Introduction
Hepatocellular carcinoma (HCC) is one of the most
common malignancies and the most common cause of cancer mortality
worldwide (1). The main treatments
may be curative, such as hepatic resection, liver transplantation,
microwave coagulation and radiofrequency ablation, or palliative,
including transarterial chemoembolization (TACE), systemic
chemotherapy and targeted therapy with sorafenib, among others
(2,3). Although much research has been
carried out into the treatment of HCC, the prognosis remains
extremely poor. In this study, we report a case of long-term
survival from primary HCC with early successive lung and adrenal
gland metastasis.
Case report
A 35-year old male was admitted to Zhongnan Hospital
(China) in July 2001 due to a computed tomographic (CT) scan, which
indicated a low density, space-occupying lesion, sized 10.2×9.8 cm
in the right lobe of the liver (Fig.
1), as well as a blood α-fetoprotein (AFP) level of >350
ng/ml. Liver cancer was suspected and no evidence of metastatic
disease was detected. A partial right hepatic lobe resection was
performed on August 23, 2001, and a tumor, sized approximately
12×10×10 cm, was concurrently removed. The pathological report
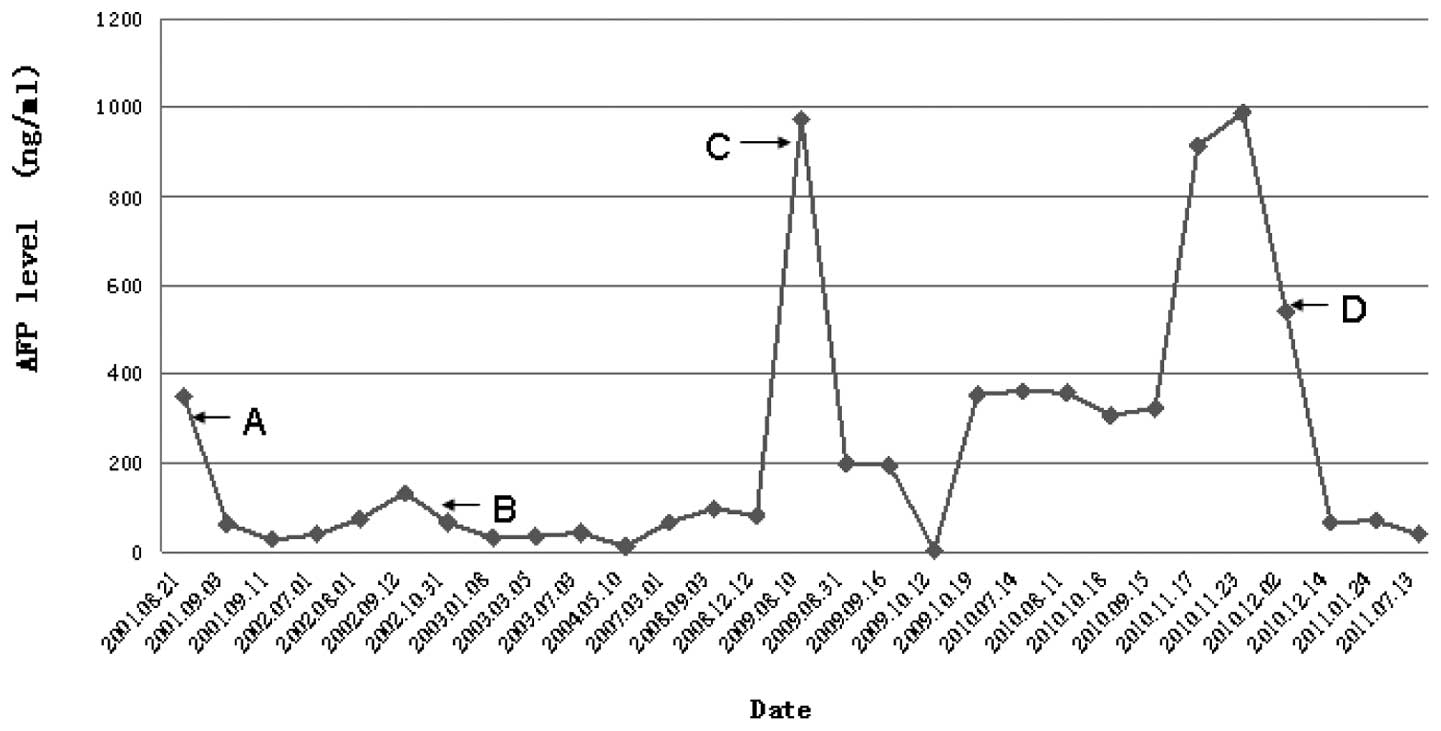
demonstrated a moderate-to-poorly differentiated HCC (Fig. 4A). The blood AFP levels decreased
gradually, reaching 26.47 ng/ml by September 11, 2001 (Fig. 5).
