Introduction
Endometrial biopsy is a common procedure for the
investigation of many gynecological disorders, including abnormal
uterine bleeding, postmenopausal bleeding, abnormal cytology and
infertility (1,2). The majority of women experience some
degree of discomfort and pain during the procedure. Pain may occur
during dilatation of the cervix for insertion of the catheter and
during endometrial biopsy, which further aggravates pain by
inducing uterine contraction (1,2).
The paracervical block relieves pain in the lower
part of the uterus and cervix by blocking nerve impulses that are
conveyed through the Frankenhäuser plexus. However, it may not be
effective for pain in the upper part of the uterus, which has a
different innervation. Intrauterine anesthesia, by the infusion of
a local anesthetic into the uterine cavity, has a theoretical
action by blocking nerve endings in the uterine corpus and fundus
(3,4).
The effectiveness of intrauterine anesthesia for
pain relief in gynecological procedures that involve the uterine
cavity has been demonstrated in many studies (5–9). The
intrauterine instillation of a topical anesthetic is easy,
relatively painless, and promising for adequate analgesia during
endometrial biopsy. This technique could be an ideal method of
anesthesia for endometrial biopsies.
Levobupivacaine is a long-acting local anesthetic
agent. Levobupivacaine takes a while to take effect; however, it
has a longer duration of action.
The goal of this study was to determine pain during
endometrial biopsy by comparing the intrauterine instillation of
levobupivacaine or paracervical block with a placebo in a
randomized, double-masked trial in premenopausal and postmenopausal
women. Also types and incidence of possible adverse events were
reported.
Materials and methods
Study population and exclusion/inclusion
criteria
This was a randomized, placebo-controlled trial
carried out in the Obstetrics and Gynecology Department, Faculty of
Medicine, Fatih University, Turkey between September 2009 and July
2010. The aim of this study was to compare the efficacy of
intrauterine levobupivacaine instillation, paracervical block and a
placebo for pain control in patients undergoing endometrial biopsy.
The study was approved by the human ethics committee of the
university. The study population comprised women with abnormal
uterine bleeding who were scheduled for endometrial curettage or
women who would have control biopsies before surgery due to other
pathologies. Patients who were virgins, or those who had an
American Society of Anesthesiologists (ASA) physical status class
of >II, acute cervicitis, profuse uterine bleeding, known
allergy to levobupivacaine, a history of impaired liver function,
were pregnant, had cervical stenosis or vaginismus or were unable
to understand how to score a 10-cm visual analog scale (VAS) pain
score were excluded from the study. Suitable patients were informed
as regards the study protocol and signed informed consent was
obtained from all patients.
A total of 90 women were included in the study.
Before the procedure, patient demographics such as age, gravida,
parity, menopausal status and biopsy indications were recorded.
Endometrial thickness in patients was measured by transvaginal
sonography before the procedure. Patients were allocated to either
the control or case groups by simple randomization prior to
endometrial biopsy. Group 1 comprised cases with intrauterine
anesthesia with 5 ml 0.5% levobupivacaine (Chirocaine; Abbott,
Tipperary, Republic of Ireland). Group 2 comprised patients who
underwent paracervical block with lidocaine (Aritmal ampule 2%;
Biosel, Istanbul, Turkey). No analgesic agent was given to the
remaining 30 patients; these cases comprised the control group.
Biopsies
Biopsies were carried out with the Pipelle (Unimar,
Wilton, CT, USA), a flexible plastic 3.1-mm diameter catheter. The
same technique was used to sample the endometrium by resident
doctors to minimize the risk of technical variation.
The procedures were performed under the aseptic
technique as follows: the patient was placed in a modified
lithotomy position. A sterile bivalve speculum was introduced into
the vagina for visualization of the cervix. The cervix and vagina
were then cleansed with betadine solution (Betadine; Purdue Pharma
LP, Stamford, CT, USA). Each patient in group 1 received an
intrauterine injection of 0.5% levobupivacaine before endometrial
sampling. The solution (5 ml) was instilled through the endocervix
into the uterine cavity using an 18-gauge angiocatheter. The
angiocatheter was left in place for 15 min before it was withdrawn
to decrease backflow and allow the anesthetic to take effect. In
group 2, paracervical block was performed with 5 ml 2% lidocaine
solution. Local anesthetic was applied at 0.5–1 cm depth of the
cervicovaginal junction at the four and eight o'clock positions
without application of tenaculum to the cervix. We waited for 5 min
before endometrial sampling to allow the anesthetic to take effect.
