Introduction
The objectives of the TNM system are to aid
clinicians and investigators in planning treatment, assessing
prognosis, stratifying patients for therapeutic studies, evaluating
the results of treatment and facilitating communication (1,2). A
series of modifications was introduced to the TNM staging system
for nasopharyngeal carcinoma (NPC), while focusing on the primary
tumor (T) and local node (N) components. However, the metastasis
(M1) stage is a ‘catch-all’ classification, covering a group of
patients whose outlook ranges from potentially curable to
incurable, and does not allow clinicians to stratify patients
according to prognosis or guide therapeutic decision making or
allow comparison of results of radical and non-radical
treatments.
In more recent years, increasing interest in the use
of local therapy for metastases has arisen to prolong the life and
improve the quality of life of patients with metastases including
NPC and other solid tumors (3–8).
Based on the fact that local therapy offers the chance of cure for
patients with liver metastases in colorectal cancer, the European
Colorectal Metastases Treatment Group in 2006 proposed a new M1
staging system that would subdivide the M1 into three subcategories
(9). This proposal was accepted in
seven editions of the AJCC cancer staging manual. The current
challenge is to obtain a similar result in modifying the M1 stage
of the TNM staging system for NPC. Studies have shown that liver
metastasis is prognostic for metastatic survival in metastatic NPC
and is associated with a shorter survival when compared with lung
or bone metastases (4–6,10–12).