Without any adjuvant therapy, regular follow-ups
were carried out until July 2002, when the blood AFP level
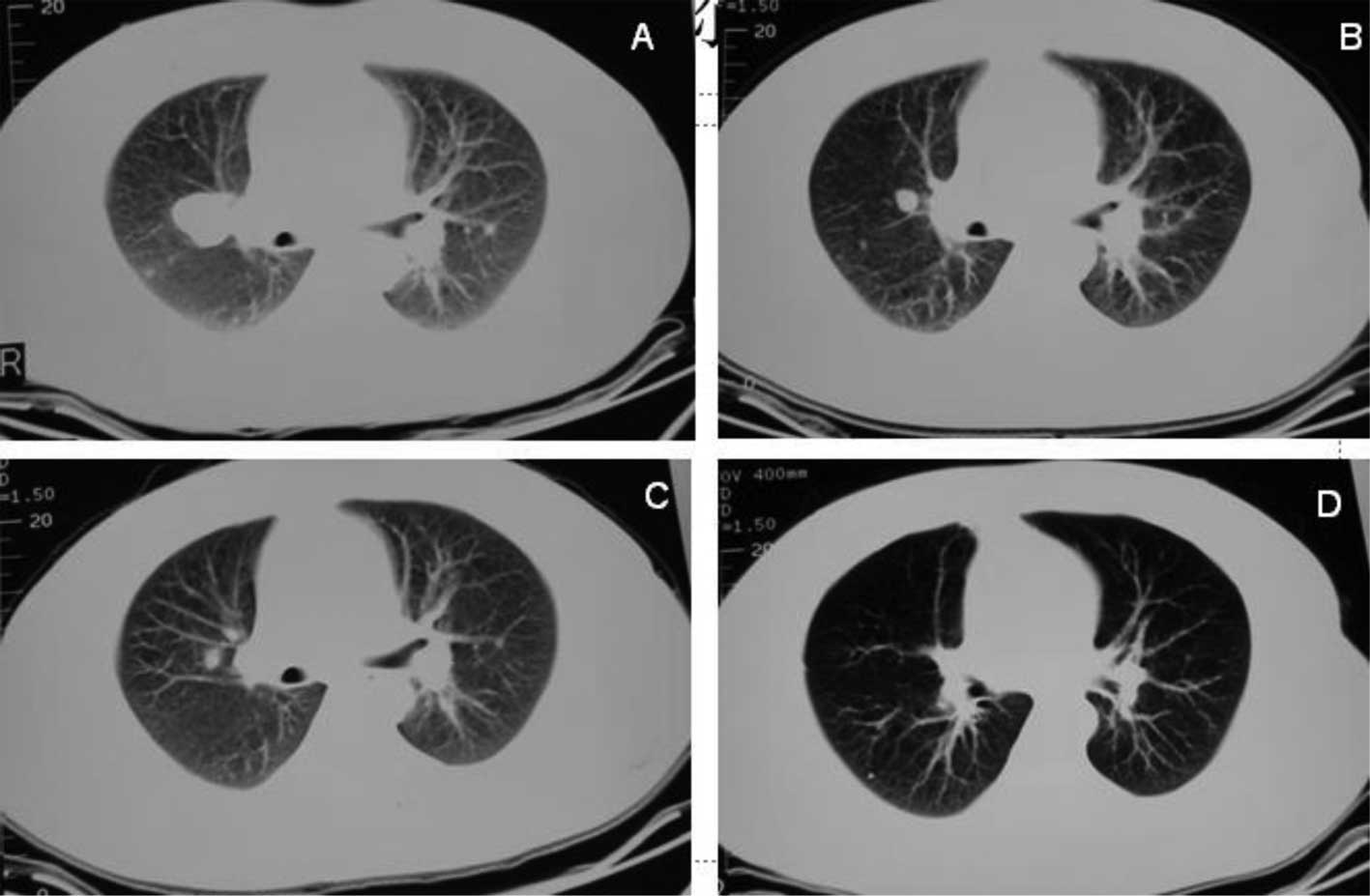
increased to 132.63 ng/ml and a CT scan revealed small nodules in
both lungs, with the largest one (3.5×3.5 cm) in the right
pulmonary hilum (Fig. 2A). No
other metastatic disease was detected. A chemotherapy regimen of
hydroxycamptothecin (HCPT) 10 mg administered intravenously with a
glucose tolerance test (i.v. gtt), on days 1–5 + calcium folinate
(CF) 200 mg i.v. gtt, on days 1–5 + fluorodeoxyuridine (FUDR) 1900
mg i.v. gtt, on days 1–5 + mitomycin c 10 mg i.v., on day 1
(HCPT+CF+FUDR+MMC) was repeated every 3 weeks for 7 cycles between
September 25, 2002 and June 11, 2003, during which time a repeated
CT scan revealed a clear diminution of pulmonary nodules following
the 4th cycle (Fig. 2B), and blood
AFP levels decreased to 34.08 ng/ml by March 5, 2003 (Fig. 5). The therapeutic effect was
partial remission (PR) (Fig. 2C and
D). Later follow-ups revealed a stable disease (SD) until the
CT scan found an enlargement of the pulmonary nodules on May 10,
2004. Another regimen of oxaliplatin (L-OHP) 250 mg i.v. gtt, on
day 1 + FUDR 750 mg i.v. gtt, on days 1–5 + CF 300 mg i.v. gtt, on
days 1–5 (L-OHP+FUDR+CF) was repeated every 3 weeks for 2 cycles
between May 13 and June 3, 2004, and the therapeutic effect was
SD.
Pulmonary nodules remained stable and there was no
evidence of intrahepatic recurrence. Five years later, on June 10,
2009, a CT scan revealed a left adrenal gland mass sized 4.5×4.5 cm
and an increase in blood AFP level to 329.19 ng/ ml. A following
