThioDL ThomasM CarringtonChronic viral
hepatitis and the human
genomeHepatology31819827200010.1053/he.2000.431610733534
|
|
6.
|
AJ MuirJD BornsteinPG
KillenbergPeginterferon alfa-2b and ribavirin for the treatment of
chronic hepatitis C in blacks and non-Hispanic whitesN Engl J
Med35022652271200410.1056/NEJMoa03250215163776
|
|
7.
|
HS ConjeevaramMW FriedLJ
JeffersPeginterferon and ribavirin treatment in African American
and Caucasian American patients with hepatitis C genotype
1Gastroenterology131470477200610.1053/j.gastro.2006.06.00816890601
|
|
8.
|
MW FriedML ShiffmanKR ReddyPeginterferon
alfa-2a plus ribavirin for chronic hepatitis C virus infectionN
Engl J Med347975982200210.1056/NEJMoa02004712324553
|
|
9.
|
MP MannsJG McHutchisonSC
GordonPeginterferon alfa-2b plus ribavirin compared with interferon
alfa-2b plus ribavirin for initial treatment of chronic hepatitis
C: a randomised
trialLancet358958965200110.1016/S0140-6736(01)06102-511583749
|
|
10.
|
M LaggingG AskariehF NegroResponse
prediction in chronic hepatitis C by assessment of IP-10 and
IL28B-related single nucleotide polymorphismsPLoS
One6e17232201110.1371/journal.pone.001723221390311
|
|
11.
|
DL ThomasCL ThioMP MartinGenetic variation
in IL28B and spontaneous clearance of hepatitis C
virusNature461798801200910.1038/nature0846319759533
|
|
12.
|
D GeJ FellayAJ ThompsonGenetic variation
in IL28B predicts hepatitis C treatment-induced viral
clearanceNature461399401200910.1038/nature0830919684573
|
|
13.
|
V SuppiahM MoldovanG AhlenstielIL28B is
associated with response to chronic hepatitis C interferon-alpha
and ribavirin therapyNat
Genet4111001104200910.1038/ng.44719749758
|
|
14.
|
Y TanakaN NishidaM SugiyamaGenome-wide
association of IL28B with response to pegylated interferon-alpha
and ribavirin therapy for chronic hepatitis CNat
Genet4111051109200910.1038/ng.44919749757
|
|
15.
|
X LiuZ WangJ YuG LeiS WangThree
polymorphisms in interleukin-1beta gene and risk for breast cancer:
a meta-analysisBreast Cancer Res
Treat124821825201010.1007/s10549-010-0910-320437198
|
|
16.
|
WB ZhouDQ XueXA LiuQ DingS WangThe
influence of family history and histological stratification on
breast cancer risk in women with benign breast disease: a
meta-analysisJ Cancer Res Clin
Oncol13710531060201110.1007/s00432-011-0979-z21499874
|
|
17.
|
J NattermannM VogelHD NischalkeGenetic
variation in IL28B and treatment-induced clearance of hepatitis C
virus in HIV-positive patients with acute and chronic hepatitis CJ
Infect Dis203595601201110.1093/infdis/jiq09821257738
|
|
18.
|
J LauJP IoannidisCH SchmidQuantitative
synthesis in systematic reviewsAnn Intern
Med127820826199710.7326/0003-4819-127-9-199711010-000089382404
|
|
19.
|
R DerSimonianN LairdMeta-analysis in
clinical trialsControl Clin
Trials7177188198610.1016/0197-2456(86)90046-23802833
|
|
20.
|
N MantelW HaenszelStatistical aspects of
the analysis of data from retrospective studies of diseaseJ Natl
Cancer Inst22719748195913655060
|
|
21.
|
CN HayesM KobayashiN AkutaHCV
substitutions and IL28B polymorphisms on outcome of peg-interferon
plus ribavirin combination
therapyGut60261267201110.1136/gut.2010.22349521068134
|
|
22.
|
A RauchZ KutalikP DescombesGenetic
variation in IL28B is associated with chronic hepatitis C and
treatment failure: a genome-wide association
studyGastroenterology1381338134545
e17201010.1053/j.gastro.2009.12.05620060832
|
|
23.
|
E AparicioM PareraS FrancoN Perez-AlvarezC
TuralB ClotetMA MartinezIL28B SNP rs8099917 is strongly associated
with pegylated interferon-alpha and ribavirin therapy treatment
failure in HCV/HIV-1 coinfected patientsPLoS
One5e13771201010.1371/journal.pone.001377121048934
|
|
24.
|
J GrebelyK PetoumenosM HellardPotential
role for interleukin-28B genotype in treatment decision-making in
recent hepatitis C virus
infectionHepatology5212161224201010.1002/hep.2385020803561
|
|
25.
|
ML YuCF HuangJF HuangRole of
interleukin-28B polymorphisms in the treatment of hepatitis C virus
genotype 2 infection in Asian
patientsHepatology53713201110.1002/hep.2397621254157
|
|
26.
|
CS HsuSJ HsuHC ChenAssociation of IL28B
gene variations with mathematical modeling of viral kinetics in
chronic hepatitis C patients with IFN plus ribavirin therapyProc
Natl Acad Sci USA10837193724201110.1073/pnas.110034910821321200
|
|
27.