However, there is a lack of large, systematic cohort studies on the
prognostic impact of metastatic status in NPC. We aimed to
subdivide the M1 stage according to our retrospective study of 1027
NPC patients with distant metastasis and a review of the
literature.
Patients and methods
Patients
This retrospective study was approved by the
Institutional Review Board of Sun Yat-Sen University Cancer Center.
The institutional database was reviewed to identify 1027 inpatients
with a confirmed clinical diagnosis of metastatic NPC between
January 1995 and December 2007. The diagnosis of metastasis was
based on histological evaluation, and/or combined with imaging and
subsequent clinical follow-up confirmation. We excluded the 11
patients who did not have a complete medical history of clinical
and follow-up data. We reviewed the clinical records of the
remaining 1016 cases. Patient demographics, characteristics of
their metastases and treatment modality were recorded using Epidate
3.0 software.
Study protocol
Subdivision of the M1 stage was attempted according
to various metastatic sites, the number of metastatic organs and
the number of metastases. The following prognostic variables were
also assessed: synchronous versus metachronous onset of metastases,
age (≤47 or >47 years), gender, AJCC 1998 stage classification
for T and N classification and body mass index (BMI) (<18.5,
18.5–24.9, >25). Patients were grouped according to the above
factors, and survival analysis was carried out by subgroup.
Metastatic survival was defined as survival from the first
diagnosis of metastases to the time of death, or the cut-off day of