No anesthetic was given to the control group. The Pipelle was
pushed into the uterine cavity for three passes to ensure complete
sampling in all patients.
All patients were observed for 60 min in a recovery
room. None of the patients enrolled in the study had received any
oral or parenteral analgesic drugs. All tissue specimens were sent
for cytopathological examination. All tissue specimens were
analyzed by pathologists who were blinded to the test solution.
VAS pain ratings
The primary outcome measures were pain or discomfort
experienced during the procedure. Pain was assessed using a 10-cm
visual analogue pain scale. Patients were asked to rate their pain
levels on a VAS, marking an ‘X’ on a 10-cm line (0 cm, no pain; 10
cm, unbearable pain). The pain score was measured during the
uterine curettage. To control for possible confounding as the
result of a nonequal distribution of women with insertional pain,
we excluded those subjects who experienced pain from speculum
insertion. In those cases where the patient had intolerable pain,
the procedure was terminated immediately, and the pain score was
recorded. Scores were measured from the left and recorded. All
observed adverse effects were recorded until the patients were
discharged.
Statistical analysis
The statistical analyses were carried out using the
SPSS 15.0 statistical software package. Following the entering of
patient data into the computer, all the necessary diagnostic checks
and corrections were performed. The conformity of the measured
values to normal distribution was examined graphically and using
the Shapiro-Wilk test. In presenting descriptive statistics,
numbers and percentages were used for categorical variables, and
median [interquartile range (IQR)] values were used for the data.
For the comparison of normally distributed data, ANOVA and post hoc
Bonferoni tests were used. The Kruskal-Wallis test and the
Bonferoni-corrected Mann-Whitney test were used to compare the data
that was not distributed normally. Spearman's correlation analysis
was used for parameters that affect pain scores. A two-tailed
p-value of <0.05 was considered to indicate a statistically
significant difference.
Results
A total of 90 women were included in the study and
divided into three groups (30 cases per group) randomly. Mean age,
gravida, parity, and menopausal status of the women in the three
groups were similiar. Endometrial thickness in patients was
measured by transvaginal sonography before the procedure.
Endometrial thickness was significantly lower in Group 2 than group
1 and the control group. The demographic and clinical
characteristics of the groups are summarized in Table I.
 | Table I.Demographic and clinical
characteristics of the groups. |
Table I.
Demographic and clinical
characteristics of the groups.
| Characteristic | Levobupivacaine
(n=30) | Paracervical block
(n=30) | Control (n=30) | p-value |
|---|
| Age (years; mean ±
SD) | 44.6±7.9 | 45.3±10.4 | 47.8±9.2 | 0.256 |
| Gravida [n; median
(IQR)] | 3 (2) | 2 (3) | 3 (2) | 0.412 |
| Parity [n; median
(IQR)] | 2 (1) | 2 (2) | 2 (1) | 0.532 |
| Menopausal
status | | | | |
| Premenopause
(%) | 24 (80.0) | 23 (76.7) | 23 (76.7) | 0.938 |
| Postmenopause
(%) | 6 (20.0) | 7 (23.3) | 7 (23.3) | |
| Endom. thickness | | | | |
| <5 mm (%) | 8 (26.7) | 1 (3.3) | 9 (30.0) | 0.019a |
| ≥5 mm (%) | 22 (73.3) | 29 (96.7) | 21 (70.0) | |
When groups were compared for biopsy indications,
there was no difference between groups. Endometrial biopsy due to
hypermenorrhea was higher in the levobupivacaine group. Control
biopsy prior to surgery due to other gynecological pathologies was
higher in group 2 and the control group (p=0.003 vs. p=0.002,
respectively) than in group 1 (Table
II).
 | Table II.Biopsy indications according to
groups. |
Table II.