positron emission tomography (PET)/CT scan revealed a locally
hypermetabolic foci in the left adrenal gland, which indicated the
presence of metastatic disease. A laparoscopic left adrenalectomy
was performed on July 14, 2009 and the pathological report revealed
a metastatic hepatoma (Fig. 4B).
Following this, blood AFP levels decreased sharply (Fig. 5). The patient received 2 cycles of
capecitabine 1.5 g, per os (p.o.), twice daily (bid), on
days 1–14 + L-OHP 200 mg, i.v. gtt, on day 1 (XELOX); repeated
every 3 weeks in August and September 2009.
On September 16, 2009, a CT scan found an enlarged
pulmonary nodule of 2.5×2.5 cm near the left cardiac border, with
no change in the remaining lesions (Fig. 3A), and blood AFP levels were 193.44
ng/ml. A 3-dimensional conformal radiation therapy (3DCRT) was
administered (total dose, 57.5 Gy/2.5 Gy/23 F) to the pulmonary
nodule near the left cardiac border between September 24, and
November 23, 2009, during which time the patient received 2 cycles
of irinotecan 280 mg i.v. gtt, on day 1; CF 300 mg i.v. gtt, on
days 1–2; fluorouracil 750 mg i.v. gtt, on days 1–2; fluorouracil
1000 mg by continuous intravenous infusion (CIV), on days 1–2
(FOLFIRI); repeated every 2 weeks. A CT scan on December 9, 2009
revealed that the pulmonary nodule near the left cardiac border was
clearly diminished (Fig. 3B and
C). The later follow-ups revealed SD until the CT scan found an
enlargement of the left lung nodule below the chest wall. On
November 26, 2010, it was found that the left upper lung nodule had
grown up to 29 mm in diameter; no other clear metastasis was noted.
