Introduction
Although organ transplantation has been successful
for decades, graft rejection and immunosuppression (IS)-derived
chronic toxicity remain as key problems which need to be overcome.
However, in comparison with the majority of transplant recipients
who have extreme difficulty achieving an IS-free state following
transplantation, a significantly higher proportion of liver
transplant recipients achieve clinical operational tolerance
(1). Moreover, liver allografts
are able to protect co-transplanted organs from rejection (2–4),
suggesting that the liver, unlike other solid organs such as the
kidney or heart, is an immunoprivileged organ. Notably, although
liver allografts are the most spontaneously accepted
transplantations in a number of species, hepatocyte allografts
alone are acutely rejected (5,6),
suggesting that liver non-parenchymal cells (NPCs), including
resident dendritic cells (DCs), liver sinusoid endothelial cells
(LSECs), Kupffer cells (KCs) and hepatic stellate cells (HSCs), are
considerably involved in liver immunotolerance. Previous studies
have indicated that NPCs mediate immunosuppresion via a variety of
mechanisms, including the secretion of anti-inflammatory cytokines
and the induction of T-cell apoptosis (7), However, the underlying mechanism is
not yet completely understood.
HSCs (vitamin A-storing cells, lipocytes,
interstitial cells, fat-storing cells and Ito cells), exist in the
space between the hepatocytes and LSECs of the hepatic lobule and
are well known for their functions of regulating retinoid
homeostasis and participating in the pathogenesis of liver
fibrogenesis. In addition, HSCs have been demonstrated to be
antigen-presenting cells (APCs) and tolerogenic (8). Activated HSCs express negative
co-stimulator B7-H1 which inhibits T-cell responses via the
mediation of T-cell apoptosis (9).
Previous studies have revealed that co-transplanted HSCs protect
islet allografts from rejection and attenuate the severity of
graft-versus-host disease (10,11),
suggesting that the HSCs have immunosuppressive properties. The
present study revealed that HSCs are involved in liver transplant
immunotolerance via T-cell apoptosis partly mediated by the
Fas/FasL pathway and the regulation of TGF-β and IL-10
production.
Materials and methods
Animals
Male Dark Agouti (DA) and Lewis rats, aged between
10 and 12 weeks and weighing 220–250 g (Vital River Laboratory
Animal Technology Co., Ltd., Beijing, China) were maintained in a
pathogen-free animal facility. The rats were allowed free access to
tap water and food. The animal procedures were approved by the
Institutional Animal Care Committee.
Orthotopic liver transplantation
Previous studies have shown that liver grafts are
spontaneously accepted in Lewis to DA transplantations, while DA to
Lewis liver allograft recipients suffer from severe rejection
(12). The present study included
a tolerance group (Lewis into DA, n=5) and rejection group (DA into
Lewis, n=5). The liver transplantation was performed according to
the ‘2 cuff technique’ of Kamada and Calne (13). Briefly, after anesthesia and
systemic heparinization, the livers were removed from the donors
and prepared in 4°C Ringer’s solution. The grafts were then
implanted into the recipients by anastomosis of the suprahepatic
vena cava using a continuous everting suture, reconstruction of the
portal vein and infra-hepatic vena cava by the cuff technique and
connection of bile duct by an end-to-end anastomosis over an
indwelling stent without hepatic artery reconstruction. After
surgery, the recipients were kept warm by lighting and had free
access to food and water. Rats deaths within 5 days after
transplantation were considered to be due to technical failures and
hence excluded from the study.
Histological examination
Tissue specimens from the liver grafts were fixed in
4% formalin, embedded in paraffin and used for histological
examination. The specimens were then sliced into 5-μm
sections and stained with hematoxylin and eosin (H&E) for
routine histological examination.
