Introduction
A discoid meniscus is an anatomical congenital
anomaly which was considered to be a vestige of viviparous
cartilage development of the knee (1,2).
Diagnosis of the discoid meniscus has been improved by the MRI
technique, and the incidence of discoid lateral meniscus of the
knee in the Chinese population is 16–46% (3). Although it may be left untreated,
tearing of the discoid lateral meniscus may cause pain and
immobility of the knee joint, and therefore requires surgery. The
traditional treatment is to open the capsule and resect the
meniscus, but this often leads to the development of arthritis
(4). Since the use of arthroscopy
has been suggested to preserve part of the meniscus (5,6), we
investigated the short-term clinical outcomes of 43 cases of
arthoscopic meniscectomy for discoid lateral meniscus tears.
Patients and methods
Patients
The study was conducted in the Renmin Hospital,
Hubei University of Medicine, China from February, 2007 to
December, 2010. Forty-two patients (47 knees) with injured discoid
lateral meniscus were treated using arthroscopy, including 10 men
and 32 women, aged from 14 to 62 years (mean, 31.46). The type of
discoid lateral meniscus in these cases was evaluated by the
O’Connor classification (7)
(Table I) and there was no
Wrisberg-type by Watanabe classification (8). This study was approved by the ethics
committee of Hubei University of Medicine Hubei, China) and written
informed consent was obtained from all subjects.
 | Table ITear patterns according to types of
discoid lateral meniscus. |
Table I
Tear patterns according to types of
discoid lateral meniscus.
| Type of discoid
lateral meniscus
|
|---|
| Tear pattern | Complete | Incomplete | Total |
|---|
| Simple
horizontal | 7 | 0 | 7 |
| Complicated
horizontal | 8 | 4 | 12 |
| Longitudinal | 7 | 6 | 13 |
| Radial | 0 | 8 | 8 |
| Degenerative | 0 | 4 | 4 |
| Complex | 0 | 3 | 3 |
| Total | 22 | 25 | 47 |
The preoperative examinations included physical
examination, X-ray imaging and MRI of the injured knee. Physical
examination revealed atrophy of the quadriceps femoris muscle,
lateral tibiofemoral joint line tenderness, restriction of mobility
and positive McMurray sign. Certain patients had ‘clicking’ of
joints. Radiography revealed a widened lateral joint space
(Fig. 1) in 13 knees. The MRI
results were all in accordance with those of the arthroscopic
examination (Fig. 2).
Surgical techniques
Patients were arthroscoped (Stryker, Kalamazoo, MI,
