Introduction
Although effective surgical and radiation treatment
exist for clinically localized esophageal cancer, refractory
metastatic esophageal cancer remains incurable. Distinct sets of
genes and proteins dictate the progression from precursor lesions
to localized disease and finally to metastatic disease (1). Identifying and characterizing key
genes that regulate the metastatic ability of esophageal cancer may
help identify which tumours are on an aggressive path from the
outset and may aid in treating them adequately before the
development of metastases. Through gene expression profiling
studies, metastasis-associated gene 2 (MTA2), a gene involved in
the transcriptional silencing machinery of mammalian cells, was
recently identified to be significantly overexpressed in metastatic
prostate cancer when compared to clinically localized disease
(2). MTA2 was identified by
differential cDNA library screening of metastatic breast cancer
cell lines and confirmed in breast cancer tissue (3). MTA2 overexpression at the
transcription level was observed in other cancers, such as
gastrointestinal cancers, and was associated with tumour
invasiveness and metastasis (4–6). In
addition, inhibition of MTA2 protein expression resulted in growth
inhibition of cancer cell lines (7). However, the expression of MTA2 in the
development and progression of esophageal carcinoma are not clear.
In the present study, we characterized for the first time the
expression of MTA2 in esophageal cancer progression. All
observations suggest that MTA2 is associated with carcinogenesis,
progression and metastasis in human tumours.
Based on the above considerations, we performed an
immunohistochemical study on MTA2 expression in esophageal squamous
cell carcinoma (ESCC) patients, and examined whether any
relationships exist among the expression of MTA2, pathological
tumour variables and prognosis in patients with ESCC.
Patients and methods
Patient selection
Surgical specimens were obtained from 162 patients
(112 males; 50 females) who had ESCC and underwent potentially
curative surgery at the Fourth Hospital of Hebei Medical University
(Shijiazhuang, China) between 1996 and 2002. The age of the
patients ranged from 30 to 89 years, with a mean of 61.9 years. The
tumour stage and disease grade were classified according to the 5th
edition of the TNM Classification of the International Union
Against Cancer (8). The evaluation
of tumour differentiation was based on histological criteria by the
Japanese Society for Esophageal Diseases (9). None of the patients had received
irradiation or chemotherapy prior to surgery. Patients who
underwent non-curative surgery and/or who had received inadequate
follow-up were excluded from this study (10). The information was entered into a
database following the approval of the Fourth Hospital of Hebei
Medical Univercity Institutional Review Board. M1 tumours were
attributable to distant lymph node metastases. Post-operative
chemotherapy and/or radiation therapy were not performed until
recurrence of the tumour was confirmed by a radiologic or
endoscopic examination. Specimens were fixed in 10% formaldehyde
solution and embedded in paraffin. We examined sections that
contained both a tumour portion and non-cancerous esophageal
epithelium.
Immunohistochemical staining and
evaluation
Immunohistochemical staining of the section for MTA2
was performed by streptoavidin-biotin methods. Antigen retrieval
was achieved by boiling the specimen in a citrate buffer 0.01 M (pH
7.0) at 120°C for 3 min, continued with a blocking treatment by
normal rabbit serum for 30 min. For MTA2, the specimens were
incubated with mouse anti-human monoclonal antibody (sc-55566;
Santa Cruz, CA, USA) at a dilution of 1:100 in phosphate-buffered
saline (PBS) at 4°C overnight. After washing with PBS, specimens
were incubated with a secondary antibody for 30 min.
Immunohistochemistry was performed using a Histofine SAB-PO (M) kit
(Zhongshan, Beijing, China). Human breast tumour expressing MTA2
was used as a positive control. Negative controls were prepared by
substituting normal mouse serum for primary antibody; no detectable
staining was evident.
The expression of MTA2 in tumour cells was compared
to MTA2 expression in non-cancerous epithelium. When the staining
in tumour cells (in the cancer cell nests) was stronger than the
staining noted in the non-cancerous epithelium, the sample was
classified as having MTA2 overexpression; when staining in the
tumour cell was as strong as the staining noted in the
non-cancerous epithelium it was considered to have weak expression,
or when there was no staining at all, the sample was classified as
exhibiting MTA2 under-expression. The sections were evaluated
independently by three investigators (Y.P. L., G.X. W. and X.L. W.)
without knowledge of the clinical and pathological background of
the patients. When the interpretation differed among observers,
re-evaluation was carried out for a final decision on a conference
microscope.
Statistical analysis
Statistical analysis was performed using the
unpaired two-group t-test for age. A Chi-square test was used for
gender, differentiation, TNM clinical classification, stage and
location. In this study, the correlation among MTA2, lymphatic
invasion, infiltrative growth pattern and blood-vessel invasion to
the tumour tissues was also assessed. The survival curves of the
patients were calculated using the Kaplan-Meier method, and
analysis was performed using the log-rank test. Differences were
considered statistically significant at P<0.05.