Isolation of HSCs
On the 7th day after transplantation, the recipient
rats were sacrificed. A 0.5×1.0 cm liver tissue specimen was
obtained from each liver graft for histological examination. HSCs
were then extracted from the left liver tissue as previously
described (14–16). Briefly, the grafts underwent serial
in situ perfusions with 70 ml 0.1% pronase at a flow rate of
10–15 ml/min for 7 min and 60 ml 0.05% collagenase IV (Sigma, St.
Louis, MO, USA) at a flow rate of 10–15 ml/min for 20 min. The
liver tissue was then digested in 50 ml buffer solution containing
collagenase IV, pronase and DNase (Sigma), followed by density
gradient centrifugation and 11% Nycodenz (Axis-Shield PoC, Oslo,
Norway) gradient centrifugation. The harvested HSCs were
resuspended in high glucose Dulbecco’s modified Eagle’s medium
(DMEM; Gibco-BRL, Grand Island, NY, USA) containing 20% fetal calf
serum (FCS). The viability of HSCs was >90% as determined using
trypan blue exclusion and the purity of HSCs ranged from 90 to 95%
as determined by desmin immunostaining. The typical light
microscopic appearance of a lipid droplet was as described
previously (17). The HSCs were
cultured in DMEM containing 20% FCS for 7 days for further
study.
Preparation of T cells
The spleens of the recipient rats were removed on
the 7th day after transplantation and single spleen cell (SC)
suspensions were prepared. Following lysis of red blood cells and
density gradient centrifugation, T cells were isolated and purified
using an adherence culture in DMEM containing 10% FCS and a nylon
wool column.
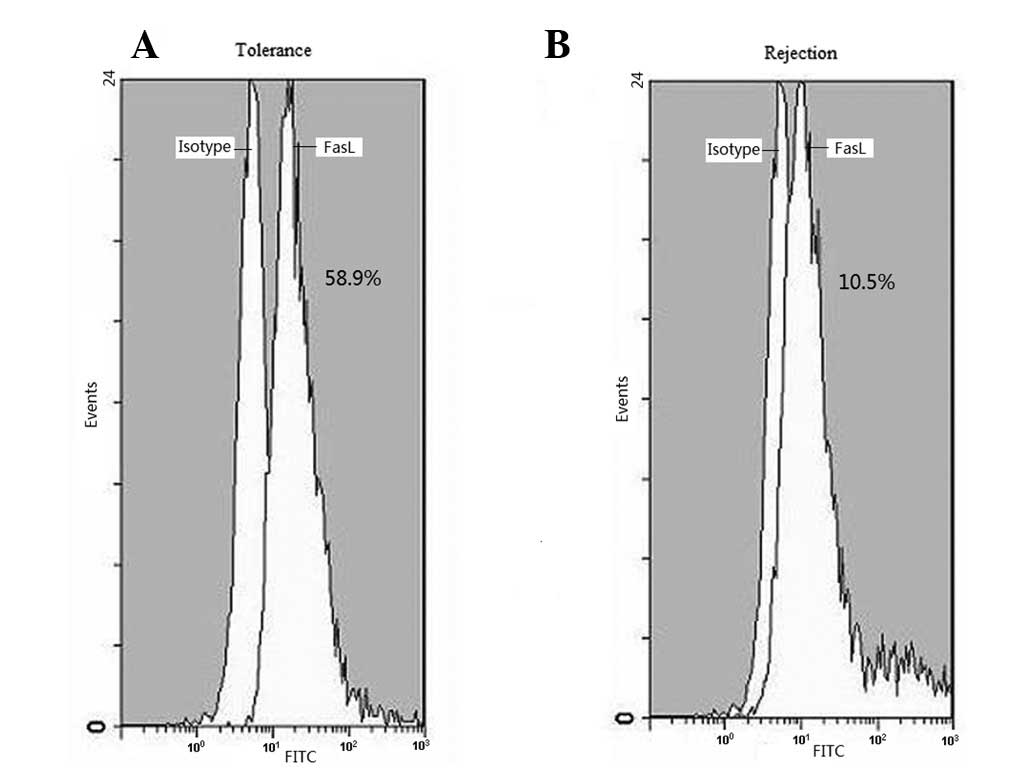
FasL expression in HSCs
HSCs (2.5×104) were incubated with
mitomycin C (10 μg/ml) for 30 min at 37°C in a 5%
CO2-humidified air atmosphere. Then, HSCs were stained
with Hamster monoclonal anti-rat FasL-specific IgG (eBioscience,
San Diego, CA, USA) followed by a second fluorescein-labeled
antibody (BD Pharmingen, San Diego, CA, USA). The FasL expression
levels of the HSCs were determined by flow cytometry according to
the manufacturer’s instructions.