USA) in the supine position under continuous peridural anesthesia
or combined spinal epidural anesthesia with a calibrated pneumatic
tourniquet (the tourniquet time was <90 min). Arthroscopic
examination was performed to observe the intra-articular structures
in the following order: suprapatellar pouch, patellofemoral joint,
medial gutter, medial compartment, intercondylar notch, lateral
compartment and lateral gutter. The meniscus was probed carefully
to identify individual structures, type of the discoid lateral
meniscus, stability of the peripheral rim, position and extent of
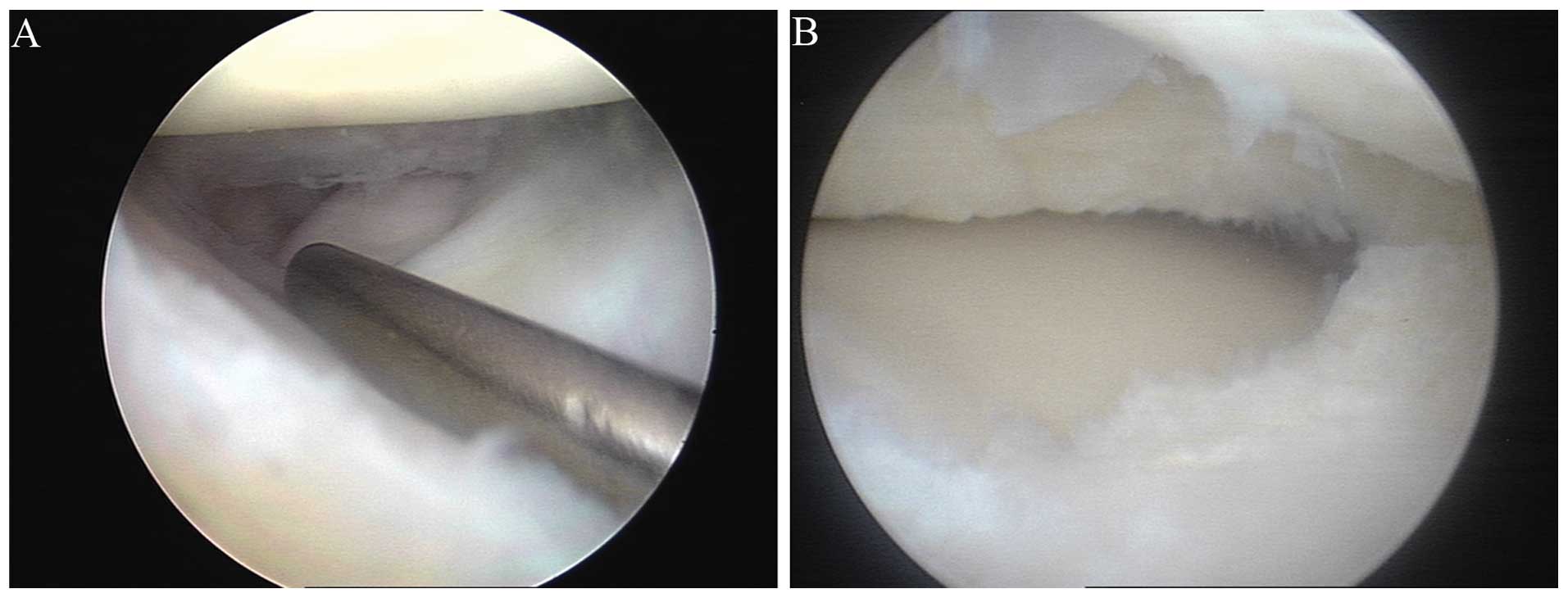
the meniscus tear, as well as other accompanying lesions (Figs. 3A and 4A).
The meniscal tear was carefully resected using
standard techniques and the meniscal rim was preserved. The methods
in common use are partial resection (shaping of the discoid
meniscus), hypo-complete resection and complete resection. For
partial meniscectomy, the small inferior leaf of the horizontal
cleavage tear was partially resected, whereas the main body was
preserved 6–8 mm in width during surgery (9) and the anatomical shape was maintained
with arthroscopy. Following the meniscectomy, the resected edge was
smoothened, the meniscus was reshaped (from discoid to crescent),
the peripheral rim was then thickened and the free edge of the
meniscus was thinned to form a slope (Figs. 3B and 4B). Following surgery, the joint was
lavaged thoroughly to remove all the debris, the arthroscopic
portals were sutured and the knee was compressed with a
bandage.
Postoperative rehabilitation
The rehabilitation training programs started soon
after surgery with all the patients instructed to perform isometric
quadricep exercises. The muscular training in the first week
following surgery was focused on the quadriceps femoris muscle,
including straight leg raises and Actimove GenuFlex movements, but
no weight loading. Active flexion and extension exercises of the
knee joint were performed in the second week, and patients could
walk with walking sticks. Dermal sutures were removed 14 days after
surgery, and four weeks after surgery, patients went back to normal
life and continued the above training.
Follow-up
Thirty-nine of the patients (43 knees) were followed
up for a mean of 21 months (ranging from 9 to 53 months). The
Lysholm scoring system (10,11)
was used to assess the function of the knee prior to surgery and
during the follow-up, and the results were compared using a
Student’s t-test with SPSS 12.0.
