Introduction
Mucins are high-molecular-weight epithelial
glycoproteins that are heavily glycosylated with numerous
oligosaccharide side chains linked to a protein backbone called
apomucin. Mucin proteins are known for providing protection and
lubrication to epithelial surfaces; in addition, their roles in
cell signaling are under intense study (1–2).
Aberrant expression of mucins is likely associated with cancer
biology as alterations in the expression and/or glycosylation
patterns of various mucins influence cellular growth,
differentiation, transformation, adhesion, invasion and immune
surveillance. Mucins are divided into two distinct classes
according to their structure and function (3). Secreted-type mucins (MUC2, 5AC, 5B,
6, 7, 8, 9 and 19) are glycoproteins constituting the major
macromolecular component of mucus, and membrane-associated type
mucins (MUC1, 3A, 3B, 4, 12, 13, 15, 16, 17 and 20) contribute to
epithelial cell-cell interactions (3–4).
MUC1 is normally abundantly present at the luminal
surface of various secretory epithelial cells (5), and is associated with the epidermal
growth factor receptor tyrosine kinase and is involved in cellular
signaling (1,6). Overexpression of MUC1 is reported in
malignant neoplasms including breast, pancreatic, colorectal or
non-small-cell carcinoma of the lung, and is associated with a poor
prognosis (7–9).
MUC4 expression is also present in normal epithelial
tissues including stomach, colon, cervix and lung. The
overexpression of MUC4 has been discovered in a number of human
neoplasms (10–12). It has been shown that MUC4
expression is related to aggressive tumor behavior or a poor
outcome in intrahepatic cholangiocarcinoma, invasive ductal
carcinoma of the pancreas, extrahepatic bile duct carcinoma, and
lung adenocarcinoma (13–17). On the other hand, loss of MUC4
expression is related to poor survival in mucoepidermoid carcinoma
of the salivary gland, squamous cell carcinoma of the upper
aerodigestive system, and adenocarcinoma of lung (18–21).
The function of MUC4 in gastric cancer is not understood. To date,
there have been few studies on the relationship between MUC4
expression and patient prognosis in gastric adenocarcinoma.
The aims of this study were to investigate MUC1 and
4 expression patterns and to evaluate the correlation of MUC1 and 4
expression with patient prognosis in gastric adenocarcinoma.
Materials and methods
Patients
We recruited 365 patients who underwent gastrectomy
for gastric adenocarcinoma from archives of paraffin blocks at
Keimyung University Dongsan Hospital from October 1995 to December
1999. Tissue samples were fixed in formalin and embedded in
paraffin. All cases were reviewed by an expert panel of two
pathologists according to the current criteria of the WHO
classification for morphological features and immunohistochemical
results. The clinical data (age, gender, T stage, N stage, Lauren
classification, date of diagnosis, adjuvant chemotherapy, date of
relapse, and date of last follow-up) and pathological reports of
the patients with gastric adenocarcinoma were collected from the
medical records. Patients were divided into subgroups: ≤60 and
>60 years of age.
Immunohistochemistry
Formalin-fixed, paraffin-embedded tissue samples
were used for tissue microarray (TMA). Representative areas of each
tumor were marked on each H&E-stained slide, and the
corresponding areas of tissue blocks were sampled. The designated
areas of each donor block were collected using a tissue cylinder
punch of 5-mm diameter, and samples were transferred to a recipient
block.
Sections (4 μm) from TMAs were cut from 10% (v/v)
formalin buffer and embedded in paraffin, were mounted on
Superfrost Plus glass slides (VWR Scientific, West Chester, PA,
USA) and incubated at 60°C for 15 min. The slides were next
deparaffinized in xylene, rehydrated in graded alcohol solutions,
and washed in tap water. Endogenous peroxidase activity was blocked
by the addition of 3% (v/v) H2O2. Slides were
placed in a steam cooker filled with 10 mM sodium citrate buffer,
pH 6.0, for antigen retrieval. After treatment with a blocking
agent (Dako, Carpinteria, CA, USA) for 10 min to block nonspecific
protein binding, samples were incubated for a further 1 h with
primary anti-human mouse antibodies which included MUC1 (1:200,
Zymed, South San Francisco, CA, USA) and MUC4 (1:300, Zymed). After
reaction with a biotinylated antibody for 30 min, antigen-antibody
complexes were visualized using a streptavidin-horseradish
peroxidase conjugate (Dako LSAB kit; Dako, Los Angeles, CA, USA)
employing diaminobenzidine as the chromogen. Slides were
counterstained with Meyer's hematoxylin for 3–5 min.
