Introduction
Most advanced high-risk tumors are contraindicated
for conventional treatments, such as surgery, chemotherapy and
radiotherapy, due to the following characteristics: post-operative
recurrence and metastasis (1);
significant functional central organ invasion (2); local lymph node nerve cell
infiltration or multiple metastases (3–5). On
this occasion, symptomatic palliative therapy is preferable in
clinical treatment (6). Due to
direct invasion, tumors oppress neighboring tissues; thus, the
accompanying tumor oppression syndrome leads to great patient
suffering (7–9).
In order to improve therapeutic efficacy for
advanced high-risk tumors, we tried to eliminate the local lesion
by CyberKnife, which was combined with hyperthermia therapy. In the
present study, a retrospective evaluation of short-term outcomes of
patients treated consecutively with CyberKnife was performed to
demonstrate the clinical applicability of CyberKnife for incurable
advanced high-risk tumors. Through CyberKnife therapy, we
controlled the development of tumors, alleviated the clinical
symptoms of patients and reduced adverse reactions.
Patients and methods
Patient characteristics
One hundred and sixty patients with 341 tumor
lesions were recruited; all of them were patients with advanced
high-risk tumors who came to the Center for Tumor Treatment, The
People's Liberation Army 107th Hospital, for palliative treatment
between November 2010 and June 2011. The inclusion criteria were:
i) pathological or radiographic confirmation of stage III–IV
high-risk tumors; ii) performance status (PS) of 1–4 according to
the Eastern Cooperative Oncology Group (ECOG) scale; iii) all the
inclusive patients provided informed consent for detection and
treatment.
One hundred and one patients were male and 59 were
female. All patients were from 6 to 81 years of age, with a mean
age of 53.7. The locations of tumors were 55 head and neck cases,
54 chest cases, 34 abdomen cases and 17 vertebral cases. Included
were a total of 341 lesions and 201 target area plans among all
patients. The number of lesions for each patient ranged from 1 to
24. The largest tumor lesion was 15×9.5×18 cm, while the smallest
was 1×0.5×0.5 cm. Twenty-eight cases were combined with moderate to
severe hydrothorax or ascites, and 49 cases had cerebral edema of
different degrees.
Methods
CT scans (1.25-mm) were conducted soon after the
patients were hospitalized. MRI, PET-CT or DSA image fusion was
performed when necessary. For the organs which usually make large
respiratory amplitude, 1–3 gold markers were placed into the lung,
liver and pancreas, to definitely mark the target areas. We then
outlined the target areas and determined the treatment plan and
therapeutic doses according to the number, volume, location and
stage of the tumor, which were usually delivered in 1–6 fractions,
and the entire treatment was completed in 1 week. The whole doses
ranged from 18 to 60 Gy, with a fractional dose of 4–18 Gy. For
patients with somatic tumors, we subjoined radiofrequency ablation
diathermy of 2 fractions per week after the CyberKnife therapy,
with an equivalent hot dose of 40°C/min.
Outcome evaluation and statistical
analyses
The outcomes were evaluated based on radiographic
examination, radioimmunoassay, ZPS (Zubrod-ECOG-WHO) scores,
changes in ascities and the Objective Efficacy Evaluation Criteria.
Comparisons between short-term outcomes of CyberKnife therapy and
conformal radiotherapy (CRT) were made. Chi-square test was used
for the comparison of the rate between the two samples. Differences
were considered statistically significant with a P-value <0.05.
SPSS 13.0 software was used for statistical analysis.
Results
Radiographic observation
Radiographic study showed tumor shrinkage of
different degrees and even disappearance after CyberKnife therapy
(18 disappeared, 99 exhibited shrinkage, 35 were unchanged and 8
were enlarged). The recent curative effect of CyberKnife therapy in
the radiographic study was 73.13%, and was obviously superior to
CRT (3 disappeared, 65 exhibited shrinkage, 70 were unchanged and
22 were enlarged) according to the statistical analysis.
Radioimmunoassay (RIA)
In 40 patients, the tumor marker reversed trend and
was positively heightened. After CyberKnife therapy, 5 cases became
negative, 15 cases decreased to different degrees and 17 cases were
unchanged, while 3 cases became more positive.
ZPS scores before and after
treatment
After CyberKnife therapy, the ZPS scores of all
patients decreased, accompanied by alleviation of tumor oppression
syndrome and apparent improvement of the quality of life. The
comparison of ZPS scores before and after CyberKnife therapy was
performed using the Wilcoxon's test (P<0.05). Apparent
improvement of ZPS scores occurred after CyberKnife therapy.