Biopsy indications according to
groups.
| Biopsy
indication | Levobupivacaine n
(%) | Paracervical n
(%) | Control n (%) | p-value |
|---|
| Menorrhagia | 7 (23.3 | 3 (10.0) | 4 (13.3) | 0.343 |
| Metrorrhagia | 3 (10.0 | 3 (10.0) | 1 (3.3) | 0.492 |
| Menometrorrhagia | 7 (23.3) | 10 (33.3) | 12 (40.0) | 0.380 |
| Postmenopausal
bleeding | 6 (20.0) | 7 (23.3) | 6 (20.0) | 0.935 |
| Hypermenorrhea | 5 (16.7) | 0 (0.0) | 0 (0.0) | 0.003a |
| Polymenorrhea | 2 (6.7) | 0 (0.0) | 0 (0.0) | 0.106 |
| Pre-op control | 0 (0.0) | 7 (23.3) | 7 (23.3) | 0.002a |
| Total | 30 (100.0) | 30 (100.0) | 30 (100.0) | 0.944 |
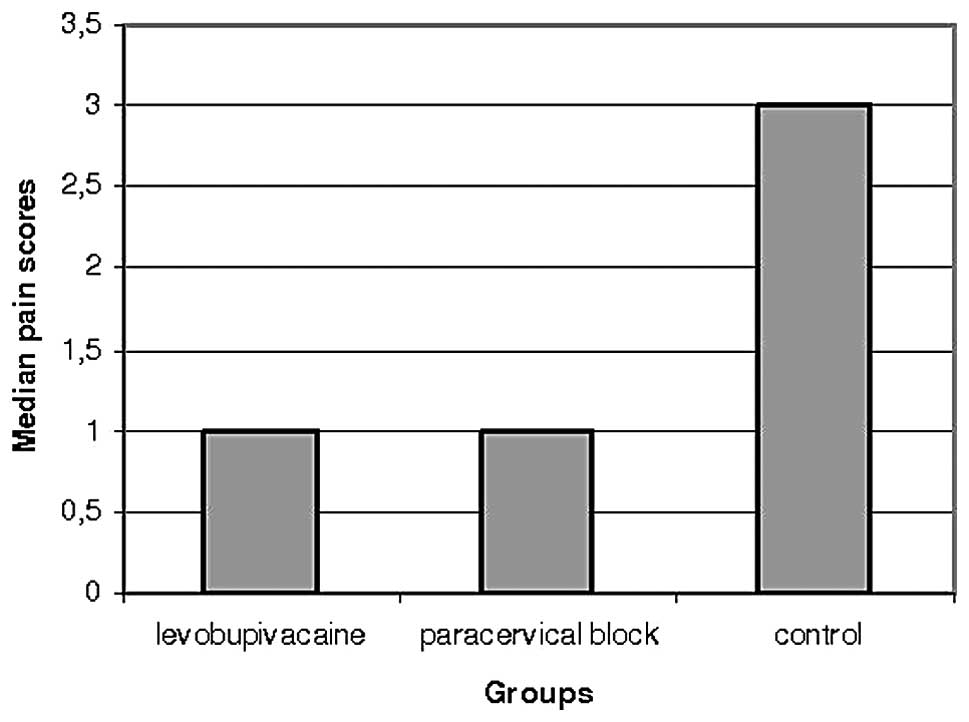
When pain scores between the groups were compared,
scores in the intrauterine levobupivacaine and paracervical block
groups were found to be significantly lower than those in the
control group (Fig. 1) (Z=2.761;
p=0.006 vs. Z=3.310; p=0.001, respectively). There was no
difference between the levobupivacaine and paracervical block
groups in terms of pain scores (Fig.
2) (Z=0.305; p=0.760). The distribution of pain scores among
the groups is shown in Table
III.
 | Table III.Distribution of pain scores by
group. |
Table III.