Immunopositivity for MUC1 and MUC4 was evaluated by
staining intensity (0, negative; 1, weak; 2, moderate; 3, strong)
and the proportions of positive staining cells (0, 0% positive; 1,
≤10% positive; 2, >10% and ≤50% positive; 3, >50% positive).
Samples were considered positive for MUC1 or 4 when staining
intensity was >0 (weak-to-strong) and >10% of cells were
positively stained.
Statistics
The SPSS statistical package, version 19.0 for
Windows, was used for all statistical analyses. The relationship
between MUC1/4 immunoreactivity and each clinicopathological
variable was evaluated using the Chi-square or Fisher's exact test,
as appropriate. Disease-free survival was measured from the date of
diagnosis to the date of recurrence or the last follow-up. Overall
survival was measured from the date of diagnosis to the date of
death or the last follow-up visit. Disease-free and overall
survival were measured according to the Kaplan-Meier method and the
Cox regression test, and survival rates were compared using the
log-rank test. P-values <0.05 were considered to indicate
statistically significant results, and all p-values correspond to
two-sided significance tests.
Results
Clinicopathological variables
The mean age of the 365 patients with gastric
adenocarcinoma was 56.2 years (range, 25–82 years). There were 248
(67.9%) male patients and 117 (32.1%) female patients. Early
gastric carcinoma, invading the mucosal or submucosal layer, was