Results
Immunohistochemistry of MTA2
expression
Immunostaining of MTA2 in non-cancerous tissue was
detected in the nucleus of the parabasal layer (Fig. 1A). In tumour tissue, MTA2
expression was observed in the nucleus, particularly in cells
located in the central layer of the cancer cell nests (Fig. 1B). MTA2 overexpression was detected
in 65 of the 162 patients (40.1%). Ninety-seven cases (59.9%) were
classified as having MTA2 underexpression (Fig. 1C).
Relationship between MTA2 expression and
clinicopathological outcome
The relationship between MTA2 and
clinicopathological outcome in ESCC is summarized in Table I. There were significant
correlations between the overexpression of MTA2 and the TNM
clinical classification (depth of invasion, P=0.018; presence of
regional lymph node metastasis, P=0.009; presence of distant
metastasis, P=0.003; staging, P=0.006), differentiation (P=0.05),
lymphatic invasion (P=0.002) and blood-vessel invasion (P=0.004).
However, there was no correlation with patient age, gender and
location of the tumours.
 | Table I.Clinicopathological findings and MTA2
expression. |
Table I.
Clinicopathological findings and MTA2
expression.
| Parameters | Total (n=162) | MTA2 underexpression
(n=97) | MTA2 overexpression
(n=65) | P-value |
|---|
| Age (years; mean ±
SD) | 60.9±6.4 | 62.1±6.7 | 59.7±6.1 | 0.860 |
| Gender | | | | 0.320 |
| Male | 112 | 65 | 47 | |
| Female | 50 | 32 | 18 | |
| Differentiation | | | | 0.050 |
| Well | 26 | 19 | 7 | |
| Moderate | 86 | 51 | 35 | |
| Poor | 50 | 27 | 23 | |
| TNM | | | | |
| T | | | | 0.018 |
| T1 | 57 | 41 | 16 | |
| T2 | 31 | 17 | 14 | |
| T3 | 65 | 35 | 30 | |
| T4 | 9 | 4 | 5 | |
| N | | | | 0.009 |
| N0 | 73 | 53 | 20 | |
| N1 | 89 | 44 | 45 | |
| M | | | | 0.003 |
| M0 | 133 | 88 | 45 | |
| M1 | 29 | 9 | 20 | |
| Stage | | | | 0.006 |
| I | 48 | 35 | 13 | |
| II | 52 | 32 | 20 | |
| III | 36 | 23 | 13 | |
| IV | 26 | 7 | 19 | |
| Location | | | | 0.500 |
| Upper | 22 | 14 | 8 | |
| Middle | 100 | 60 | 40 | |
| Lower | 40 | 23 | 17 | |
| Lymphatic
invasion | | | | 0.002 |
| Negative | 52 | 41 | 11 | |
| Positive | 110 | 56 | 54 | |
| Blood vessel
invasion | | | | 0.004 |
| Negative | 78 | 57 | 21 | |
| Positive | 84 | 40 | 44 | |
Prognostic significance of MTA2
expression
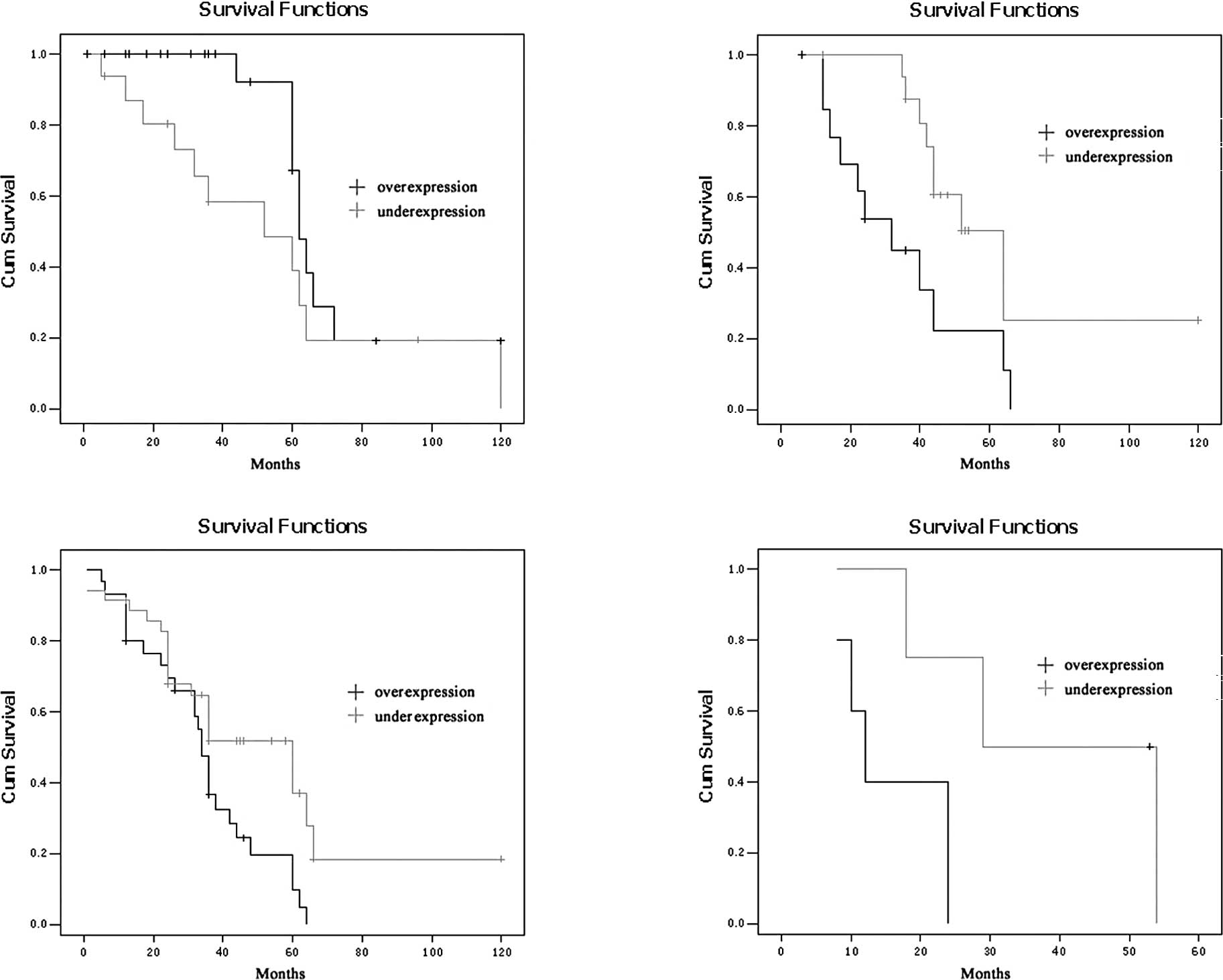
The 5-year survival rates of the ESCC patients with
MTA2 overexpression were significantly lower than those with MTA2
underexpression (P=0.002; Fig. 2).
The 5-year survival rates of the patients with overexpression and