Distribution of pain scores by
group.
| Pain score | Levobupivacaine n
(%) | Paracervical block n
(%) | Control n (%) | p-value |
|---|
| 0 | 9 (30.0) | 8 (26.7) | 2 (6.7) | 0.057 |
| 1 | 9 (30.0) | 10 (33.3) | 4 (13.3) | 0.164 |
| 2 | 5 (16.7) | 5 (16.7) | 5 (16.7) | 1.000 |
| 3 | 3 (10.0) | 0 (0.0) | 6 (20.0) | 0.011a |
| 4 | 1 (3.3) | 0 (0.0) | 5 (16.7) | 0.016 |
| 5 | 1 (3.3) | 3 (10.0) | 2 (6.7) | 0.572 |
| 6 | 0 (0.0) | 2 (6.7) | 2 (6.7) | 0.189 |
| 7 | 0 (0.0) | 1 (3.3) | 2 (6.7) | 0.242 |
| 8 | 2 (6.7) | 0 (0.0) | 1 (3.3) | 0.242 |
| 9 | 0 (0.0) | 1 (3.3) | 0 (0.0) | 0.330 |
| 10 | 0 (0.0) | 0 (0.0) | 1 (3.3) | 0.330 |
| Median (IQR) | 1 (2.25) | 1 (2.75) | 3 (3) | 0.002b |
There was a marked positive correlation between
biopsy indications and pain scores (rho = 0.648; p<0.001). Pain
scores were lower in cases with the indication of polymenorrhea,
hypermenorrhea and metrorraghia than those with other indications.
There was mild positive correlation between pain scores and type of
anesthesia used (rho = 0.344; p=0.001) (Table IV).
 | Table IV.Correlation analysis of parameters
that affect pain score. |
Table IV.
Correlation analysis of parameters
that affect pain score.
| Age | Gravida | Parity | Indication | Endometrial
thickness | Type of
anesthesia | Pain score |
|---|
| Age | | | | | | | |
| Rho | - | 0.454a | 0.361 | 0.361 | 0.026 | 0.321 | 0.189 |
| p-value | - | 0.026 | 0.083 | 0.050 | 0.891 | 0.142 | 0.317 |
| Gravida | | | | | | | |
| Rho | 0.454a | - | 0.633a | 0.557a | 0.152 | 0.183 | 0.083 |
| p-value | 0.026 | - | 0.001 | 0.005 | 0.479 | 0.212 | 0.699 |
| Parity | | | | | | | |
| Rho | 0.361 | 0.633a | - | 0.342 | 0.053 | 0.243 | 0.188 |
| p-value | 0.083 | 0.001 | - | 0.102 | 0.805 | 0.156 | 0.380 |
| Indication | | | | | | | |
| Rho | 0.361 | 0.557a | 0.342 | - | 0.257a | 0.026 | 0.648a |
| p-value | 0.050 | 0.005 | 0.102 | - | 0.014 | 0.809 | <0.001 |
| p-value | 0.571 | 0.164 | 0.218 | 0.401 | <0.001 | 0.211 | 0.709 |
| Endometrial
thickness | | | | | | | |
| Rho | 0.026 | 0.152 | 0.053 | 0.257a | - | 0.034 | 0.172 |
| p-value | 0.891 | 0.479 | 0.805 | 0.014 | - | 0.750 | 0.104 |
| Type of
anesthesia | | | | | | | |
| Rho | 0.154 | 0.085 | 0.112 | 0.026 | 0.034 | - | 0.344a |
| p-value | 0.412 | 0.622 | 0.521 | 0.809 | 0.750 | - | 0.001 |
| Pain score | | | | | | | |
| Rho | 0.189 | 0.083 | 0.188 | 0.648a | 0.172a | 0.344a | - |
| p-value | 0.317 | 0.699 | 0.380 | <0.001 | 0.104 | 0.001 | - |
The majority of the biopsy results were
proliferative (n=28; 31.1%) and secretory (n=19; 21.1%)
endometrium. Simple hyperplasia was found only in three cases
(3.3%). Due to insufficient material, inconclusive results were
observed in the control and paracervical groups (n=6; 20% for each
group) (Table V).
 | Table V.Histopathological results of
cases. |
Table V.