Results
Among the 47 knees, 37 received partial resection, 8
received hypo-complete resection and 2 had complete resection
(Table II).
 | Table IISurgical methods according to types of
tear patterns. |
Table II
Surgical methods according to types of
tear patterns.
| Type of surgical
method
| |
|---|
| Tear pattern | Partial
resection | Hypo-complete
resection | Complete
resection | Total |
|---|
| Simple
horizontal | 6 | 0 | 1 | 7 |
| Complicated
horizontal | 9 | 3 | 0 | 12 |
| Longitudinal | 10 | 2 | 1 | 13 |
| Radial | 6 | 2 | 0 | 8 |
| Degenerative | 4 | 0 | 0 | 4 |
| Complex | 2 | 1 | 0 | 3 |
| Total | 37 | 8 | 2 | 47 |
One patient had pain and swelling of the knee joint
postoperation, but the symptom disappeared 4 months after surgery.
Another patient suffered with hemarthrosis, and the symptom
disappeared following arthrocentesis. All the patients were
instructed to perform the rehabilitation training and returned to
normal activities within 4–6 weeks.
Knee function significantly improved postoperation,
and the clinical outcome was improved at 9 months compared to the
function after 3 months, as measured by Lysholm score (P<0.05),
showing the curative effect of meniscectomy (Table III).
 | Table IIIThe Lysholm score measured
preoperatively and postoperatively. |
Table III
The Lysholm score measured
preoperatively and postoperatively.
| Time | Lysholm score |
|---|
| Preoperative | 66.83±8.26 |
| 3 months after
operation | 91.48±3.01a |
| 9 months after
operation | 95.28±2.01b |
Discussion
Discoid lateral meniscus of the knee is common in
Asian populations (12,13). Unlike normal menisci, discoid
menisci cannot control the coordination of the tibiofemoral joint,
absorb shock, or reduce the mechanical pressure on articular
cartilage, thus they quickly become worn and are torn easily,
particularly when injured (14).
Atay et al (15) revealed
that the ultrastructure of discoid lateral menisci significantly
differs from that of normal menisci. The collagen fibrils in
discoid menisci are decreased in number and misaligned, both of
which contribute to an increased incidence of tears. Therefore we
suggested discoid menisci be treated by arthroscopy early, even
when asymptomatic.
MRI accurately displays a discoid meniscus and the
type, extent and position of the tear (16). In the present study, the use of
radiography in addition to MRI was useful, since it identifies and
tracks changes in the bone before and after surgery, including
osteoarthritis, rheumatoid arthritis, fracture and bone tumor. We
identified a widened lateral joint space in 13 knees by
radiography.
The traditional treatment for a discoid lateral
meniscus tear is to open the capsule and resect the meniscus, but
this often leads to arthritis development, particularly in children
who receive a total meniscectomy (17). With the recent advance in
arthoscopic surgical techniques and results from research on
healing function of meniscus arthroscopy, meniscal repair has now
become the technique of first choice to preserve menisci (18). The aim of the surgery is to remove
the central and torn parts of the discoid meniscus and to preserve
a stable peripheral rim as much as possible. Since the thick
discoid lateral meniscus is located within the space between knee
joints this affects the performance of the surgery, and a large
quantity of meniscal tissues has to be removed. It is much more
difficult to perform the shaping of the discoid meniscus (partial
resection) for a discoid lateral meniscus than for a normal one. In
our experience, bending the knee during the surgery and lowering
the lower leg along the side of the operation table to open up the
joint space via gravity, as well as using a suitable meniscus knife
and meniscus scissors, was helpful. When the discoid meniscus is
reshaped, the femoral surface should be resected more to form a
slope adapting to the shape of the femoral condyles. In our study,
among the 47 knees, 37 received partial resection (78.72%), 8
received hypo-complete resection (17.02%) and 2 received complete
resection (4.26%). Hayashi et al (9) suggested that the rim should be
retained to 6–8 mm in width, but the excessive thickness of a
complete-type discoid meniscus should be reduced substantially to
avoid new tears. In partial meniscectomies, a rim of 8 mm was
originally left for complete-type lesions and 10 mm for
incomplete-type lesions (the average width of normal menisci is
12–13 mm). We followed this standard in our study.
In conclusion, arthroscopic meniscectomy is an
effective treatment for discoid menisci resulting in maximal
meniscus preservation, minimal invasion, quick recovery and early
functional exercise.