observed in 126 (34.5%) patients and advanced gastric carcinoma,
which invaded the proper muscle or a deeper layer, was observed in
239 (65.5%). According to the Lauren classification, 112 (30.7%)
patients had diffuse type, 251 (68.8%) had intestinal type and two
(0.5%) had mixed type. The clinicopathological variables of gastric
adenocarcinoma are summarized in Table
I.
 | Table I.Clinicopathological variables of the
gastric adenocarcinoma cases. |
Table I.
Clinicopathological variables of the
gastric adenocarcinoma cases.
| Clinical
variables | Value |
|---|
| Mean age, years
(range) | 56.2 (25–82) |
| Gender (M/F) | 248:117 |
| Depth of tumor
invasion, n (%) | |
| Mucosa or submucosa
(early gastric cancer) | 126 (34.5) |
| Other than
submucosa (advanced gastric cancer) | 239 (65.5) |
| Lymph node (regional)
metastasis, n (%) | |
| No | 182 (49.9) |
| Yes | 182 (50.1) |
| Lauren
classification, n (%) | |
| Diffuse-type | 112 (30.7) |
|
Intestinal-type | 251 (68.8) |
| Mixed-type | 2 (0.5) |
| Recurrence, n
(%) | 89 (24.4) |
| Survival, n (%) | 72 (19.7) |
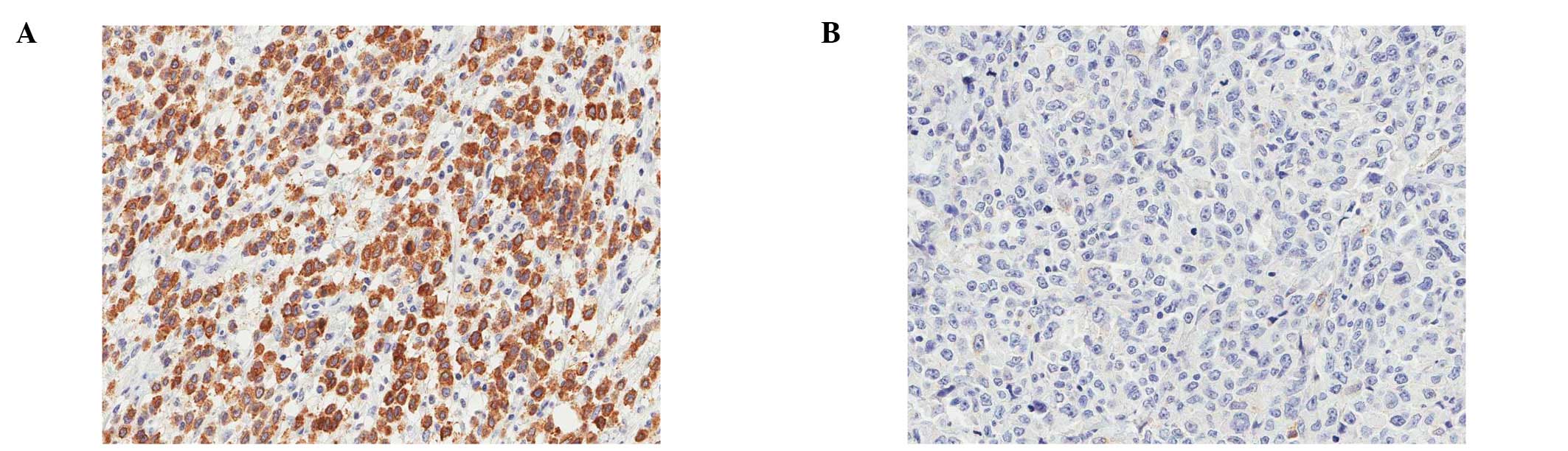
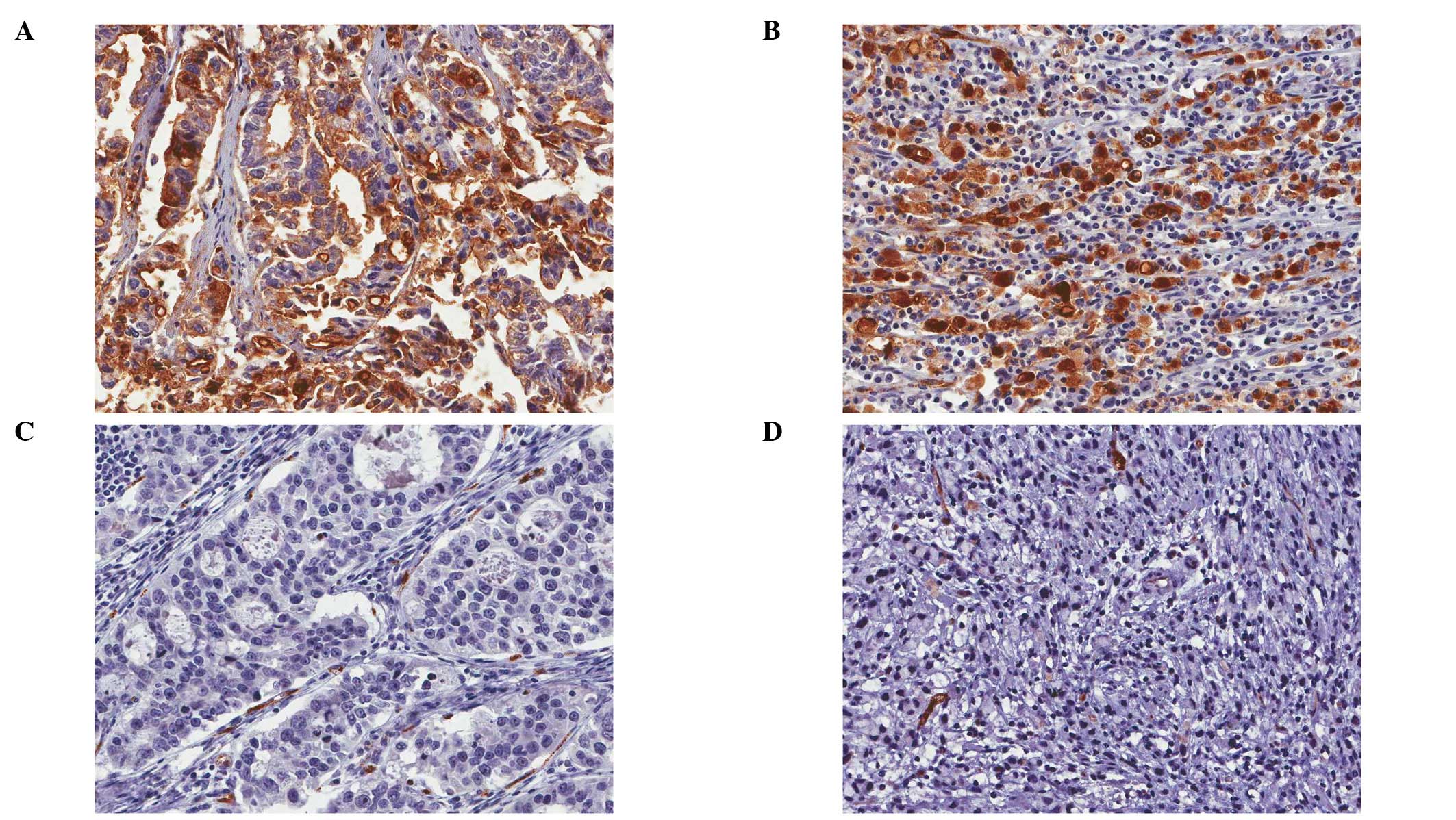
MUC1 and MUC4 expression
MUC1 demonstrated diffuse and strong
immunopositivity on the membrane and in the cytoplasm of normal
gastric glandular cells. MUC4 was also strongly positive on the
membrane and in the cytoplasm of normal surface glandular cells,
but was negative on the membrane or in the cytoplasm of pyloric
glandular cells.
