Introduction
Gorham-Stout syndrome is a rare skeletal disorder,
the etiology and pathogenesis of which remain unknown. Since the
first description by Jackson et al in 1838, no more than 200
cases have been reported (1,2). The
therapeutic procedure remains controversial owing to the rarity and
progressive osteolysis of this disease, while reconstructive
treatments are used in certain cases in an attempt to recover the
function of the bone involved. According to clinical records,
Gorham-Stout syndrome is usually initiated in a single bone (or
very few bones) or contiguous bones around one focus (1,2). The
maxillofacial skeleton is one region frequently affected. The first
maxillofacial case was described by Romer et al in 1928
(3). Since then, ∼50 maxillofacial
cases have been reported (4). In
the present study, a case of Gorham-Stout syndrome affecting the
left mandible in a 20-year-old male is presented.
Case report
A 20-year-old male patient presented with a 6-year
history of dental pain and progressive loosening of the posterior
teeth on the left mandible. A panoramic radiograph revealed
wide-ranging dissolution of the left mandible, while no periosteal
reaction or reactive new bone formation were observed around the
residual bone tissues (Fig. 1). A
CT scan of the craniofacial region corroborated X-ray results, and
further revealed that the osteolytic bone ranged from the left
ramus to the second premolar, with a continuation of the lower
margin of the left mandible only. The teeth appeared to float in
the osteolytic tissues (Fig. 2A).
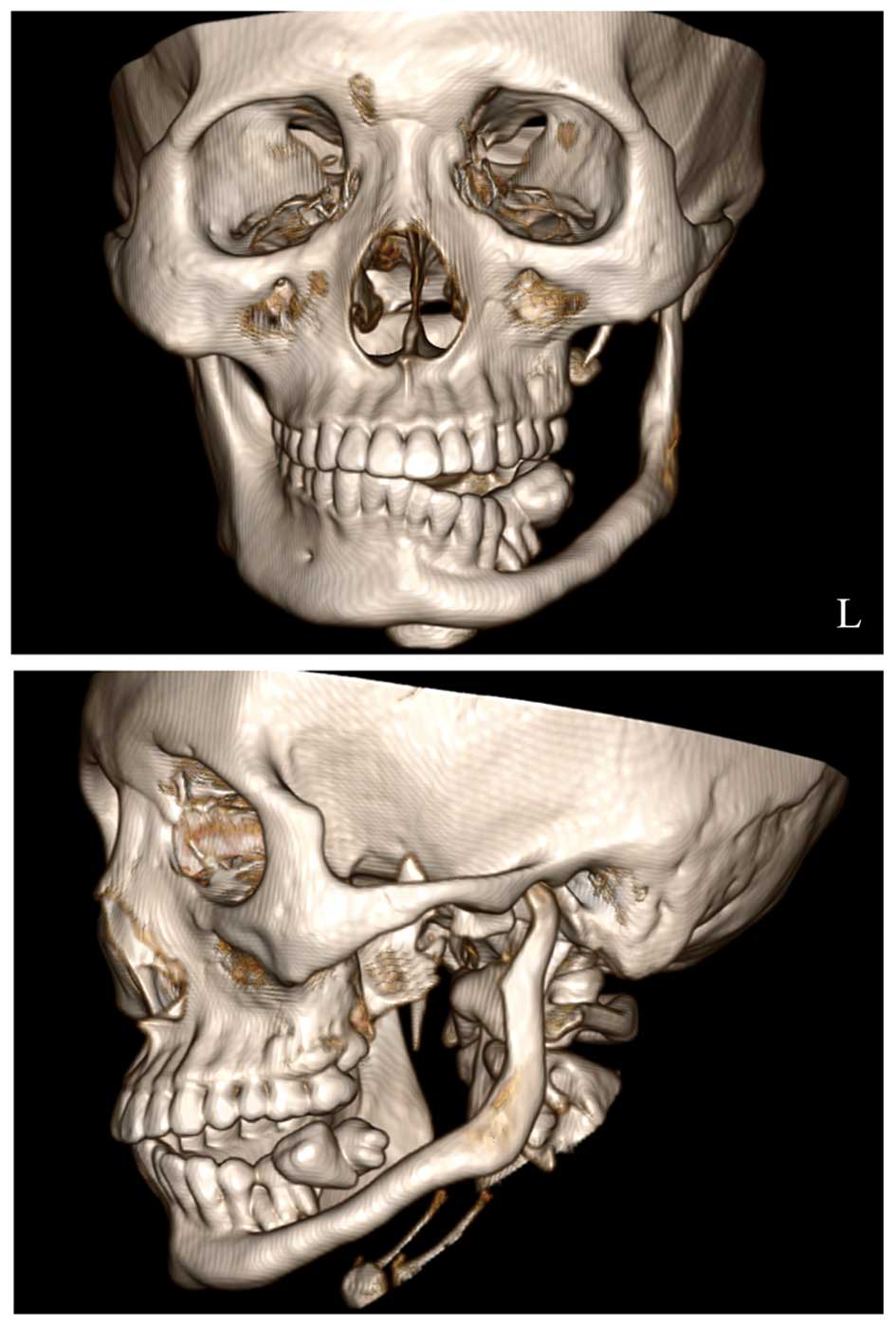
Three-dimensional reconstruction CT images indicated that the left
temporomandibular joint remained uninvolved (Fig. 3).
An initial diagnosis of pericoronitis of the wisdom
tooth was issued by the patient’s local primary hospital. Following
anti-inflammatory therapy, the dental pain was temporarily relieved
but the progressive tooth loosening was also aggravated. In 2009,
the chewing function in the left mandibular area was completely
lost. Dental radiology at that time indicated massive osteolysis of
the left mandible, however, the patient refused further
examinations and therapy.
In May 2012, the patient was referred to our
hospital due to an enlarging mass in the left mandible. CT and MRI
images showed a 38×43×75-mm, irregular, thick-walled cystic mass in