The blood AFP levels increased to 540.55 ng/ml. A video-assisted,
thoracoscopic left upper pulmonary wedge resection was performed on
December 2, 2010 and the pathological report demonstrated a
metastatic HCC (Fig. 4C). The
blood AFP levels following surgery decreased gradually from 181.9
ng/ml on December 6, 2010 to 37.5 ng/ml on July 13, 2011 (Fig. 5).
Throughout the course of the disease, the blood AFP
was very sensitive to the treatment, especially to the operations
(Fig. 5). Since the disease was
founded, the patient had a good performance status and Child-Pugh A
disease. With regard to personal history, a liver disease of
Schistosomiasis japonic was diagnosed and cured in 1997, hepatitis
B was diagnosed in 2001, and the patient had a long history of
smoking (10 cigarettes per day for 20 years). There was no other
special personal or family history.
Discussion
Primary liver cancer, HCC being the major subtype,
is one of the most common malignancies and the most common cause of
cancer mortality worldwide (1). An
estimated 748,300 new cases and 695,900 cancer fatalities occurred
worldwide in 2008, half of which were in China (4). Viral infection is the most common
cause of HCC, in which hepatitis B virus (HBV) and hepatitis C
virus (HCV) infections account for approximately 60 and 33% of the
total liver cancer cases in developing countries, respectively;
whereas these account for 23 and 20% of cases in developed
countries (5,6). Metastases are common in patients with
HCC. The frequent sites of extrahepatic metastasis include the
lung, abdominal lymph node, adrenal gland and bone (7,8).
Although much research has been carried out into the treatment of
HCC, the prognosis remains extremely poor. For patients at early
stages of the disease, well-selected, 5-year survival rates may
increase to 60–70%, and for those at advanced stages, there is as
yet no benefit of survival from systemic therapies (9).
With great improvement of survival results following
hepatic surgery, hepatic resection remains the main therapy for
those early-stage HCC patients who are not suitable for liver
transplantation (10). Ikai et
al reported the 15th follow-up survey of primary liver cancer
in 6,785 HCC patients with cirrhosis who underwent hepatic
resection between 1988 and 1999, the 1-, 3-, 5- and 10-year
survival rates were 85, 64, 45 and 21%, respectively (11). Liver transplantation is the optimal
treatment approach for those strictly selected patients with
unresectable disease. It is based on the Milan criteria, which
supports transplantation in the setting of 1 lesion of ≤5 cm or up
to 3 lesions of ≤3 cm in diameter (12).
Compared to other neoplasms, HCC is resistant to
most conventional chemotherapeutic agents. Monotherapy, mainly with
anthracyclines, including doxorubicin and 4′-epidoxorubicin, may
obtain a response rate of 10–15% (13). Combined chemotherapy has also been
explored. Urabe et al reported an objective response rate
[complete response (CR)+PR] of 46.7% in 16 patients administered
combination therapy with methotrexate, 5-fluorouracil, cisplatin
and interferon-α-2b (14). A phase
II study of combined chemotherapy containing new agents, such as
gemcitabine, L-OHP and bevacizumab in 33 patients with HCC reported
an objective response rate of 20% (15). However, these results should be
confirmed by further large-scale, multi-center, randomized,
controlled trials.