Two hundred and ninety-two out of 315 (92.7%) cases
were positive for MUC1 immunoreactivity and 216 out of 317 (60.5%)
were positive for MUC4 immunoreactivity. Staining patterns of MUC1
and MUC4 in tumor cells were the same as that of MUC1 and MUC4 in
normal glandular cells (Fig. 1 and
2). MUC1 expression was not
correlated with any other clinicopathological variables such as
age, gender, depth of invasion, lymph node metastasis, Lauren
classification or recurrence. However, MUC4 expression was
significantly correlated with recurrence (P=0.033), but not with
any other variables such as age, gender, depth of invasion, lymph
node metastasis or Lauren classification (Table II). The prevalence of MUC4
expression was higher in the intestinal-type (42.4%) than in the
diffuse-type (32.7%) but this did not achieve statistical
significance (P=0.100). MUC4-positive tumor cells were not
morphologically different than the MUC4-negative tumor cells in
either the diffuse- or intestinal-type. (Fig. 2)
 | Table II.Correlations between MUC1/4 expression
and clinical variables of the gastric adenocarcinoma cases. |
Table II.
Correlations between MUC1/4 expression
and clinical variables of the gastric adenocarcinoma cases.
| MUC1
expressiona
| | MUC4
expressiona
| |
|---|
| Positive No. | Negative No. | P-value | Positive No. | Negative No. | P-value |
|---|
| Age (years) | | | | | | |
| ≤60 | 14/315 | 165/315 | 0.828 | 80/357 | 130/357 | 0.582 |