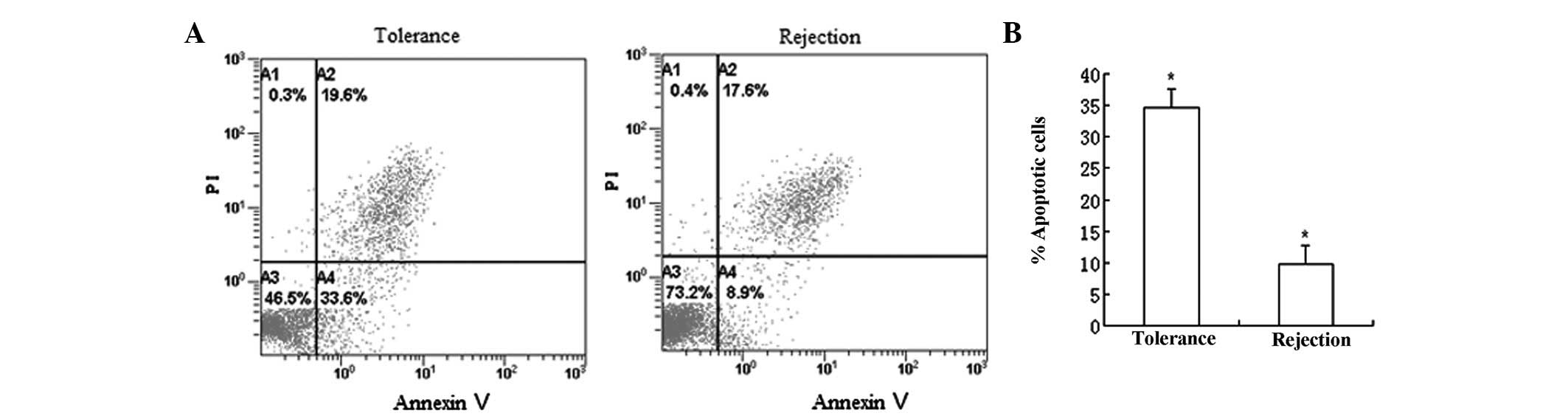
Flow cytometry analysis for alloreactive
T-cell apoptosis
After incubating with mitomycin C (10 μg/ml)
for 30 min, the HSCs (2.5×104) were resuspended in 100
μl DMEM containing 10% FCS and then co-cultured with 100
μl T cells (5×105) in the presence or absence of
FasL blocking mAb for 24 h. All cultures were incubated at 37°C in
a 5% CO2-humidified air atmosphere. The nonadherent
cells were isolated and the apoptotic T cells stained with anti-CD3
mAb (eBioscience) and Annexin V-FITC/PI (BD Pharmingen) were
determined by flow cytometry according to the manufacturer’s
instructions.