Histopathological results of
cases.
| Endometrial biopsy
results | Levobupivacaine n
(%) | Paracervical n
(%) | Control n (%) | Total n (%) |
|---|
| Simple
hyperplasia | 1 (3.3) | 0 (0.0) | 1 (3.3) | 2 (2.2) |
| Proliferative
endometrium | 12 (10.0) | 5 (13.4) | 11 (33.4) | 28 (31.1) |
| Secretory
endometrium | 6 (20.0) | 6 (20.0) | 7 (23.3) | 19 (21.1) |
| Endometrial
polyp | 2 (6.7) | 0 (0.0) | 0 (0.0) | 2 (2.2) |
| Stromal glandular
destruction | 3 (10.0) | 0 (0.0) | 0 (0.0) | 3 (3.3) |
| Chronic
endometritis | 1 (3.3) | 5 (16.6) | 2 (6.7) | 8 (8.9) |
| Menstrual
endometrium | 3 (10.0) | 0 (0.0) | 0 (0.0) | 3 (3.3) |
| Endometrial tissue
fragments | 2 (6.7) | 1 (3.3) | 1 (3.3) | 4 (4.5) |
| Endometrium under
drug effect | 0 (0.0) | 3 (10.0) | 2 (6.7) | 5 (5.6) |
| Atrophic
endometrium | 0 (0.0) | 2 (6.7) | 0 (0.0) | 2 (2.2) |
| Blood, fibrin and
mucus | 0 (0.0) | 2 (6.7) | 0 (0.0) | 2 (2.2) |
| Insufficient
material | 0 (0.0) | 6 (20.0) | 6 (20.0) | 12 (13.3) |
| Total | 30 (100.0) | 30 (100.0) | 30 (100.0) | 90 (100.0) |
Discussion
Endometrial biopsy is one of the essential but
painful procedures of gynecology. Procedural pain appears to arise
from two separate anatomical structures, the cervix and the uterus.
The cervix and uterus are richly innervated and pain perception
from the cervix and the corpus of the uterus appears to pass
through two distinct neural pathways; Frankenhäuser plexus
(parasympathetic S2-4) supplying the cervix and lower uterus, and
sympathetic nerves via the infundibulopelvic ligament from the
ovarian plexus supplying the uterine fundus (3,4).
Procedural pain may occur during dilatation of the
cervix for insertion of the catheter and during endometrial biopsy,
which further aggravates pain by inducing uterine contraction. The
paracervical block aids in decreasing pain from cervical origin
(10–12). However, it has been found to be
ineffective in reducing pain arising from the uterine corpus and
carries a risk of inducing bradycardia, hypotension, convulsion,
respiratory arrest, and death (13,14).
On the other hand, a local or topical anesthetic injected into the
uterine cavity may inhibit nerve responses and decrease pain
primarily arising from the body of the uterus.
There is controversy over the efficacy of
transcervical intrauterine anaesthesia. Previous studies have
investigated the use of different local anesthetics (i.e.,
lidocaine, mepivacaine) to lessen the pain experienced with
endometrial biopsy and other intrauterine procedures such as
hysteroscopy, fractional curettage, hysterosalpingography (HSG) and
removal of a lost intrauterine device (IUD) (6–9). The
intrauterine instillation of local anesthetic has variously been
reported to be ineffective or effective in reducing pain when
compared with saline in randomised trials (6,7,15–17).
However, in the majority of studies, local anesthetic injected into
the uterine cavity has been demonstrated to be effective in
decreasing patient pain associated with these intrauterine
procedures.
A study of a 2-ml infusion of 2% lidocaine, in
addition to oral naproxen sodium, prior to HSG demonstrated no
reduction in pain and the possibility of increased postprocedural
pain (18). Also, in the study by
Zupi et al (6), with 45
women, no statistically significant reduction in pain was
found.
In another study, Guney et al (19) compared the effects of a local
anesthetic and placebo for the removal of a ‘lost’ IUD. A
significant difference was found in terms of pain reduction with
the use of intrauterine topical local anesthetic either during or
immediately after the procedure. However, perception of pain at 20
min after the procedure was significantly higher in the lidocaine
group compared with the placebo group.
Cicinelli et al (7) randomly assigned 80 women to receive 2
ml of 2% mepivacaine or normal saline with a 5-min delay before an
office hysteroscopy and/or endometrial biopsy. Their results showed
a statistically significant reduction in pain in women receiving
the mepivacaine infusion. They reported considerably higher (32.5%)
incidence of vasovagal reaction in their placebo group. Similar
results were observed by Dogan et al (9). They found that the combination of
local lidocaine and oral naproxen sodium significantly reduced
patient discomfort during an endometrial biopsy.