Changes in ascities
There were 28 patients who presented with different
degrees of ascites among the 160 cases. Regarding the alleviation
of ascites, CyberKnife treatment was significantly effective in 8
cases (ascites disappeared completely), effective in 11 cases
(>60% ascites disappeared after treatment and no new
complication appeared), while CyberKnife treatment was ineffective
in 9 cases. The total efficacy rate was 67.9%.
Objective efficacy assessment
For patients with advanced high-risk tumors who
received repeated treatment, there was still high palliative
efficacy after CyberKnife therapy. What should be emphasized is
that, although there were no significant changes in radiography,
these patients experienced complete improvement in the quality of
life after CyberKnife therapy. According to the statistical
analysis, CyberKnife therapy is superior to CRT in the aspect of
objective effect assessment.
Discussion
With substantial improvements in radiotherapy
technology, stereotactic body radiotherapy, which allows
dose-intensification, has led to promising treatment outcomes
(10). Cyberknife, the robotic
stereotactic radiosurgery system, which is able to precisely
deliver a high dose of radiation using an excellent synthesis of
modern image-guided localization and a compact robotically
positioned linear accelerator, has unique advantages that make it
dramatically suited for stereotactic radiotherapy of advanced
high-risk tumors (11,13).
However, due to the realization of hypofractions,
larger doses and shorter treatment courses when using CyberKnife
therapy, numerous studies have consequently placed too much
emphasis on the lack of need for patient hospitalization, the short
treatment course and non-toxic side effects (12–14).
We believe that CyberKnife, due to its precision and flexibility,
should be highly individualized, and the blind pursuit of a rapid
treatment course and early discharge from the hospital should be
avoided (15). During the present
study, we found it was extremely necessary to prevent an early
tumor-dissolving response and abnormal bilirubin metabolism due to
the rapid, short-course killing of tumor cells. The study also
discovered that patient neurophil levels suddenly decreased 2 weeks
after CyberKnife therapy. If this had not been discovered in time
and treated efficiently, there would have been serious consequences
for the patients. Therefore, it is necessary for patients with
multiple or large tumors to be hospitalized.
Using a combination of CyberKnife with a variety of
imaging techniques, such as CT, MRI, PET-CT and DSA, an actual
three-dimensional image of tumors or vascular lesions can be
obtained. This provides a good foundation for target area sketching
(16,17). However, to date, most experts still
refer to the traditional radiobiology model (18); a new biological model has yet to be
established. Because of this delay, in China, no uniform treatment
exists even for the same disease (19–21).