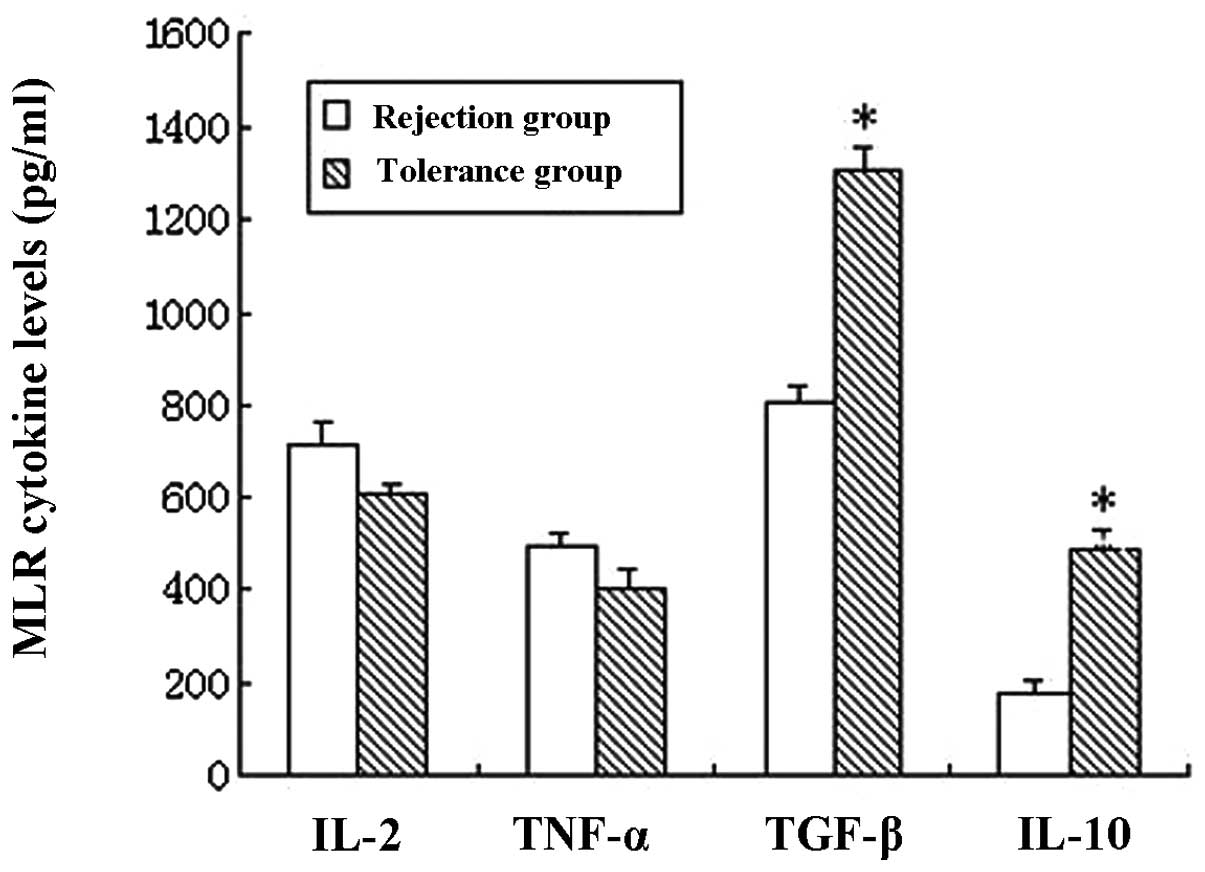
Cytokine quantitation
A two-way mixed lymphocyte reaction (MLR) was
performed and 2.5×105 Lewis and 2.5×105 DA
SCs were co-cultured in 96-well plates (200 μl) in DMEM
containing 10% FCS, 100 U/ml penicillin and 100 mg/ml streptomycin,
in the presence of 2.5×104 HSCs. This co-culture was
incubated at 37°C in a 5% CO2-humidified air atmosphere
for 5 days. The IL-2, IL-10, TNF-α and TGF-β levels in the
supernatant of this co-culture were quantified using the respective
ELISA kits (Biosource International Inc, Camarillo, CA, USA). A
standard curve using recombinant cytokine was generated for each
assay.
Statistical analysis
The data are presented as the mean ± standard
deviation (SD). The statistical significance of the parametric data
was determined using the Student’s t-test. P<0.05 was considered
to indicate a statistically significant difference.