underexpression of MTA2 were 18.4 and 46.0%, respectively. To
further investigate the influence of MTA2 expression within
homogeneous stage groups, adding more prognostic sense, we analysed
the seperate Kaplan-Meier diagrams for T1, T2, T3, T4 and N0/N1
tumours with MTA2 expression; it was also shown that the 5-year
survival rates of ESCC patients with MTA2 over-expression were
poorer in every group (P=0.036, 0.012, 0.014, 0.038 and 0.000,
0.002, respectively; Figs. 3 and
4).
Discussion
MTA2 expression and prognosis in cancer
in comparison with previous studies
In this study, we showed that MTA2 overexpression
frequently occurred in ESCC and was correlated with several aspects
of tumour progression summarized in the TNM classification.
Recently, the expression of MTA2 in various types of malignant
tumours has been reported. However, only a few reports, including
our previous article, showed the prognostic relevance of MTA2
expression in ESCC. Zhang et al (11) reported that MTA2 was expressed in
10% of epithelial cells with a weak immunoreactivity in the nuclear
compartment. A marked increase in the nuclear MTA signal was
observed in late stage carcinoma. In their study, MTA
immunoreactivity was associated with high tumour grade. We
previously showed the prognostic relevance of MTA2 expression in a
large series of gastric carcinoma and its significant relation to
clinicopathological findings. These results indicate that MTA2
overexpression may be an outcome of some important genetic and/or
epigenetic change in cancer progression; however, it remains
unknown whether in these carcinomas MTA2 expression merely
represents a surrogate marker for prognosis or whether it plays a
pathogenic role in carcinogenesis and tumour progression.
In non-cancerous epithelial esophageal squamous
cells, only slight MTA2 expression was observed in the parabasal
layers. MTA2 overexpression was detected in the nucelus of cancer
cells, especially in the central layers of the cancer cell nests.
These immunohistochemical results suggest that the overexpression
of MTA2 protein is correlated with TNM clinical classifications
(depth of invasion, presence of regional lymph node metastasis,
presence of distant metastasis and staging), lymphatic invasion and
blood-vessel invasion. There was a statistically significant
correlation between MTA2 over-expression and patient survival.
The prognosis of patients with overexpression of
MTA2 was poorer than that of patients with MTA2 underexpression.