References
|
1
|
Ahn JH, Choi SH, Lee YS, et al:
Symptomatic torn discoid lateral meniscus in adults. Knee Surg
Sports Traumatol Arthrosc. 19:158–164. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Smillie IS: The congenital discoid
meniscus. J Bone Joint Surg Br. 30B:671–682. 1948.PubMed/NCBI
|
|
3
|
Lu Y, Li Q and Hao J: Torn discoid lateral
meniscus treated with arthroscopic meniscectomy: observations in 62
knees. Chin Med J (Engl). 120:211–215. 2007.PubMed/NCBI
|
|
4
|
Washington ER III, Root L and Liener UC:
Discoid lateral meniscus in children. Long-term follow-up after
excision. J Bone Joint Surg Am. 77:1357–1361. 1995.PubMed/NCBI
|
|
5
|
Kramer DE and Micheli LJ: Meniscal tears
and discoid meniscus in children: diagnosis and treatment. J Am
Acad Orthop Surg. 17:698–707. 2009.PubMed/NCBI
|
|
6
|
Bellisari G, Samora W and Klingele K:
Meniscus tears in children. Sports Med Arthrosc. 19:50–55. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Woods GW and Whelan JM: Discoid meniscus.
Clin Sports Med. 9:695–706. 1990.PubMed/NCBI
|
|
8
|
Bin SI, Kim JC, Kim JM, Park SS and Han
YK: Correlation between type of discoid lateral menisci and tear
pattern. Knee Surg Sports Traumatol Arthrosc. 10:218–222. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hayashi LK, Yamaga H, Ida K and Miura T:
Arthroscopic meniscectomy for discoid lateral meniscus in children.
J Bone Joint Surg Am. 70:1495–1500. 1988.PubMed/NCBI
|
|
10
|
Ristić V, Ninković S, Harhaji V, Stanković
M, Savić D and Milankov M: Reconstruction of anterior cruciate
ligament by using two different techniques. Med Pregl. 63:845–850.
2010.(In Serbian).
|
|
11
|
Komárek J, Vališ P, Repko M, Chaloupka R
and Krbec M: Treatment of deep cartilage defects of the knee with
autologous chondrocyte transplantation: long-term results. Acta
Chir Orthop Traumatol Cech. 77:291–295. 2010.(In Czech).
|
|
12
|
Rao SK and Sripathi Rao P: Clinical,
radiologic and arthroscopic assessment and treatment of bilateral
discoid lateral meniscus. Knee Surg Sports Traumatol Arthrosc.
15:597–601. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fukuta S, Masaki K and Korai F: Prevalence
of abnormal findings in magnetic resonance images of asymptomatic
knees. J Orthop Sci. 7:287–291. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Murlimanju BV, Nair N, Pai MM,
Krishnamurthy A and Chandra Philip X: Morphology of the medial
meniscus of the knee in human fetuses. Rom J Morphol Embryol.
51:347–351. 2010.PubMed/NCBI
|
|
15
|
Atay OA, Pekmezci M, Doral MN, Sargon MF,
Ayvaz M and Johnson DL: Discoid meniscus: an ultrastructural study
with transmission electron microscopy. Am J Sports Med. 35:475–478.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yue BW, Gupta AK, Moorman CT III, Garrett
WE and Helms CA: Wrisberg variant of the discoid lateral meniscus
with flipped meniscal fragments simulating bucket-handle tear: MRI
and arthroscopic correlation. Skeletal Radiol. 40:1089–1094. 2011.
View Article : Google Scholar
|
|
17
|
Räber DA, Friederich NF and Hefti F:
Discoid lateral meniscus in children. Long-term follow-up after
total meniscectomy. J Bone Joint Surg Am. 80:1579–1586. 1998.
|
|
18
|
Stilli S, Marchesini Reggiani L,
Marcheggiani Muccioli GM, Cappella M and Donzelli O: Arthroscopic
treatment for symptomatic discoid lateral meniscus during
childhood. Knee Surg Sports Traumatol Arthrosc. 19:1337–1342. 2011.
View Article : Google Scholar : PubMed/NCBI
|