the left ramus of the mandible (Fig.
2B and C). Standard laboratory investigations, including bone
metabolism tests, revealed no abnormality. A skeletal survey
revealed no other osseous involvement. The loosening posterior
teeth (4–8) were extracted during exploratory
surgery and a large quantity of pus was spilled from the incision
area. Following repeated rinsing with sterile saline, the wound was
sutured. Histopathological examination of the bone biopsy showed
proliferation of the fibrous connective tissue, intermixed with
irregular bony trabeculae (Fig.
2D). Tissues obtained from the cystic wall were also sent for
histopathological examination, but only inflammation and
granulation tissue formation were revealed.
On the basis of the clinical, radiographic and
histopathological results, a diagnosis of Gorham-Stout syndrome was
made. Radiotherapy and etidronate therapy were proposed to the
patient, but were not accepted. At present, the patient remains
under observation. The study was approved by the ethics committee
of Wuhan General Hospital of Guangzhou Command. Written informed
patient consent was obtained from the patient.
Discussion
Numerous studies concerning the etiopathology and
clinical presentation of Gorham-Stout syndrome have been reported,
along with radiographic findings and therapeutic options, in order
to raise the awareness of this rare disease.
Debates over the presence of osteoclasts in
Gorham-Stout syndrome reveal the uncertainty of researchers about
the exact etiopathology of the condition. Certain researchers
consider that angiomatosis of the blood vessels and occasionally of
the lymphatics is responsible (3),
while others consider that a previous trauma must be involved
(5). However, a definite etiology
has not been established thus far.
The clinical presentation of Gorham-Stout syndrome
is variable depending on the affected sites. Certain patients have
presented with a relatively abrupt onset of pain and swelling or a
pathological fracture on the affected site, whereas others have
presented with a history of an insidious onset of pain, limitation
of motion and progressive weakness in the affected area (3). The disease is not usually accompanied
by any systemic symptoms (6). In
most cases, the bone resorption process may stop spontaneously, and
therefore the prognosis is generally good unless vital structures
are involved.