| >60 | 9/315 | 127/315 | | 61/357 | 86/357 | |
| Gender | | | | | | |
| Male | 14/315 | 199/315 | 0.492 | 98/357 | 144/357 | 0.643 |
| Female | 9/315 | 93/315 | | 43/357 | 72/357 | |
| Depth of
invasion | | | | | | |
| Early gastric
cancer | 4/315 | 93/315 | 0.168 | 40/357 | 80/357 | 0.109 |
| Advanced gastric
cancer | 19/315 | 199/315 | | 101/357 | 136/357 | |
| Lymph node
metastasis | | | | | | |
| No | 10/315 | 138/315 | 0.830 | 62/357 | 113/357 | 0.131 |
| Yes | 13/315 | 154/315 | | 79/357 | 103/357 | |
| Lauren
classification | | | | | | |
| Diffuse-type | 6/314 | 93/314 | 0.647 | 36/355 | 74/355 | 0.100 |
|
Intestinal-type | 17/314 | 198/314 | | 104/355 | 141/355 | |
| Recurrence | | | | | | |
| No | 17/314 | 215/314 | 1.000 | 96/356 | 171/356 | 0.033 |
| Yes | 6/314 | 76/314 | | 44/356 | /356 | |
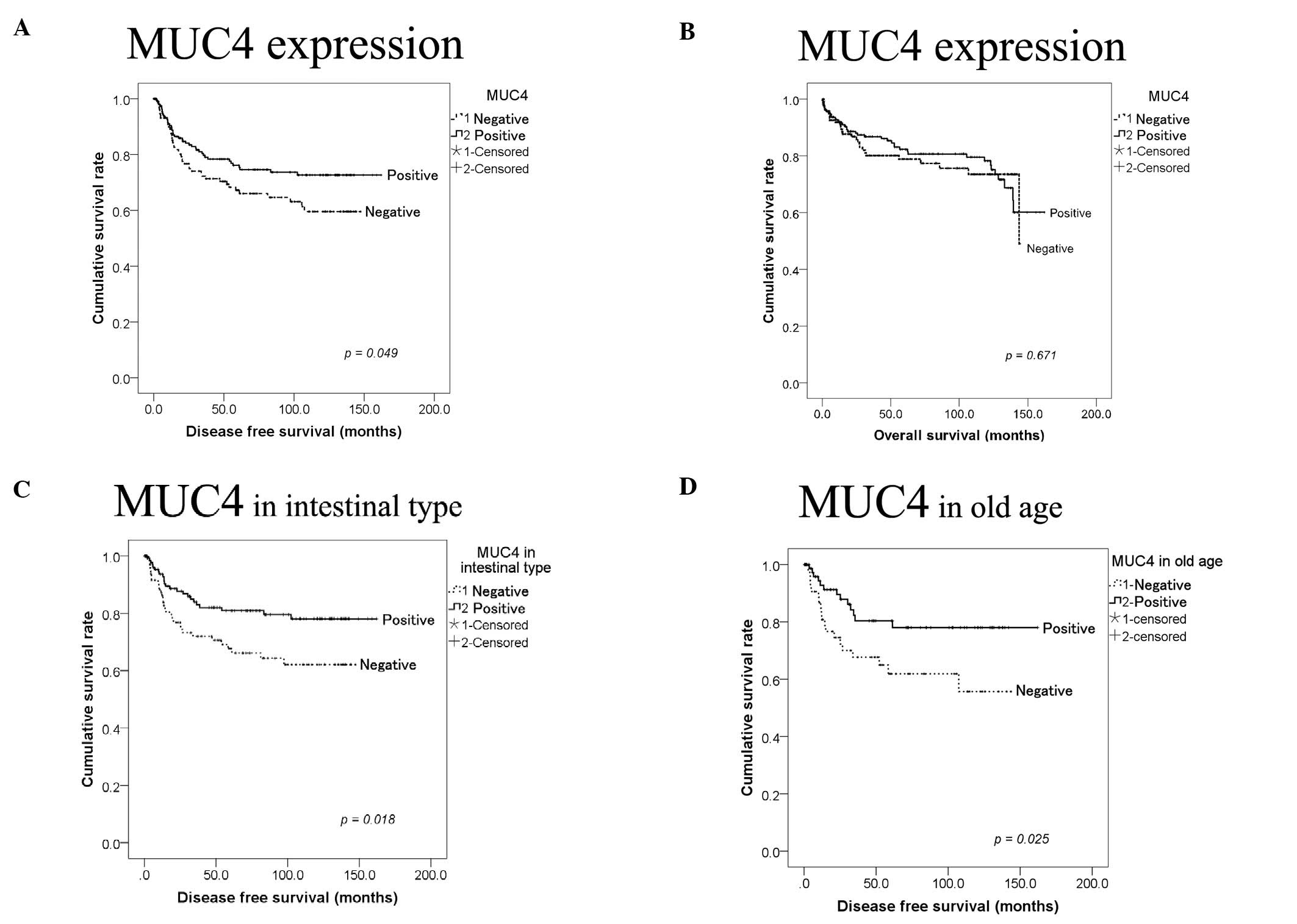
Prognosis
Loss of MUC4 expression was significantly correlated
with worse disease-free survival (p=0.049) but was not
significantly correlated with overall survival (p= 0.671) in
Kaplan-Meier survival test. (Fig.
3) Tumor invasion (more than submucosa), presence of lymph node
metastasis, and diffuse type by Lauren classification were
significantly correlated with worse disease-free survival
(p<0.001, <0.001 and =0.044) in Kaplan-Meier survival
analysis. However, MUC1 expression and other clinical variables
including age, gender, or adjuvant chemotherapy were not correlated
with disease-free survival.