Based on the dosage plan, which was designed according to the
linear quadratic model, with the α/β value of early response
tissues set as 10, late response tissue as 3 and conversed by
conventional 2 Gy fractionated radiation, we arrived at a dosage
which was close to the clinical experienced dose. Yet, a difference
with both the clinical practice and foreign reports was noted
(22,23). As a more precise therapy modality,
CyberKnife realizes hypofracted steretactic treatment and abandons
the strict limitation of taking biological effect into
consideration, which is different from ordinary radiotherapy.
(24–27).
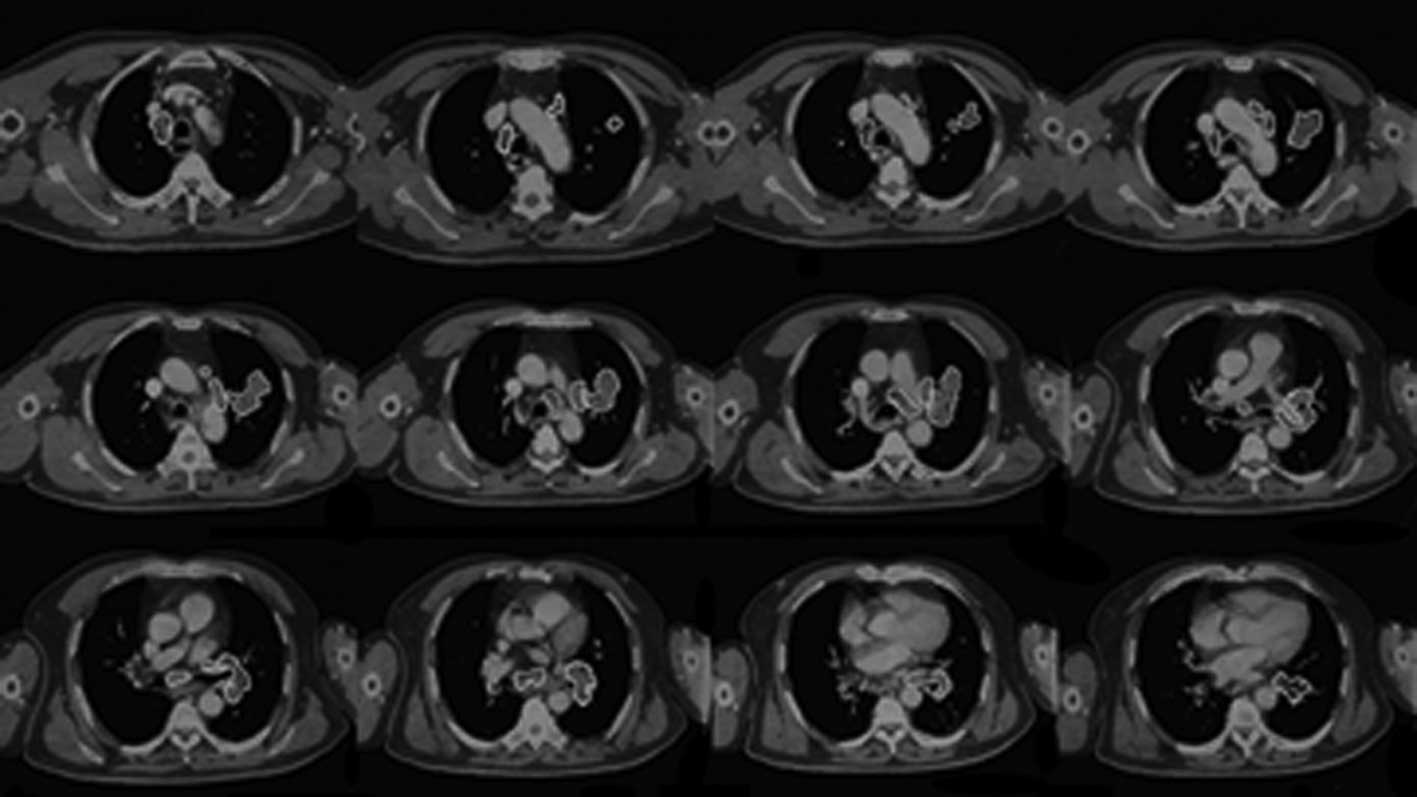
We conclude that CyberKnife is undoubtedly a safer
treatment modality for high-risk or highly difficult cases. One
patient in our study who had lung cancer with mediastinal lymph
node metastases (15 lesions) was definitely a highly difficulty
case. After treatment using CyberKnife, the tumor lesions
completely disappeared (Fig. 1).
After the applied research of CyberKnife in 160 advanced high-risk
(or difficult) tumor cases, we believe that CyberKnife cannot only
quickly improve the clinical symptoms of patients and obtain
satisfactory short-term curative effects, but it is also suitable
for the treatment of high-risk tumors, thus curing the incurable
tumors.
Acknowledgements
This study was partially supported by
grants from the National Special Issue of the Ministry of Health of
China (No. 2009BX042).
References
|
1.
|
Chang BK and Timmerman RD: Stereotactic
body radiation therapy: a comprehensive review. Am J Clin Oncol.
30:637–644. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Shirato H, Shimizu S, Kitamura K and
Onimaru R: Organ motion in image-guided radiotherapy: lessons from
real-time tumor tracking radiotherapy. Int J Clin Oncol. 12:8–16.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Dewas S, Dewas-Vautravers C, Servent V, et
al: Results and special considerations when treating elderly
patients with CyberKnife: a review of 345 cases. Crit Rev Oncol
Hematol. 76:1–7. 2010.PubMed/NCBI
|
|
4.
|
Brown WT, Wu X, Wen BC, et al: Early
results of CyberKnife image-guided robotic stereotactic
radiosurgery for treatment of lung tumors. Comput Aided Surg.
12:253–261. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Bucholz RD, Laycock KA and Cuff LE:
CyberKnife stereo-tactic radiosurgery for intracranial neoplasms,
with a focus on malignant tumors. Technol Cancer Res Treat.
9:541–550. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Nagata Y, Matsuo Y, Takayama K, et al:
Current status of stereo-tactic body radiotherapy for lung cancer.
Int J Clin Oncol. 12:3–7. 2007. View Article : Google Scholar
|
|
7.
|
Yamazaki H, Shiomi H, Tsubokura T, et al:
Quantitative assessment of inter-observer variability in target
volume delineation on stereotactic radiotherapy treatment for
pituitary adenoma and meningioma optic tract. Radiat Oncol.