Results
Histological characteristics of the liver
grafts
Histological analysis confirmed that the liver
grafts of the rejection group underwent serious acute rejection,
while those of the tolerance group did not. In the rejection group,
the H&E staining results showed severe acute rejection, which
was characterized by extensive T-cell infiltration of the portal
tracts; bile duct damage; vacuolar degeneration, karyopycnosis and
even necrosis of hepatocytes. Meanwhile, the tolerance group
exhibited only minimal T-cell infiltration without portal tract
involvement and the hepatic parenchyma exhibited no significant
damage (Fig. 1).
HSCs induce T-cell apoptosis through the
Fas/FasL pathway
As T-cell apoptosis is a well-established mechanism
of liver immunotolerance (18), we
hypothesized that HSCs may contribute to liver immunotolerance by
inducing T-cell apoptosis. The results indicated that the HSCs of
the tolerance group had significantly higher FasL expression than
the rejection group (Fig. 2).
Furthermore, the results also showed that the HSCs of the tolerance
group were able to markedly enhance the apoptosis of T cells,
suggesting that the immunosuppressive effect of HSCs may induce
T-cell apoptosis (Fig. 3). The
Fas/FasL is a well-known pathway of apoptosis (19). To determine whether Fas/FasL was
critical in HSC-induced T-cell apoptosis, HSCs were co-cultured
with T cells in the presence or absence of FasL blocking mAb. FasL
blocking mAb partially but significantly inhibited T-cell apoptosis
in the tolerance group (P<0.05) and had little effect in the
rejection group (P>0.05; Figs.
4 and 5).
HSCs promote Th2/Th3-like cell cytokine
production in the tolerance group
The IL-2, TNF-α, TGF-β and IL-10 cytokine levels in
the supernatant of the MLR cultures in the presence of HSCs were
measured using ELISA assays. The results indicated that there were
no significant differences in the Th1 cytokine (IL-2 and TNF-α)
levels between the tolerance and rejection groups (P>0.05).
However, in the tolerance group, the Th2-like cell cytokine IL-10
and Th3-like cell cytokine TGF-β levels were markedly increased
(P<0.05; Fig. 6).
Discussion
Unlike other solid organs, liver allografts may be
spontaneously accepted without IS in a number of species, including
humans, demonstrating that the liver is an immunoprivileged organ
(1,20–22).
Moreover, an accumulating amount of evidence suggests that NPCs,
such as DCs, KCs and LSECs, are critical in liver transplant
immunotolerance (23–25). HSCs are a type of NPC, well known
for their key role in liver fibrogenesis. Additionally, HSCs have
been demonstrated to be immunoregulating (8–10).
In the present study, the activated HSCs from the
tolerance group had an increased T-cell apoptosis-inducing
activity, indicating that activated HSCs have an immune suppressive
function, since induced T-cell apoptosis is a significant mechanism
in the development of immune tolerance (18). The present data also showed that in
the tolerance group, the expression of FasL by HSCs was
significantly higher than in the rejection group. Moreover, FasL
blocking mAb partially but significantly reversed HSC-induced
T-cell apoptosis in the tolerance group but not in the rejection
group, suggesting that the Fas/FasL pathway is associated with
HSC-induced T-cell apoptosis. It is generally accepted that Fas and
FasL interactions are key to cell apoptosis and maintain the
immunoprivilege (19). Moreover,
other studies have revealed that the Fas system is involved in
liver transplant immune regulation. Specifically, FasL expressed by
infiltrating cells induces liver cell apoptosis during acute
rejection following liver transplantation. However, the increased
expression of FasL in liver allografts results in immunotolerance
by combining with Fas expressed by the infiltrating lymphocytes
(26,27). This phenomenon may be explained by
the expression of FasL gradually switching from infiltrating cells
to hepatocytes. Sun et al observed that KCs in the liver
downregulate the T-cell response via the Fas/FasL pathway following
liver transplantation. The authors results indicated that the
Fas/FasL pathway was involved in the immunotolerance of liver
transplantation (24). However,
FasL may not be the only molecule involved in the immunosuppressive
effect of HSCs, since the blocking of FasL only partially reversed
HSC-induced T-cell apoptosis. Studies have further demonstrated
that the upregulation of B7-H1 suppresses T-cell proliferation,
promotes T-cell apoptosis and induces the production of various
cytokines by combining with programmed death-1 (PD-1) B and T
lymphocyte attenuator. Therefore, B7-H1 is considerably involved in
peripheral immune tolerance and tumor immune evasion (28,29).