In intestinal-type gastric cancer according to
Lauren classification, loss of MUC4 expression was significantly
correlated with worse disease-free survival (p= 0.018), but was not
significantly correlated with disease-free survival in the
diffuse-type although loss of MUC4 was significantly correlated
with disease-free survival in overall types of gastric carcinoma.
Loss of MUC4 expression was also significantly correlated with
worse disease-free survival (p=0.025) in the older age group
(>60), but was not correlated with worse disease-free survival
in the younger age group (≤60). Gender, depth of tumor invasion,
lymph node metastasis, or adjuvant chemotherapy did not have an
effect on MUC4 expression and disease-free survival.
Discussion
Significant correlations between MUC1 expression and
clinico pathological manifestations including Lauren type or
recurrence were not identified in the present study. In several
studies, MUC1 expression has been suggested as a prognostic factor
of gastric adenocarcinoma (1,22–24).
The proportion of MUC1 overexpression in the present study was more
than 90%. However, MUC1 expression was detected in 30–60% of
gastric adenocarcinoma cases in other studies. The difference in
MUC1 expression could be explained by different conditions
including the type of commercial antibody, concentration of the
primary antibody or substrate of staining. Therefore, for higher
accuracy, further studies should be undertaken with a larger number
of gastric adenocarcinoma samples using standardized methods.
Similarly, comparing the expression patterns of other molecules
such as E-cadherin or other mucins may potentiate the possible use
of MUC1 as a prognostic marker for gastric adenocarcinomas.
However, we demonstrated that MUC1 expression may be valuable in
the diagnosis of gastric adenocarcinoma particularly in difficult
clinical cases including metastatic carcinoma of unknown primary
site.
Aberrant expression of MUC4 has been reported in
various cancers and inflammatory diseases. MUC4 is upregulated in
high-grade dysplasia and adenocarcinoma of the esophagus.
High-grade salivary tumors have a trend for reduced MUC4 expression
compared to low-grade and intermediate-grade tumors.
MUC4-expressing salivary gland mucoepidermoid tumors are associated
with improved patient survival and a longer time to recurrence as
compared with patients whose tumors were diagnosed as being
negative for MUC4 expression. In addition, prostate cancer has
exhibited downregulation of MUC4 expression in prostate carcinomas
as compared with that in the normal/benign prostate regions. In
contrast to the aforementioned studies, high MUC4 expression
correlates with a short disease-free interval and a poor survival
rate of small-sized lung adenocarcinomas, cholangiocarcinomas,
epithelial ovarian carcinomas, pancreatic cancers and colorectal
adenocarcinoma (12–16,25,26).
MUC4 overexpression in gastric cancer tissues compared with normal
adjacent tissues has been previously reported (27). MUC4 is known to be expressed in
embryonic gastric tissues at approximately 8 weeks gestation. It
has also been shown that a number of embryogenesis phenomena such
as cell proliferation, lineage allocation, cell migration, and
differentiation of cells are also observed during cancer
progression (28). Overexpression
of MUC4 has a role in promoting properties in poorly differentiated
gastric non-signet ring cell carcinoma cells (29). Our study into the role of MUC4 as a
prognostic marker in gastric adenocarcinoma tissues found
contradictory results. The level of MUC4 expression was higher in
the intestinal-type than the diffuse-type but did not achieve
statistical significance. Therefore, further research is required
to evaluate the functional diversity of MUC4. MUC4 is an
intramembrane ligand for receptor tyrosine kinase ErbB2, which is a
transmembrane glycoprotein encoded by the c-Erb-B2
proto-oncogene with a tyrosine kinase domain (13,30–32).
MUC4 expression may be a more important marker in tumor
differentiation than the cell signaling pathway or as an
epithelial-mesenchymal transition relating factor. Likewise in
gastric adenocarcinoma, MUC4 expression may be a more important
tumor differentiation marker and loss of MUC4 expression may denote
poor differentiation regardless of morphological change.
Additionally, there are studies demonstrating that MUC4 expression
was correlated with increased apoptosis. MUC4 was found to
upregulate the expression of the cell cycle inhibitor
p27kip. Hence, the role of MUC4 in apoptotic cell death
is seemingly regulated by Erb-B2 and other signaling
components that are altered in the cancer cell (33).