Trolice et al (8) randomly assigned 57 perimenopausal and
postmenopausal women to receive either intrauterine lidocaine or
normal saline before having an office endometrial biopsy. Five
milliliters of 2% lidocaine were infused with a 3-min time delay
before obtaining the biopsy. They found a statistically significant
reduction in pain in women receiving the lidocaine infusion. They
concluded that local anesthetic injected into the uterine cavity is
effective in decreasing patient pain associated with these
intrauterine procedures.
The time interval allowed for the local anesthetic
to become effective is also important. The peak anesthetic effect
following topical application of 1% lidocaine occurs within 10 min
(20). Edelman et al
(20) randomly assigned 80 women
to receive 10 ml 1% lidocaine or saline with a 3-min delay in
first-trimester abortions and did not observe a reduction in pain
during or after suction aspiration. The 3-min waiting period may be
too short. It is also possible that tubal extravasation of
high-dose lidocaine might have caused peritoneal irritation. In our
study, as explained in Materials and methods, we waited 5 min
following the injection of lidocaine and 15 min following the
injection of levobupivacaine before removing the catheter. The
volume of anesthetic used in our study was 5 ml.
Rattanachaiyanont et al (21) found statistically significant
reductions in pain when a combination of paracervical block and
intrauterine anesthesia was used before fractional curettage. We
did not apply paracervical block, as cervical dilation was not
necessary in our patients. Cases with cervical stenosis who
required cervical dilation were excluded from the study.
Since pain is a subjective symptom, it is difficult
to evaluate and anxiety may be a potential confounder. Ethnic and
cultural differences between the patients may affect pain
perception and tolerance. Measurement of anticipatory pain may
therefore be of value in studies on pain for determination of true
pain. It is likely that the speculum insertion measurement is a
surrogate for a patient's overall tolerance of pain and/or anxiety.
Pain with speculum insertion occurs in many conditions such as
dyspareunia, vulvar vestibular syndrome, and vaginismus (21,22).
To control for possible confounding as the result of a nonequal
distribution of women with insertional pain, we excluded those
subjects who experienced pain from speculum insertion.
Endometrial biopsy is an essential office procedure
to collect tissue for histological evaluation of the endometrium.
Patient acceptability and compliance with the procedure may be
difficult due to associated pain. According to our MEDLINE search,
this is the first study to evaluate the efficacy of intrauterine
topical levobupivacaine installation for endometrial biopsy. A
limitation of our study is the small sample number; however,
analysis of our data showed a statistically significant reduction
in pain during endometrial biopsy with intrauterine levobupivacaine
and lidocaine in premenopausal and postmenopausal women, regardless
of parity. Although instillation may lengthen the procedure, the
reduction in patient discomfort outweighs the time factor. Among
the local anesthetic agents, lidocaine has an advantage over
levobupivacaine, as a shorter time is needed for the initiation of
its effects. The intrauterine topical instillation of anesthetic
also did not affect pathology results.
In conclusion, the transcervical intrauterine
topical instillation of levobupivacaine or paracervical block with
lidocaine brings about pain relief during and after endometrial
biopsy. Therefore, it appears to be a beneficial method. However,
further studies with larger series are required to evaluate the
effectiveness of intrauterine anesthesia, for determination of
optimal concentration, volume and waiting time according to local
anesthesia and also for applicability of the method to other
intrauterine procedures.
References
|
1.
|
Chambers JT and Chambers SK: Endometrial
sampling: when? Where? Why? With what? Clin Obstet Gynecol.
35:28–39. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Fothergill DJ, Brown VA and Hill AS:
Histological sampling of the endometrium - a comparison between
formal curettage and the Pipelle sampler. Br J Obstet Gynaecol.
99:779–780. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Rogers RM: Basic pelvic neuroanatomy.
Chronic Pelvic Pain: an Integrated Approach; Steege JF, Metzger DA
and Levy BS: WB Saunders Company; Philadelphia, PA: pp. 31–58.
1998
|
|
4.
|
Moore KL, Dalley AF and Agur AMR: Pelvis
and Perineum Pelvic Viscera In: Clinically Oriented Anatomy. 6th
edition. Lippincott Williams & Wilkins; Baltimore, MD: pp.
362–402. 2010
|
|
5.
|
Cicinelli E, Didonna T, Fiore G, Parisi C,
Matteo M and Castrovilli G: Topical anesthesia for hysteroscopy in
postmenopausal women. J Am Assoc Gynecol Laparosc. 4:9–12. 1996.