the study using the Kaplan-Meier method. The survival status was
verified on 31 August, 2009 through direct telecommunication with
the patient or family and checking of the clinic attendance
records. The log-rank test was used to assess the significance
between variables. Analyses were performed using the SPSS 15.0
software package.
Results
Characteristics of metastases
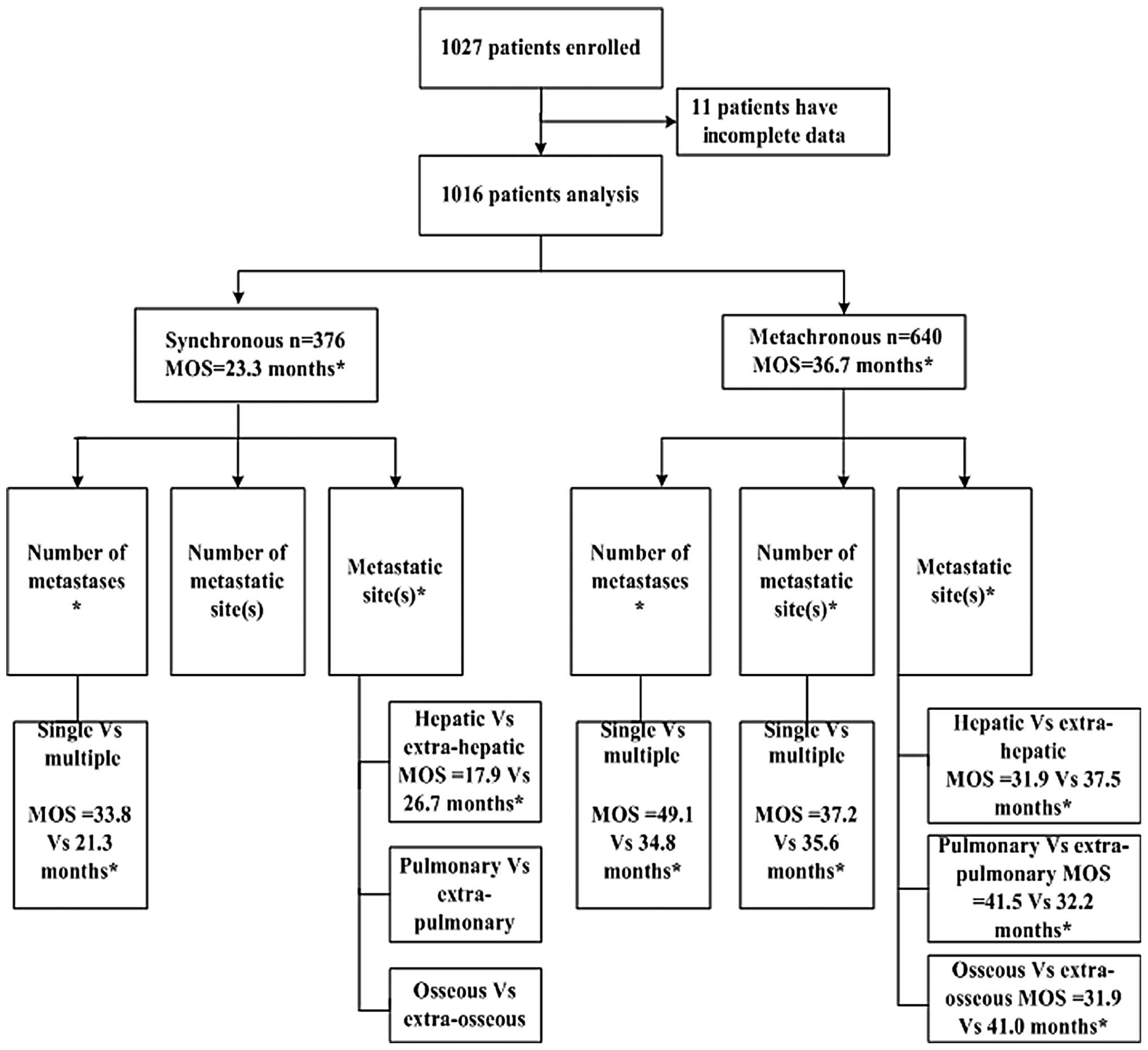
This analysis included 1016 patients. Patient ages
ranged from 15 to 78 years, with a median age of 45.8 years. At the
time of the first diagnosis of metastases, 376 patients had
solitary organ metastasis (33.96%) and 164 patients had solitary
metastatic lesions (16.15%). The most frequently involved sites
were bone (542, 53.35%), lung (420, 41.34%) and liver (302,
29.72%). Following diagnosis of metastases, all were candidates for
cytotoxic chemotherapy.
Metastatic overall survival and
prognostic factors
The median overall survival was 30.8 months from the
time of diagnosis of metastases for all of the 1016 NPC patients.
For the 376 patients in the synchronous metastatic group, the
median survival was 23.3 months and the 1-, 3- and 5-year
metastatic overall survival rates were 74.2, 27.6 and 18.5%,
respectively. For the 640 patients in the metachronous metastatic
group, the median survival was 36.7 months and the 1-, 3- and
5-year metastatic overall survival rates were 88.1, 49.6 and 28.6%,
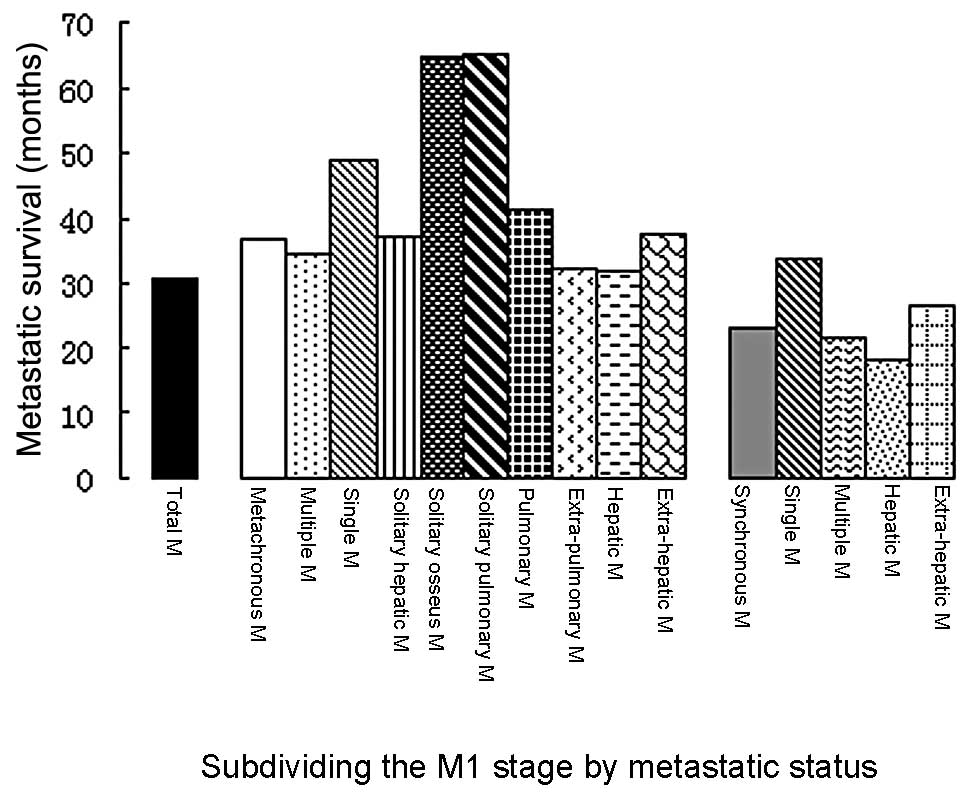
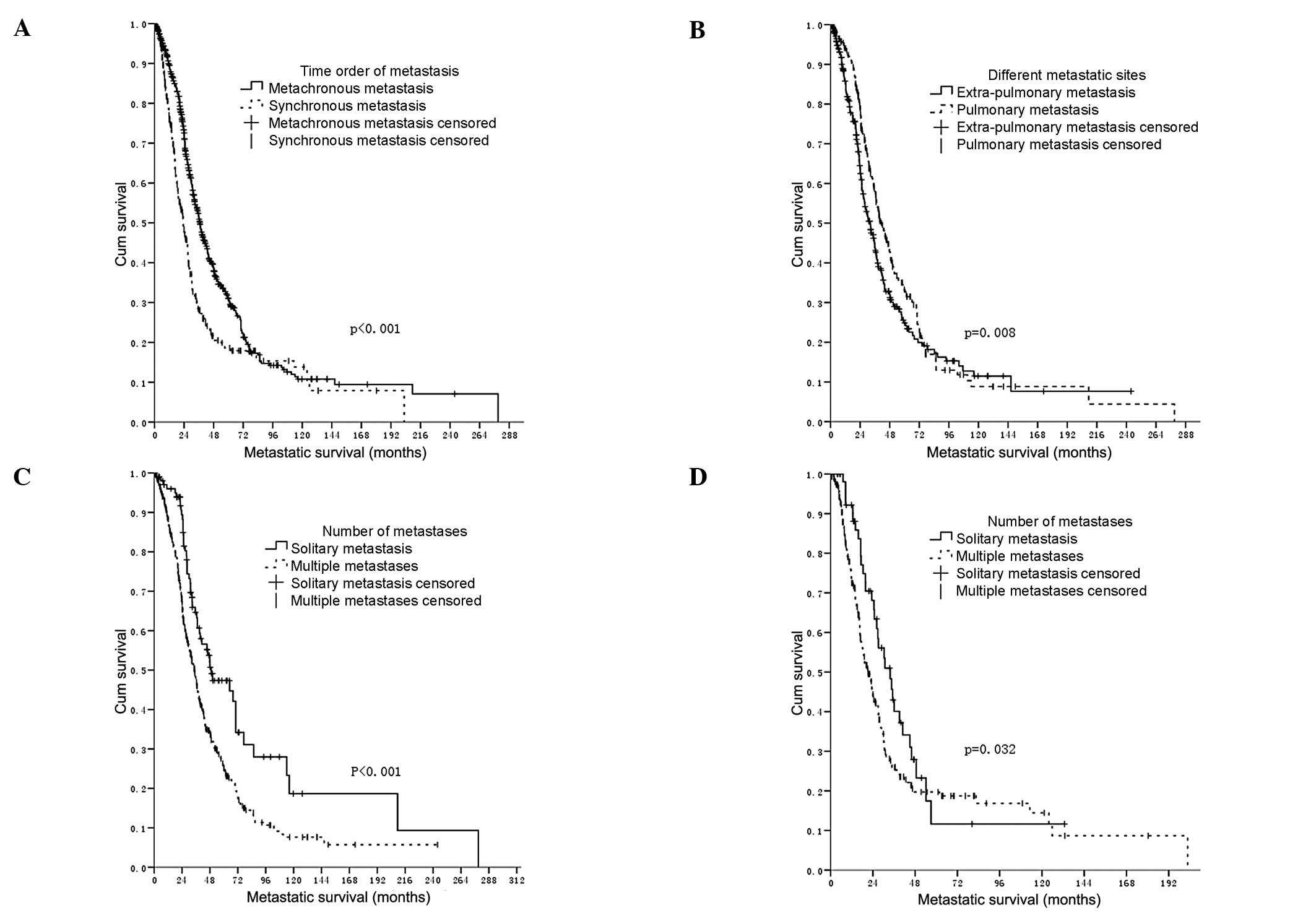
respectively (P<0.001). Subdivisions of the M1 stage according
to other metastatic statuses were significantly associated with
survival (Figs. 1 and 2).