Our study focused on investigating the prognostic
significance of MUC1 and MUC4 expression in gastric cancer. We
identified that loss of MUC4 expression was significantly
correlated with worse disease-free survival. MUC4 may serve diverse
functions in a context-dependent manner. There is a need to further
our comprehension of the function and mechanism of MUC4 in normal
and pathological conditions of gastric epithelial cells. Therefore,
delineating the signaling mechanisms in the expression of MUC4 and
defining the specific functions of MUC4 may lead to a better
understanding of gastric adenocarcinoma.
References
|
1.
|
Li XH, Zheng HC, Wang ZG, et al: The
clinicopathological and prognostic significance of MUC-1 expression
in Japanese gastric carcinomas: an immunohistochemical study of
tissue micro-arrays. Anticancer Res. 28:1061–1067. 2008.PubMed/NCBI
|
|
2.
|
Hollingsworth MA and Swanson BJ: Mucins in
cancer: protection and control of the cell surface. Nat Rev Cancer.
4:45–60. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Zheng H, Takahashi H, Nakajima T, et al:
MUC6 down-regulation correlates with gastric carcinoma progression
and a poor prognosis: an immunohistochemical study with tissue
micro-arrays. J Cancer Res Clin Oncol. 132:817–823. 2006.
View Article : Google Scholar
|
|
4.
|
Cozzi PJ, Wang J, Delprado W, et al: MUC1,
MUC2, MUC4, MUC5AC and MUC6 expression in the progression of
prostate cancer. Clin Exp Metastasis. 22:565–573. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Fattorossi A, Battaglia A, Malinconico P,
et al: Constitutive and inducible expression of the epithelial
antigen MUC1 (CD227) in human T cells. Exp Cell Res. 280:107–118.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Pandey P, Kharbanda S and Kufe D:
Association of the DF3/MUC1 breast cancer antigen with Grb2 and the
Sos/Ras exchange protein. Cancer Res. 55:4000–4003. 1995.PubMed/NCBI
|
|
7.
|
Monges GM, Mathoulin-Portier MP, Acres RB,
et al: Differential MUC 1 expression in normal and neoplastic human
pancreatic tissue. An immunohistochemical study of 60 samples. Am J
Clin Pathol. 112:635–640. 1999.PubMed/NCBI
|
|
8.
|
Nakamori S, Ota DM, Cleary KR, Shirotani K
and Irimura T: MUC1 mucin expression as a marker of progression and
metastasis of human colorectal carcinoma. Gastroenterology.
106:353–361. 1994.PubMed/NCBI
|
|
9.
|
Khodarev NN, Pitroda SP, Beckett MA, et
al: MUC1-induced transcriptional programs associated with
tumorigenesis predict outcome in breast and lung cancer. Cancer
Res. 69:2833–2837. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Moniaux N, Escande F, Porchet N, Aubert JP
and Batra SK: Structural organization and classification of the
human mucin genes. Front Biosci. 6:D1192–D1206. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Ho SB, Niehans GA, Lyftogt C, et al:
Heterogeneity of mucin gene expression in normal and neoplastic
tissues. Cancer Res. 53:641–651. 1993.PubMed/NCBI
|
|
12.
|
Jeon JM, Lee HW, Park JY, et al:
Expression of MUC1 and MUC4 and its prognostic significance in
non-small cell lung carcinoma. Korean J Pathol. 44:397–403. 2010.
View Article : Google Scholar
|
|
13.
|
Shibahara H, Tamada S, Higashi M, et al:
MUC4 is a novel prognostic factor of intrahepatic
cholangiocarcinoma-mass forming type. Hepatology. 39:220–229. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Tamada S, Shibahara H, Higashi M, et al:
MUC4 is a novel prognostic factor of extrahepatic bile duct
carcinoma. Clin Cancer Res. 12:4257–4264. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Saitou M, Goto M, Horinouchi M, et al:
MUC4 expression is a novel prognostic factor in patients with
invasive ductal carcinoma of the pancreas. J Clin Pathol.
58:845–852. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Tsutsumida H, Goto M, Kitajima S, et al:
MUC4 expression correlates with poor prognosis in small-sized lung
adenocarcinoma. Lung Cancer. 55:195–203. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Singh AP, Chauhan SC, Bafna S, et al:
Aberrant expression of transmembrane mucins, MUC1 and MUC4, in
human prostate carcinomas. Prostate. 66:421–429. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Kwon KY, Ro JY, Singhal N, et al: MUC4
expression in non-small cell lung carcinomas: relationship to tumor
histology and patient survival. Arch Pathol Lab Med. 131:593–598.