6:102011.
|
|
8.
|
Hasney CP, Swanton RG and Friendlander PL:
CyberKnife stereotactic radiosurgery for recurrent squamous cell
carcinoma of the head and neck following salvage surgery with close
or positive margins. Laryngoscope. 4:1522010. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Oermann EK, Slack RS, Hanscom HN, et al: A
pilot study of intensity modulated radiation therapy with
hypofractionated stereotactic body radiation therapy (SBRT) boost
in the treatment of intermediate to high-risk prostate cancer.
Technol Cancer Res Treat. 9:453–462. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Unger F, Dominikus K and Haselsberger K:
Stereotactic radiosurgery and fractionated stereotactic
radiotherapy of acoustic neuromas. HNO. 59:31–37. 2011.(In
German).
|
|
11.
|
Alongi F and Di Muzio N: Image-guided
radiation therapy: A new era for the radiation oncologist? Int J
Clin Oncol. 14:568–569. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Schweikard A, Shiomi H and Adler J:
Respiration tracking in radiosurgery. Med Phys. 31:2738–2741. 2004.
View Article : Google Scholar
|
|
13.
|
Jereczed-Fossa BA, Beltramo G, Fariselli
L, et al: Robotic image-guided stereotactic radiotherapy, for
isolated recurrent primary, lymph node or metastatic prostate
cancer. Int J Radiat Oncol Biol Phys. 79:1–9. 2011.PubMed/NCBI
|
|
14.
|
Reichner C, Collins B, Gagnon G, et al:
The placement of gold fiducials for cyberknife stereotactic
radiosurgery using a modified transbronchial needle aspiration
technique. J Bronchol. 12:193–195. 2005. View Article : Google Scholar
|
|
15.
|
Collins BT, Erickson K, Reichner CA, et
al: Radical stereotactic radiosurgery with real-time tumor motion
tracking in the treatment of small peripheral lung tumors. Radiat
Oncol. 2:392007. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Hashizume M: MRI-guided laparoscopic and
robotic surgery for malignancies. Int J Clin Oncol. 12:94–98. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Roh KW, Jang JS, Kim MS, et al:
Fractionated stereotactic radiotherapy as reirradiation for locally
recurrent head and neck cancer. Int J Radiat Onc Biol Phys.
74:1348–1355. 2009. View Article : Google Scholar
|
|
18.
|
King CR, Brooks JD, Gill H, et al:
Stereotactic body radiotherapy for localized prostate cancer:
interim results of a prospective phase II clinical trial. Int J
Radiat Oncol Biol Phys. 73:1043–1048. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Brown WT, Fayad F, Hevezi J, et al:
Individualized higher dose of 70–75 Gy using five-fraction robotic
stereotactic radiotherapy for non-small-cell lung cancer: a
feasibility study. Comput Aided Surg. 16:1–10. 2011.
|
|
20.
|
Vavassori A, Jereczek-Fossa BA, Beltramo
G, et al: Image-guided robotic radiosurgery as salvage therapy for
locally recurrent prostate cancer after external beam irradiation:
retrospective feasibility study on six cases. Tumori. 96:71–75.
2010.
|
|
21.
|
Yoshioka Y: Current status and
perspectives of brachytherapy for prostate cancer. Int J Clin
Oncol. 14:31–36. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Thariat J, Li G, Angellier G, et al:
Current indications and ongoing clinical trials with CyberKnife
stereotactic radiotherapy in France in 2009. Bull Cancer.
96:853–864. 2009.PubMed/NCBI
|
|
23.
|
Xie Y, Djajaputra D, King CR, et al:
Intrafractional motion of the prostate during hypofractionated
radiotherapy. Int J Radiat Oncol Biol Phys. 72:236–246. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Fowler JF, Welsh JS, Howard SP, et al:
Loss of biological effect in prolonged fraction delivery. Int J
Radiat Oncol Biol Phys. 159:242–249. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Fuller DB, Naitoh J, Lee C, et al: Virtual
HDR CyberKnife treatment for localized prostatic carcinoma:
dosimetry comparison with HDR brachytherapy and preliminary
clinical observations. Int J Radiat Oncol Biol Phys. 70:1588–1597.
2008. View Article : Google Scholar
|
|
26.
|
Naito S: Recent developments and
perspectives of image-guided precision surgery for malignant. Int J
Clin Oncol. 12:69–70. 2007. View Article : Google Scholar
|
|
27.
|
Hara W, Loo BW, Goffinet DR, et al:
Excellent local control with stereotactic radiotherapy boost after
external beam radiotherapy in patients with nasopharyngeal
carcinoma. Int J Radiat Oncol Biol Phys. 71:393–400. 2008.
View Article : Google Scholar : PubMed/NCBI
|