B7-H1 negatively regulates the immune system and inhibits T-cell
activity, mainly at the effect phase since B7-H1 receptor PD-1 is
inducibly expressed on activated T cells (30–32).
Deficiencies of B7-H1 lead to the accumulation of CD8+ T
cells in the liver, suggesting a role for B7-H1 in the regulation
of T-cell homeostasis (33). A
study by Yu et al showed that quiescent HSCs express very
low levels of B7-H1, while B7-H1 expression in HSCs may be notably
increased by various stimuli and the inhibition of B7-H1 may
partially reduce HSC-induced T-cell apoptosis (9). Therefore, we propose that the B7-H1
and Fas/FasL pathways are involved in HSC-induced immune
suppression.
The present study also showed that there were higher
IL-10 and TGF-β levels in the supernatant of the MLR cultures of
HSC and T cells from the tolerance group. We hypothesize that HSCs
may drive the T-cell subset differentiation of Th2/Th3 cells or
activate the production of inhibitory cytokines, such as IL-10
and/or TGF-β, by HSCs. Th1-like cell cytokines mediate cellular
immunity and enhance rejection, while Th2-like cell cytokines
downregulate the activity of Th1-like cells and cytotoxic T
lymphocytes (CTL) and attenuate post-transplantation rejection. It
has been reported that IL-10 and TGF-β contributed to liver
transplant immunotolerance (34,35).
Studies have also demonstrated that KCs and LSECs negatively
regulate the immune response by secreting TGF-β (35). Therefore, HSCs may regulate the
immune response following liver transplantation by regulating
Th2/Th3-like cell cytokine production.
In conclusion, the present study revealed that HSCs
contribute to liver transplant immunotolerance by inducing T-cell
apoptosis and stimulating Th2/Th3-like cell cytokine production.
This immunosuppressive activity of HSCs provides a supplementary
mechanism for the development of immunotolerance following liver
transplantation.
Acknowledgements
This study was supported by the
Foundation for Innovative Research Groups of the National Natural
Science Foundation of China (No.81121002) and Zhejiang Provincial
Natural Science Foundation of China (No.Y 2100498).
References
|
1
|
Orlando G, Soker S and Wood K: Operational
tolerance after liver transplantation. J Hepatol. 50:1247–1257.
2009. View Article : Google Scholar
|
|
2
|
Zhong R, He G, Sakai Y, Li XC, Garcia B,
Wall W, Duff J, Stiller C and Grant D: Combined small bowel and
liver transplantation in the rat: possible role of the liver in
preventing intestinal allograft rejection. Transplantation.
52:550–552. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wang C, Sun J, Wang L, Li L, Horvat M and
Sheil R: Combined liver and pancreas transplantation induces
pancreas allograft tolerance. Transplant Proc. 29:1145–1146. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sarnacki S, Révillon Y, Cerf-Bensussan N,
Calise D, Goulet O and Brousse N: Long-term small-bowel graft
survival induced by a spontaneously tolerated liver allograft in
inbred rat strains. Transplantation. 54:383–385. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bumgardner GL and Orosz CG: Unusual
patterns of alloimmunity evoked by allogeneic liver parenchymal
cells. Immunol Rev. 174:260–279. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bumgardner GL, Heininger M, Li J, Xia D,
Parker-Thornburg J, Ferguson RM and Orosz CG: A functional model of
hepatocyte transplantation for in vivo immunologic studies.