In recent years, targeted therapies have been
intensively researched. There are studies showing that the
multi-kinase inhibitor, sorafenib, may potentially be effective in
the treatment of HCC. In the multicenter, phase III, double-blind,
placebo-controlled Sorafenib HCC Assessment Randomized Protocol
(SHARP) Trial in patients with advanced HCC, who had not received
previous systemic treatment, Josep et al reported that the
median survival and the time to radiological progression were
almost 3 months longer for patients treated with sorafenib (n=299)
than for those administered the placebo (n=303; 10.7 months in the
sorafenib group vs. 7.9 months in the placebo group; hazard ratio
in the sorafenib group, 0.69; 95% confidence interval, 0.55–0.87;
P<0.001). However, the median time to symptomatic progression
between the two groups revealed no significant difference. Other
agents, including mapatumumab, bevacizumab and erlotinib, among
others, which show potential effects are also in their early
research phase (16–18).
Despite the fact that patients with HCC generally
experience very poor outcomes, there are unique examples that
present us with long-term survivors of HCC following combined
treatment. Shirabe et al report a case of 8 years and 9
months with a resectable solitary peritoneal recurrence at the site
of the incision following initial hepatic resection for ruptured
HCC (19). Schreibman et al
reported another case of 9 years and 9 months with recurrent HCC
6.5 years following liver transplantation (20). In a study of the
clinicopathological features of patients surviving for more than 20
years following resection for HCC, Zhou et al reported that
53 cases survived for more than 20 years, in which the longest case
survived for 43 years and 2 months and another survived for 37
years, free of disease (21).
In this study, we report a case of primary HCC with
metastatic disease in the lungs and left adrenal gland, and
comprehensive treatments, including partial hepatic resection,
systemic chemotherapy, radiotherapy for the metastatic mass in the
left lung, left adrenalectomy and left upper pulmonary wedge
resection. Although worldide HCC has a poor outcome, in this case,
the patient remained alive and well for 10 years following
diagnosis of the malignancy. Of note, is that despite the early
presentation of metastatic diseases elsewhere, there was no clear
evidence of intrahepatic recurrence of the malignancy throughout
the course of disease, and the patient had Child-Pugh stage A
disease at all times. Of note, the metastatic disease in the lung
was sensitive to chemotherapy and radiotherapy. This indicates that
for certain patients with advanced stage HCC, palliative treatments
may still be benefcial to their survival. Perhaps by deminishing
the burden of the tumor and lowering the clinical stage, the
progression of the disease may be retarded and thus the patient's
quality of life may be improved. Although certain chemotherapeutic
regimens turned out to be effective, there is little evidence, and
this is one of the limitations of our treatments. This area is
therefore worthy of further research. Nevertheless, there remains a
risk of future disease recurrence, and targeted therapy may thus,
be an option. Since HCC remains a major health problem worldwide,
it is crucial that we keep on searching for new approaches for the
recognition and the treatment of HCC.
References
|
1.
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar
|
|
2.
|
Okuda K: Hepatocellular carcinoma. J
Hepatol. 32:225–237. 2000. View Article : Google Scholar
|
|
3.
|
Llovet JM, Burroughs A and Bruix J:
Hepatocellular carcinoma. Lancet. 362:1907–1917. 2003. View Article : Google Scholar
|
|
4.
|
Ferlay J, Shin HR, Bray F, Forman D,
Mathers C and Parkin DM: Estimates of worldwide burden of cancer in
2008: GLOBOCAN 2008. Int J Cancer. 127:2893–2917. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Raza SA, Clifford GM and Franceschi S:
Worldwide variation in the relative importance of hepatitis B and
hepatitis C viruses in hepatocellular carcinoma: a systematic
review. Br J Cancer. 96:1127–1134. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Parkin DM: The global health burden of
infection-associated cancers in the year 2002. Int J Cancer.
118:3030–3044. 2006.PubMed/NCBI
|
|
7.
|
Katyal S, Oliver JR, Peterson MS, Ferris
JV, Carr BS and Baron RL: Extrahepatic metastases of hepatocellular
carcinoma. Radiology. 216:698–703. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Kummar S and Shafi NQ: Metastatic
hepatocellular carcinoma. Clin Oncol (R Coll Radiol). 15:288–294.