In the univariate analysis among the metachronous
and synchronous metastatic groups, various metastatic sites (liver,
lung and bone) and the number of metastases (solitary) were
significant prognostic factors. The number of metastatic organs was
significantly associated with survival in the metachronous
metastatic group (Fig. 3), but not
in the synchronous metastatic group.
Upon multivariable analysis, in the metachronous
metastatic group, various metastatic sites (pulmonary), the number
of metastatic lesions (solitary) and N stage were identified as
independent prognostic factors, while metastatic status was not
associated with survival in the multivariate analysis (Table I).
 | Table I.Significantly independent variables
from the multivariate analysis of 1016 patients with metastatic
nasopharyngeal carcinoma. |
Table I.
Significantly independent variables
from the multivariate analysis of 1016 patients with metastatic
nasopharyngeal carcinoma.
| Factors | HR (95% CI) | P-value |
|---|
| Metachronous
metastatic group (n=640) | | |
| Number of
metastases (solitary) | 0.37 (0.21–0.52) | 0.003 |
| Metastatic sites
(pulmonary) | 0.62 (0.37–0.89) | 0.018 |
| N stage (1998)
(N3) | 1.24 (1.10–1.40) | 0.000 |
| Synchronous
metastatic group (n=376) | | |
| N stage (1998)
(N3) | 1.26 (1.08–1.49) | 0.004 |
| BMI (<18.5) | 1.30 (1.11–1.53) | 0.001 |
Discussion
A number of published studies (4–6,8,11,12),
as reported in Table II, have
focused on the characteristics of metastases, with the goal of
identifying a relatively favorable prognostic group. However, these
studies were limited by their small cohorts. The present study is
the first to reflect the clinical course of metastatic NPC in a
large cohort.
 | Table II.Survival of metastatic nasopharyngeal
carcinoma patients in studies focusing on different metastatic
status. |
Table II.
Survival of metastatic nasopharyngeal
carcinoma patients in studies focusing on different metastatic
status.
| First author
(ref.) | No. of patients | Survival |
|---|
| Pan et al
(4,6) | 376 | Median survival was
16.5 months for liver metastases |
| Pan et al
(5) | 480 | Median survival was
36.1 months for lung metastases |
| Ma et al
(8) | 105 | Median survival was
47.7 months for solitary lung metastases |
| Hui et al
(11) | 379 | Median survival after
primary radiotherapy was 2.1 vs 3.9 years for the distant
metastasis group vs. only lung metastasis group |
| Khanfir et al
(12) | 95 | One-year metastatic
survival rates were 40% (for all) and 51% vs. 25% for the single
metastasis group vs. the multiple metastasis group |
Given that patients with metastatic NPC may undergo
substantially different clinical courses, we sought to improve the
prediction of the prognosis of metastatic NPC by subdividing the M1
stage according to metastatic status, in order to categorize
patients with metastatic NPC into groups with large differences in
survival. Our results indicate that a subset of metastatic NPC
patients with pulmonary metastasis and/or solitary lesions was
potentially associated with a relatively favorable prognosis. In
addition, in the present study, the 16.15% incidence of solitary
lesions and the 41.34% incidence of pulmonary metastasis were high
rates and should not be ignored.
One of the aims of a new staging system would be to
allow the stratification of patients from the onset in terms of
their potential curability and use this to direct their therapeutic
management. In previously published results regarding hepatic and
pulmonary metastases from NPC, selected groups of patients
including patients with solitary metastasis benefit from local
therapy. Some are potentially curable (4–6,8).