2007.PubMed/NCBI
|
|
19.
|
Weed DT, Gomez-Fernandez C, Pacheco J, et
al: MUC4 and ERBB2 expression in major and minor salivary gland
mucoepidermoid carcinoma. Head Neck. 26:353–364. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Alos L, Lujan B, Castillo M, et al:
Expression of membrane-bound mucins (MUC1 and MUC4) and secreted
mucins (MUC2, MUC5AC, MUC5B, MUC6 and MUC7) in mucoepidermoid
carcinomas of salivary glands. Am J Surg Pathol. 29:806–813. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Weed DT, Gomez-Fernandez C, Yasin M, et
al: MUC4 and ErbB2 expression in squamous cell carcinoma of the
upper aerodigestive tract: correlation with clinical outcomes.
Laryngoscope. 114:1–32. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Yonezawa S, Goto M, Yamada N, Higashi M
and Nomoto M: Expression profiles of MUC1, MUC2, and MUC4 mucins in
human neoplasms and their relationship with biological behavior.
Proteomics. 8:3329–3341. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Akyurek N, Akyol G, Dursun A, Yamac D and
Gunel N: Expression of MUC1 and MUC2 mucins in gastric carcinomas:
their relationship with clinicopathologic parameters and prognosis.
Pathol Res Pract. 198:665–674. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Utsunomiya T, Yonezawa S, Sakamoto H, et
al: Expression of MUC1 and MUC2 mucins in gastric carcinomas: its
relationship with the prognosis of the patients. Clin Cancer Res.
4:2605–2614. 1998.PubMed/NCBI
|
|
25.
|
Westgaard A, Schjolberg AR, Cvancarova M,
Eide TJ, Clausen OP and Gladhaug IP: Differentiation markers in
pancreatic head adenocarcinomas: MUC1 and MUC4 expression indicates
poor prognosis in pancreatobiliary differentiated tumours.
Histopathology. 54:337–347. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Shanmugam C, Jhala NC, Katkoori VR, et al:
Prognostic value of mucin 4 expression in colorectal
adenocarcinomas. Cancer. 116:3577–3586. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27.
|
Lopez-Ferrer A, de Bolos C, Barranco C, et
al: Role of fucosyltransferases in the association between apomucin
and Lewis antigen expression in normal and malignant gastric
epithelium. Gut. 47:349–356. 2000. View Article : Google Scholar
|
|
28.
|
Buisine MP, Devisme L, Maunoury V, et al:
Developmental mucin gene expression in the gastroduodenal tract and
accessory digestive glands. I. Stomach. A relationship to gastric
carcinoma. J Histochem Cytochem. 48:1657–1666. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
29.
|
Senapati S, Chaturvedi P, Sharma P, et al:
Deregulation of MUC4 in gastric adenocarcinoma: potential
pathobiological implication in poorly differentiated non-signet
ring cell type gastric cancer. Br J Cancer. 99:949–956. 2008.
View Article : Google Scholar
|
|
30.
|
Moniaux N, Nollet S, Porchet N, Degand P,
Laine A and Aubert JP: Complete sequence of the human mucin MUC4: a
putative cell membrane-associated mucin. Biochem J. 338:325–333.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
31.
|
Carraway KL III, Rossi EA, Komatsu M, et
al: An intramembrane modulator of the ErbB2 receptor tyrosine
kinase that potentiates neuregulin signaling. J Biol Chem.
274:5263–5266. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
32.
|
Carraway KL, Ramsauer VP, Haq B and
Carothers Carraway CA: Cell signaling through membrane mucins.
Bioessays. 25:66–71. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
33.
|
Jepson S, Komatsu M, Haq B, et al:
Muc4/sialomucin complex, the intramembrane ErbB2 ligand, induces
specific phosphorylation of ErbB2 and enhances expression of
p27(kip), but does not activate mitogen-activated kinase or protein
kinaseB/Akt pathways. Oncogene. 21:7524–7532. 2002. View Article : Google Scholar
|