View Article : Google Scholar
|
|
6.
|
Zupi E, Luciano AA, Valli E, Marconi D,
Maneschi F and Romanini C: The use of topical anesthesia in
diagnostic hysteroscopy and endometrial biopsy. Fertil Steril.
63:414–416. 1995.PubMed/NCBI
|
|
7.
|
Cicinelli E, Didonna T, Ambrosi G,
Schonauer LM, Fiore G and Matteo MG: Topical anaesthesia for
diagnostic hysteroscopy and endometrial biopsy in postmenopausal
women: a randomised placebo-controlled double-blind study. Br J
Obstet Gynaecol. 104:316–319. 1997. View Article : Google Scholar
|
|
8.
|
Trolice MP, Fishburne C Jr and McGrady S:
Anesthetic efficacy of intrauterine lidocaine for endometrial
biopsy: a randomized double-masked trial. Obstet Gynecol.
95:345–347. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Dogan E, Celiloglu M, Sarihan E and Demir
A: Anesthetic effect of intrauterine lidocaine plus naproxen sodium
in endometrial biopsy. Obstet Gynecol. 103:347–351. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Glantz J and Shomento S: Comparison of
paracervical block techniques during first trimester pregnancy
termination. Intl J Gynecol Obstet. 72:171–178. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Stubblefield P: Control of pain for women
undergoing abortion. Intl J Gynecol Obstet. 3:131–140. 1989.
View Article : Google Scholar
|
|
12.
|
Wiebe E: Comparison of efficacy of
different local anesthetics and techniques of local anesthesia in
therapeutic abortions. Am J Obstet Gynecol. 167:131–134. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Miller L, Jensen MP and Stenchever MA: A
double-blind randomized comparison of lidocaine and saline for
cervical anesthesia. Obstet Gynecol. 87:600–604. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Chanrachakul B, Likittanasombut P,
O-Prasertsawat P and Herabutya Y: Lidocaine versus plain saline for
pain relief in fractional curettage: a randomized controlled trial.
Obstet Gynecol. 98:592–595. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Lau WC, Tam WH, Lo WK and Yuen PM: A
randomised double-blind placebo-controlled trial of transcervical
intrauterine local anaesthesia in outpatient hysteroscopy. Br J
Obstet Gynaecol. 107:610–613. 2000. View Article : Google Scholar
|
|
16.
|
Broadbent JA, Hill NC, Molnar BG, Rolfe KJ
and Magos AL: Randomized placebo controlled trial to assess the
role of intracervical lignocaine in outpatient hysteroscopy. Br J
Obstet Gynaecol. 99:777–779. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Guler A, Kosus A, Kosus N and Sahin HG:
Comparing the efficacy of intrauterine lidocaine and paracervical
block for decreasing pain in endometrial biopsy. J Surg Arts.
2:1–10. 2009.
|
|
18.
|
Costello M, Horrowitz S, Steigrad S, Saif
N, Bennett M and Ekangaki A: Transcervical intrauterine topical
local anesthetic at hysterosalpingography: a prospective
randomized, double-blinded, placebo-controlled trial. Fertil
Steril. 78:1116–1122. 2002. View Article : Google Scholar
|
|
19.
|
Guney M, Oral B and Mungan T: Efficacy of
intrauterine lidocaine for removal of a ‘lost’ intrauterine device.
Obstet Gynecol. 108:119–123. 2006.PubMed/NCBI
|
|
20.
|
Edelman A, Nichols MD, Leclair C, Astley
S, Shy K and Jensen JT: Intrauterine lidocaine infusion for pain
management in first trimester abortions. Obstet Gynecol.
103:1267–1272. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Rattanachaiyanont M, Leerasiri P and
Indhavivadhana S: Effectiveness of intrauterine anesthesia for pain
relief during fractional curettage. Obstet Gynecol. 106:533–539.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Bhatia K, Rustimov O, Adhikary M and Hill
S: Transcervical intrauterine bupivacaine for the management of
postoperative pain following endometrial balloon ablation - a
pre-trial toxicity study. Gynecol Surg. 6:143–146. 2009. View Article : Google Scholar
|