|
A MoghaddamE MelumN ReintonH Ring-LarsenH
VerbaanK BjøroO DalgardIL28B genetic variation and treatment
response in patients with hepatitis C virus genotype 3
infectionHepatology53746754201110.1002/hep.2415421374656
|
|
28.
|
JY ChenCY LinCM WangIL28B genetic
variations are associated with high sustained virological response
(SVR) of interferon-alpha plus ribavirin therapy in Taiwanese
chronic HCV infectionGenes
Immun12300309201110.1038/gene.2011.121346780
|
|
29.
|
TM ScherzerH HoferAF StaettermayerEarly
virologic response and IL28B polymorphisms in patients with chronic
hepatitis C genotype 3 treated with peginterferon alfa-2a and
ribavirinJ
Hepatol54866871201110.1016/j.jhep.2010.08.02421145807
|
|
30.
|
N SakamotoM NakagawaY TanakaAssociation of
IL28B variants with response to pegylated-interferon alpha plus
ribavirin combination therapy reveals intersubgenotypic differences
between genotypes 2a and 2bJ Med
Virol83871878201110.1002/jmv.22038
|
|
31.
|
M KurosakiY TanakaN NishidaPre-treatment
prediction of response to pegylated-interferon plus ribavirin for
chronic hepatitis C using genetic polymorphism in IL28B and viral
factorsJ Hepatol54439448201110.1016/j.jhep.2010.07.037
|
|
32.
|
T KawaokaCN HayesW OhishiPredictive value
of the IL28B polymorphism on the effect of interferon therapy in
chronic hepatitis C patients with genotypes 2a and 2bJ
Hepatol54408414201110.1016/j.jhep.2010.07.03221112660
|
|
33.
|
PY BochudS BibertF NegroIL28B
polymorphisms predict reduction of HCV RNA from the first day of
therapy in chronic hepatitis CJ HepatolFeb2011(E-pub ahead of
print).
|
|
34.
|
C SarrazinS SusserA DoehringImportance of
IL28B gene polymorphisms in hepatitis C virus genotype 2 and 3
infected patientsJ
Hepatol54415421201110.1016/j.jhep.2010.07.04121112657
|
|
35.
|
A MangiaAJ ThompsonR SantoroAn IL28B
polymorphism determines treatment response of hepatitis C virus
genotype 2 or 3 patients who do not achieve a rapid virologic
responseGastroenterology1398218277
e1201010.1053/j.gastro.2010.05.07920621700
|
|
36.
|
JJ McCarthyJH LiA ThompsonReplicated
association between an IL28B gene variant and a sustained response
to pegylated interferon and
ribavirinGastroenterology13823072314201010.1053/j.gastro.2010.02.00920176026
|
|
37.
|
JA PinedaA CaruzA RiveroPrediction of
response to pegylated interferon plus ribavirin by IL28B gene
variation in patients coinfected with HIV and hepatitis C virusClin
Infect Dis51788795201010.1086/65623520804372
|
|
38.
|
MA Montes-CanoJR Garcia-LozanoC
Abad-MolinaInterleukin-28B genetic variants and hepatitis virus
infection by different viral
genotypesHepatology523337201010.1002/hep.2362420578254
|
|
39.
|
M HondaA SakaiT YamashitaHepatic ISG
expression is associated with genetic variation in interleukin 28B
and the outcome of IFN therapy for chronic hepatitis
CGastroenterology139499509201010.1053/j.gastro.2010.04.04920434452
|
|
40.
|
ES De AraujoH DahariSJ CotlerTJ LaydenAU
NeumannCE MeloAA BaronePharmacodynamics of PEG-IFN-[alpha]-2a and
HCV response as a function of IL28B polymorphism in
HIV/HCV-coinfected patientsJ Acquir Immune Defic
Syndr5695992011
|
|
41.
|
JM DarlingJ AerssensG FanningQuantitation
of pretreatment serum interferon-gamma-inducible protein-10
improves the predictive value of an IL28B gene polymorphism for
hepatitis C treatment
responseHepatology531422201110.1002/hep.2405621254158
|
|
42.
|
T ReibergerK RutterA FerlitschPortal
pressure predicts outcome and safety of antiviral therapy in
cirrhotic patients with HCV infectionClin Gastroenterol
Hepatol9602608201110.1016/j.cgh.2011.03.00221397726
|
|
43.
|
L YangY LuoJ WeiS HeIntegrative genomic
analyses on IL28RA, the common receptor of interferon-λ1, -λ2 and
-λ3Int J Mol Med25807812201020372826
|
|
44.
|
L YangJ WeiS HeIntegrative genomic
analyses on interferon-λs and their roles in cancer predictionInt J
Mol Med252993042010
|
|
45.
|
KK YanM GuirgisT DinhJ GeorgeA DevA LeeA
ZekryTreatment responses in Asians and Caucasians with chronic
hepatitis C infectionWorld J
Gastroenterol1434163420200810.3748/wjg.14.341618528940
|
|
46.
|
CH LiuCJ LiuCL LinPegylated
interferon-alpha-2a plus ribavirin for treatment-naive Asian
patients with hepatitis C virus genotype 1 infection: a
multicenter, randomized controlled trialClin Infect
Dis4712601269200810.1086/592579
|