Transplantation. 65:53–61. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tiegs G and Lohse AW: Immune tolerance:
what is unique about the liver. J Autoimmun. 34:1–6. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Winau F, Hegasy G, Weiskirchen R, Weber S,
Cassan C, Sieling PA, Modlin RL, Liblau RS, Gressner AM and
Kaufmann SH: Ito cells are liver-resident antigen-presenting cells
for activating T cell responses. Immunity. 26:117–129. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yu MC, Chen CH, Liang X, Wang L, Gandhi
CR, Fung JJ, Lu L and Qian S: Inhibition of T cell responses by
hepatic stellate cells via B7-H1-mediated T-cell apoptosis in mice.
Hepatology. 40:1312–1321. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chen CH, Kuo LM, Chang Y, Wu W, Goldbach
C, Ross MA, Stolz DB, Chen L, Fung JJ, Lu L and Qian S: In vivo
immune modulatory activity of hepatic stellate cells in mice.
Hepatology. 44:1171–1181. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chen CH, Shu KH, Su YH, Tang KY, Cheng CH,
Wu MJ, Yu TM, Chuang YW and Hu C: Cotransplantation of hepatic
stellate cells attenuates the severity of graft-versus-host
disease. Transplant Proc. 42:971–975. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kamada N: The immunology of experimental
liver transplantation in the rat. Immunology. 55:369–389.
1985.PubMed/NCBI
|
|
13
|
Kamada N and Calne RY: Orthotopic liver
transplantation in the rat. Technique using cuff for portal vein
anastomosis and biliary drainage. Transplantation. 28:47–50. 1979.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Niki T, Pekny M, Hellemans K, Bleser PD,
Berg KV, Vaeyens F, Quartier E, Schuit F and Geerts A: Class VI
intermediate filament protein nestin is induced during activation
of rat hepatic stellate cells. Hepatology. 29:520–527. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Iredale JP, Benyon RC, Pickering J,
McCullen M, Northrop M, Pawley S, Hovell C and Arthur MJ:
Mechanisms of spontaneous resolution of rat liver fibrosis hepatic
stellate cell apoptosis and reduced hepatic expression of
metalloproteinase inhibitors. J Clin Invest. 102:538–549. 1998.
View Article : Google Scholar
|
|
16
|
Lang A, Schoonhoven R, Tuvia S, Brenner DA
and Rippe RA: Nuclear factor kappaB in proliferation, activation,
and apoptosis in rat hepatic stellate cells. J Hepatol. 33:49–58.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Liu C, Gaça MD, Swenson ES, Vellucci VF,
Reiss M and Wells RG: Smads 2 and 3 are differentially activated by
transforming growth factor-beta (TGF-beta) in quiescent and
activated hepatic stellate cells. Constitutive nuclear localization
of Smads in activated cells is TGF-beta-independent. J Biol Chem.
278:11721–11728. 2003. View Article : Google Scholar
|
|
18
|
Qian S, Lu L, Fu F, Li Y, Li W, Starzl TE,
Fung JJ and Thomson AW: Apoptosis within spontaneonsly accepted
mouse liver allografts: evidence for deletion of cytotoxic T cells
and implications for tolerance induction. J Immunol. 158:4654–4661.
1997.
|
|
19
|
Griffith TS, Brunner T, Fletcher SM, Green
DR and Ferguson TA: Fas ligand-induced apoptosis as a mechanism of
immune privilege. Science. 270:1189–1192. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Garnier H, Clot JP, Bertrand M, Camplez P,
Kunlin A, Gorin JP, Le Goaziou F, Lévy R and Cordier G: Liver
transplantation in the pig: surgical approach. C R Acad Sci Hebd
Seances Acad Sci D. 260:5621–5623. 1965.(In French).
|
|
21
|
Kamada N, Brons G and Davies HS: Fully
allogeneic liver grafting in rats induces a state of systemic
nonreactivity to donor transplantation antigens. Transplantation.