From the experience of subdividing the M1 stage of colorectal
cancer, we hold that the development of such a staging system is of
importance. A challenge facing the TNM staging system for NPC is
how to modify the M1 stage for more precise prognostic prediction,
thereby enabling a more tailored therapeutic approach with improved
outcomes. The development of new staging strategies must be
relevant to current clinical practice, be evidence-based and
reflect the dominant prognostic factors consistently identified in
Cox multivariate regression analyses. Based on our results and
those published in the medical literature as reported in Table II, we propose that a status of
metachronous metastatic NPC is suggested for classifying patients
according to two categories. Patients with pulmonary metastasis
and/or solitary lesions are categorized as M1a; they have a better
prognosis compared with those patients with multiple metastases
located in any other anatomic site (designated as M1b). The
advantage of this suggested staging system is that it is simple and
can be used for the daily care of patients with metastatic NPC.
Although it is likely that a more detailed and perhaps more
sophisticated M1 staging system may be found to stratify patients
entered in clinical trials, these pilot results and modifications
may be currently useful in the design of clinical trials for
metastatic NPC, for it is able to more accurately stratify patients
into groups with fairly consistent outcome and thus help to
standardize the reported results of any therapeutic interventions,
with fewer samples and less financial expenditure.
Our results and modifications should be interpreted
in the light of some limitations, including the quality of
retrospective data from a single clinical center and the small
number of cases. Therefore, our results should be further validated
by additional studies to ensure its potential clinical value.
In conclusion, this study represents a single
institutional experience of distinguishing the prognostic
significance of different metastatic statuses of NPC and
subdividing the M1 stage of metastatic NPC. Our findings have the
potential to provide clinicians with useful, easily available
information for personalizing therapy.
References
|
1.
|
Greene FL and Sobin LH: The staging of
cancer: a retrospective and prospective appraisal. CA Cancer J
Clin. 58:180–190. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Gospodarowicz MK, Miller D, Groome PA,
Greene FL, Logan PA and Sobin LH: The process for continuous
improvement of the TNM classification. Cancer. 100:1–5. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Timmerman RD, Bizekis CS, Pass HI, et al:
Local surgical, ablative, and radiation treatment of metastases. CA
Cancer J Clin. 59:145–170. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Pan C, He N, Zhao M, et al: Subdividing
the M1 stage of liver metastasis for nasopharyngeal carcinoma to
better predict metastatic survival. Med Oncol. 28:1349–1355. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Pan CC, Wu PH, Yu JR, et al: Comparative
survival analysis in patients with pulmonary metastases from
nasopharyngeal carcinoma treated with radiofrequency ablation. Eur
J Radiol. 81:473–477. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Pan C, Wu P, Yu J, et al: CT-guided
radiofrequency ablation prolonged metastatic survival in patients
with liver metastases from nasopharyngeal carcinoma. Int J
Hyperthermia. 27:549–554. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Tomlinson JS, Jarnagin WR, DeMatteo RP, et
al: Actual 10-year survival after resection of colorectal liver
metastases defines cure. J Clin Oncol. 25:4575–4580.
2007.PubMed/NCBI
|
|
8.
|
Ma J WZ, Lin P, Wang X and Xie FY, Ma J,
Wen ZS, Lin P, Wang X and Xie FY: The results and prognosis of
different treatment modalities for solitary metastatic lung tumor
from nasopharyngeal carcinoma: a retrospective study of 105 cases.
Chin J Cancer. 29:787–795. 2010.PubMed/NCBI
|
|
9.
|
Nordlinger B, Van Cutsem E, Rougier P, et
al: Does chemotherapy prior to liver resection increase the
potential for cure in patients with metastatic colorectal cancer? A
report from the European Colorectal Metastases Treatment Group. Eur
J Cancer. 43:2037–2045. 2007. View Article : Google Scholar
|
|
10.
|
Ong YK, Heng DM, Chung B, et al: Design of
a prognostic index score for metastatic nasopharyngeal carcinoma.
Eur J Cancer. 39:1535–1541. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Hui EP, Leung SF, Au JSK, et al: Lung
metastasis alone in nasopharyngeal carcinoma: a relatively
favorable prognostic group - a study by the Hong Kong
nasopharyngeal carcinoma study group. Cancer. 101:300–306. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Khanfir A, Frikha M, Ghorbel A, Drira MM
and Daoud J: Prognostic factors in metastatic nasopharyngeal
carcinoma. Cancer Radiother. 11:461–464. 2007. View Article : Google Scholar
|