2003. View Article : Google Scholar
|
|
9.
|
Lopez PM, Villanueva A and Llovet JM:
Systematic review: evidence-based management of hepatocellular
carcinoma - an updated analysis of randomized controlled trials.
Aliment Pharmacol Ther. 23:1535–1547. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Belghiti J, Cortes A, Abdalla EK,
Régimbeau JM, Prakash K, Durand F, Sommacale D, Dondero F, Lesurtel
M, Sauvanet A, Farges O and Kianmanesh R: Resection prior to liver
transplantation for hepatocellular carcinoma. Ann Surg.
238:885–893. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Ikai I, Itai Y, Okita K, Omata M, Kojiro
M, Kobayashi K, Nakanuma Y, Futagawa S, Makuuchi M and Yamaoka Y:
Report of the 15th follow-up survey of primary liver cancer.
Hepatol Res. 28:21–29. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Mazzaferro V, Regalia E, Doci R, Andreola
S, Pulvirenti A, Bozzetti F, Montalto F, Ammatuna M, Morabito A and
Gennari L: Liver transplantation for the treatment of small
hepatocellular carcinomas in patients with cirrhosis. N Engl J Med.
334:693–699. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Lai EC and Lau WY: The continuing
challenge of hepatic cancer in Asia. Surgeon. 3:210–215. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Urabe T, Kaneko S, Matsushita E, Unoura M
and Kobayashi K: Clinical pilot study of intrahepatic arterial
chemotherapy with methotrexate, 5-fluorouracil, cisplatin and
subcutaneous interferon-alpha-2b for patients with locally advanced
hepatocellular carcinoma. Oncology. 55:39–47. 1998. View Article : Google Scholar
|
|
15.
|
Zhu AX, Blaszkowsky LS, Ryan DP, Clark JW,
Muzikansky A, Horgan K, Sheehan S, Hale KE, Enzinger PC, Bhargava P
and Stuart K: Phase II study of gemcitabine and oxaliplatin in
combination with bevacizumab in patients with advanced
hepatocellular carcinoma. J Clin Oncol. 24:1898–1903. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Hotte SJ, Hirte HW, Chen EX, Siu LL, Le
LH, Corey A, Iacobucci A, MacLean M, Lo L, Fox NL and Oza AM: A
phase 1 study of mapatumumab (fully human monoclonal antibody to
TRAIL-R1) in patients with advanced solid malignancies. Clin Cancer
Res. 14:3450–3455. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Siegel AB, Cohen EI, Ocean A, Lehrer D,
Goldenberg A, Knox JJ, Chen H, Clark-Garvey S, Weinberg A, Mandeli
J, et al: Phase II trial evaluating the clinical and biologic
effects of bevacizumab in unresectable hepatocellular carcinoma. J
Clin Oncol. 26:2992–2998. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Thomas MB, Chadha R, Glover K, Wang X,
Morris J, Brown T, Rashid A, Dancey J and Abbruzzese JL: Phase 2
study of erlotinib in patients with unresectable hepatocellular
carcinoma. Cancer. 110:1059–1067. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Shirabe K, Kitamura M, Tsutsui S, Maeda T,
Matsumata T and Sugimachi K: A long-term survivor of ruptured
hepatocellular carcinoma after hepatic resection. J Gastroenterol
Hepatol. 10:351–354. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Schreibman IR, Bejarano P, Martinez EJ and
Regev A: Very late recurrence of hepatocellular carcinoma after
liver transplantation: case report and literature review.
Transplant Proc. 38:3140–3143. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Zhou XD, Tang ZY, Ma ZC, Fan J, Wu ZQ, Qin
LX, Zhou J, Yu Y, Sun HC and Qiu SJ: Twenty-year survivors after
resection for hepatocellular carcinoma-analysis of 53 cases. J
Cancer Res Clin Oncol. 135:1067–1072. 2009.PubMed/NCBI
|