29:429–431. 1980. View Article : Google Scholar
|
|
22
|
Qian S, Demetris AJ, Murase N, Rao AS,
Fung JJ and Starzl TE: Murine liver allograft transplantation:
tolerance and donor cell chimerism. Hepatology. 19:916–924. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Fairchild PJ and Waldmann H: Dendritic
cells and prospects for transplantation tolerance. Curr Opin
Immunol. 12:528–535. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Sun Z, Wada T, Maemura K, Uchikura K,
Hoshino S, Diehl AM and Klein AS: Hepatic allograft-derived Kupfer
cells regulate T cell response in rats. Liver Transpl. 9:489–497.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Limmer A and Knolle PA: Liver sinusoidal
endothelial cells: a new type of organ-resident antigen-presenting
cell. Arch Immunol Ther Exp (Warsz). 49(Suppl 1): S7–S11.
2001.PubMed/NCBI
|
|
26
|
Pan TL, Goto S, Lin YC, Lord R, Chiang KC,
Lai CY, Chen YS, Eng HL, Cheng YF, Tatsuma T, Kitano S, Lin CL and
Chen CL: The fas and fas 1igand pathways in liver allograft
tolerance. Clin Exp Immunol. 118:180–187. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Rivero M, Crespo J, Mayorga M, et al:
Involvement of the Fas system in liver allograft rejection. Am J
Gastroenterol. 97:1501–1506. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Selenko-Gebauer N, Majdic O, Szekeres A,
Höfler G, Guthann E, Korthäuer U, Zlabinger G, Steinberger P, Pickl
WF, Stockinger H, Knapp W and Stöckl J: B7-H1 (Programmed death-1
ligand) on dendritic cells is involved in the induction and
maintenance of T cell anergy. J Immunol. 170:3637–3644. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Dong H, Strome SE, Salomao DR, Tamura H,
Hirano F, Flies DB, Roche PC, Lu J, Zhu G, Tamada K, Lennon VA,
Celis E and Chen L: Tumor-associated B7-H1 promotes T-cell
apoptosis: a potential mechanism of immune evasion. Nat Med.
8:793–800. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Lu L, Qian S, Hershberger PA, Rudert WA,
Lynch DH and Thomson AW: Fas ligand (CD95L) and B7 expression on
dendritic cells provide counterregulatory signals for T cell
survival and proliferation. J Immunol. 158:5676–5684.
1997.PubMed/NCBI
|
|
31
|
Savage CO, Hughes CC, Pepinsky RB, Wallner
BP, Freedman AS and Pober JS: Endothelial cell lymphocyte
function-associated antigen-3 and an unidentified ligand act in
concert to provide costimulation to human peripheral blood CD4+ T
cells. Cell Immunol. 137:150–163. 1991.PubMed/NCBI
|
|
32
|
Chen L: B7-H1 connection of innate and
adoptive immunity against tumor dormancy. Blood. 105:2242–2243.
2005. View Article : Google Scholar
|
|
33
|
Subudhi SK, Alegre ML and Fu YX: The
balance of immune responses: costimulation verse coinhibition. J
Mol Med (Berl). 83:193–202. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Fernandes H, Koneru B, Fernandes N, Hameed
M, Cohen MC, Raveche E and Cohen S: Investigation of promoter
polymorphisms in the tumor necrosis factor-alpha and interleukin-10
gene in liver transplant patients. Transplantation. 73:1886–1891.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Karrar A, Broomé U, Uzunel M, Qureshi AR
and Sumitran-Holgersson S: Human liver sinusoidal endothelial cells
induce apoptosis in activated T cells: a role in tolerance
induction. Gut. 56:243–252. 2007. View Article : Google Scholar : PubMed/NCBI
|