A final diagnosis of Gorham-Stout syndrome is
difficult. Laboratory findings are not specific and are of no value
in the diagnostic procedure. Radiographs provide the most
significant clues for obtaining a diagnosis. In early X-rays,
Johnson and McClure (7) noted
evidence of one or multiple centromedullary and subcortical
radioluciencies, usually with indistinct margins and no sclerotic
borders. Later, these lesions may enlarge and fuse together,
causing a disruption of the cortex and then intraosseous and
extraosseous resorption (7). CT
scanning and three-dimensional reconstruction are more useful for
accurately assessing the range of bone destruction at the time of
diagnosis. MRI is used to define the extent of vascular formation
and the involvement of the adjacent soft tissue. The histological
findings depend on the phase in which the disease is diagnosed. In
the first of the two phases, the bone-displacing fibrous tissue
section exhibits a higher concentration of blood vessels, whereas
only fibrous tissue is detected in the second phase (5,8).
Hereditary and essential osteolysis, tumours, skeletal angiomas,
infection and other causes of osteolysis should all be ruled out
before a differential diagnosis of Gorham-Stout is made (9). Notably, the cystic mass in the
present study emerged at the beginning of 2012, which is later than
the appearance of the osteolysis of the left mandible. Therefore,
it may be considered as a complication of Gorham-Stout
syndrome.
Due to the rarity of this disease, there is no
standard therapy available. The treatment modalities include
surgery, radiotherapy, etidronate therapy and the use of α-2b
interferon (1,3). In the present study, as there has
been no marked progression in mandibular resorption since 2009, the
patient and his family have refused any offer of further treatment
and the patient’s condition is being observed via clinical
follow-up.
Taking all the evidence together, considering the
history and clinical manifestations and the radiographic and
histopathological results, the diagnosis of Gorham-Stout syndrome
in this case was considered to be reasonable and logical.
References
|
1
|
Heyd R, Micke O, Surholt C, et al German
Cooperative Group on Radiotherapy for Benign Diseases (GCG-BD):
Radiation therapy for Gorham-Stout syndrome: results of a national
patterns-of-care study and literature review. Int J Radiat Oncol
Biol Phys. 81:e179–e185. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lehmann G, Pfeil A, Böttcher J, et al:
Benefit of a 17-year long-term bisphosphonate therapy in a patient
with Gorham-Stout syndrome. Arch Orthop Trauma Surg. 129:967–972.
2009.PubMed/NCBI
|
|
3
|
Gondivkar SM and Gadbail AR: Gorham-Stout
syndrome: a rare clinical entity and review of literature. Oral
Surg Oral Med Oral Pathol Oral Radiol Endod. 109:e41–e48. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Escande C, Schouman T, Françoise G, et al:
Histological features and management of a mandibular Gorham
disease: a case report and review of maxillofacial cases in the
literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
106:e30–e37. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Silva S: Gorham-Stout disease affecting
both hands: stabilisation during biphosphonate treatment. Hand
(NY). 6:85–89. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rao P, Kotwal PP and Goel S: Painless
destruction of the shoulder joint: a case report. Clin Rheumatol.
20:143–146. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Johnson PM and McClure JG: Observations on
massive osteolysis; a review of the literature and report of a
case. Radiology. 71:28–42. 1958. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Heffez L, Doku HC, Carter BL and Feeney
JE: Perspectives on massive osteolysis. Report of a case and review
of the literature. Oral Surg Oral Med Oral Pathol. 55:331–343.
1983. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Holroyd I, Dillon M and Roberts GJ:
Gorham’s disease: a case (including dental presentation) of
vanishing bone disease. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod. 89:125–129. 2000.
|