Cancer invasion and metastasis are complex processes that include
alterations in cell adhesion, allowing transformed cells to invade
and migrate (12–14). MTA proteins are physiologically
expressed at only low levels in human tissue, except the testis
(10). Its expression has been
found to be associated with progression in solid cancers of various
organs and cancer cell lines with high invasive potential (15) and thus overexpression of MTA
protein has been reported to be correlated with tumour invasiveness
and lymph node metastasis in ESCC. Further study is required to
elucidate the relationship between MTA2 and prognosis in ESCC.
In this study, patients with MTA2 overexpression
were found to have a poorer prognosis for a 5-year survival.
However, by multivariate analysis, MTA2 overexpression did not
appear to be an independent prognostic factor. It may be influenced
by the depth of tumour invasion and distant metastasis. In
esophageal carcinoma, the presence of lymph node metastasis and the
number of lymph node metastases were associated with the worst
prognosis. As MTA2 overexpression was related to lymph node
metastases, patients with MTA2 overexpression had a poor
prognosis.
In conclusion, according to our data, MTA2 is
usually overexpressed in ESCC cells compared to non-cancerous
esophageal epithelia, and increased expression of MTA2 was
associated with a poor prognosis. Thus, our findings suggest that
MTA2 overexpression may play an important role in the progression
of ESCC. Tumour-specific MTA2 down-regulation may become a novel
therapeutic strategy for ESCC patients.
Acknowledgements
This study was supported by a grant
from the Health Department of Hebei Province (No. 07120), and a
grant from the Hebei Province Natural Science Foundation of P.R.
China (No. C2009001209).
References
|
1.
|
Shappell SB, Olson SJ, Hannah SE, et al:
Elevated expression of 12/15-lipoxygenase and cyclooxygenase-2 in a
transgenic mouse model of prostate carcinoma. Cancer Res.
63:2256–2267. 2003.PubMed/NCBI
|
|
2.
|
Toh Y, Kuninaka S, Endo K, et al:
Molecular analysis of a candidate metastasis-associated gene, MTA1:
possible interaction with histone deacetylase 1. J Exp Clin Cancer
Res. 19:105–111. 2000.PubMed/NCBI
|
|
3.
|
Cui Y, Niu A, Pestell R, et al:
Metastasis-associated protein 2 is a repressor of estrogen receptor
alpha whose overexpression leads to estrogen-independent growth of
human breast cancer cells. Mol Endocrinol. 20:2020–2035. 2006.
View Article : Google Scholar
|
|
4.
|
Nicolson GL, Nawa A, Toh Y, et al: Tumor
metastasis-associated human MTA1 gene and its MTA1 protein product:
role in epithelial cancer cell invasion, proliferation and nuclear
regulation. Clin Exp Metastasis. 20:19–24. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Saito M and Ishikawa F: The mCpG-binding
domain of human MBD3 does not bind to mCpG but interacts with
NuRD/Mi2 components HDAC1 and MTA2. J Biol Chem. 277:35434–35439.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Wong JJ, Hawkins NJ and Ward RL:
Colorectal cancer: a model for epigenetic tumorigenesis. Gut.
56:140–148. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Yao YL and Yang WM: The
metastasis-associated proteins 1 and 2 form distinct protein
complexes with histone deacetylase activity. J Biol Chem.
278:42560–42568. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Kumar R, Wang RA and Bagheri-Yarmand R:
Emerging roles of MTA family members in human cancers. Semin Oncol.
30:30–37. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Liu YP, Ma L, Wang SJ, et al: Prognostic
value of lymph node metastases and lymph node ratio in esophageal
squamous cell carcinoma. EJSO. 36:155–159. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Zhang H, Stephens C and Kumar R:
Metastasis tumor antigen family proteins during breast cancer
progression and metastasis in a reliable mouse model for human
breast cancer. Clin Cancer Res. 12:1479–1486. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Fujita N, Kajita M, Taysavang P, et al:
Hormonal regulation of metastasis-associated protein 3
transcription in breast cancer cells. Mol Endocrinol. 18:2937–2949.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Park SI, Zhang J, Phillips KA, et al:
Targeting SRC family kinases inhibits growth and lymph node
metastases of prostate cancer in an orthotopic nude mouse model.
Cancer Res. 68:3323–3333. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Manavathi B, Singh K and Kumar R: MTA
family of coregulators in nuclear receptor biology and pathology.
Nucl Recept Signal. 5:e0102007.PubMed/NCBI
|
|
14.
|
Li W, Zhang J, Liu X, Xu R and Zhang Y:
Correlation of appearance of metastasis-associated protein1 (Mta1)
with spermatogenesis in developing mouse testis. Cell Tissue Res.
329:351–362. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Adjei AA: Pemetrexed in the treatment of
selected solid tumors. Semin Oncol. 29:50–53. 2002. View Article : Google Scholar : PubMed/NCBI
|