Introduction
Implantation of an inferior vena cava (IVC) filter
is safe and effective in the prevention or reduction of fatal
pulmonary embolism (PE). However, there are risks associated with
long-term implantation of these filters, including IVC occlusion,
thrombosis and the recurrence of deep venous thrombosis (1–3).
Thrombus within an IVC filter reduces filter patency
and venous return from the lower extremities, and may progress to
complete IVC occlusion. Depending on collateral formation and the
extent of venous involvement and valvular damage, the long-term
sequelae of IVC thrombosis may range from mild ambulatory lower
extremity swelling to incapacitating edema at rest, venous
claudication and/or venous ulcers. In addition, filter thrombosis
may result in recurrent PE secondary to thrombus propagation above
the filter (4,5). Renal failure secondary to IVC filter
thrombus propagation into the renal veins has been reported
(6–8). If untreated or inadequately treated,
this condition may cause debilitating lower extremity pain and
swelling, back pain, weakness and venous stasis ulceration.
Conservative therapy (pneumatic and elastic compression, leg
elevation and/or anticoagulation) alone is usually inadequate to
relieve symptoms, and venous bypass surgery has been the only
option in the most severe cases and has had limited efficacy and
applicability (9). Transcatheter
thrombolytic therapy has demonstrated short-term effectiveness in
the treatment of patients with iliofemoral deep vein thrombosis
(DVT) and limited numbers of patients with IVC thrombosis (10–14).
We have employed transcatheter thrombolysis to treat
patients who have developed symptomatic IVC thrombosis following
filter implantation elsewhere and have been referred to the
Radiology department of the First hospital of China Medical
University. In the present study, we describe the clinical
experiences and outcomes of five cases complicated by
acutely/subacutely symptomatic IVC thrombosis following filter
implantation.
Patients and methods
Patients
Institutional review board approval was obtained
from the ethics committee of the First Hospital of China Medical
University for this study. Between October 2005 and September 2010,
5 patients were referred to our department with symptomatic IVC
thrombosis following filter implantation. The patients comprised 5
males, with a mean age of 34.2 years (range, 17–54 years). The
onset time was from 2 to 30 days. Symptoms included bilateral lower
limb swelling (n=5), pain (n=1), cyanosis (n=2) or pallescence
(n=3) and rising (n=3) skin temperature. Patient demographics,
symptoms, indication for filter placement, filter type, the
interval between filter placement and symptoms emerging and the
interval between symptoms emerging and transcatheter thrombolysis
for each patient are recorded in Table
I. Interventional surgery was performed after informed consent
was obtained from the patient.
 | Table I.Demographic and clinical
characteristics of the patients. |
Table I.
Demographic and clinical
characteristics of the patients.
| Case no. | Gender/age
(years) | Type of filter | Indication for filter
implantation | Interval between
filter implantation and symptoms emerging | Symptoms of IVC
occlusion | Interval between
symptoms emerging and thrombolysis |
|---|
| 1 | M/17 | Vena Tech | Left DVT | 5 days | Swelling and pain in
both LE | 2 days |
| 2 | M/24 | OptEase | Right DVT | 7 days | Swelling in both
LE | 3 days |
| 3 | M/28 | Vena Tech | Left DVT | 25 months | Swelling in both
LE | 5 days |
| 4 | M/54 | OptEase | Left DVT | 10 months | Swelling in both
LE | 30 days |
| 5 | M/48 | OptEase | Right DVT | 21 months | Swelling in both
LE | 7 days |
Filter implantation and IVC transcatheter
thrombolysis
Through the right jugular vein approach, a 5-Fr
pig-tail catheter was placed into the IVC above the filter. An
anteroposterior cavogram was performed to ensure the location of
the previous IVC filter, the extent of IVC thrombosis, the fluency
of the bilateral renal veins and the diameter of the suprarenal
IVC. After confirming that the suprarenal IVC was free of thrombus,
an 8.5-Fr sheath was inserted into the IVC. An OptEase filter
(Cordis Corp., Miami Lakes, FL, USA) or a Günther Tulip filter
(GTF; Vena Cava MReye Filter set; William Cook Europe, Bjaeverskov,
Denmark) was placed into the sheath and moved forward until the
distal end of the filter reached 1–2 cm above the level of the
renal vein confluence. The sheath was slowly withdrawn, allowing
the filter to enter the caval lumen and unfold. After ensuring that
the filter was suitably located and free of tilt, the retrieval
hook of the GTF was released.
After excluding PE by an anteroposterior pulmonary
arteriogram, a 5-Fr curved catheter over a 0.035-inch hydrophilous
guide wire was placed into the IVC above the occluded filter. The
guide wire was pushed forwards and rotated when its tip met
resistance from the thrombus. In acutely IVC thrombotic patients,
the guide wire easily entered the thrombus. In subacute patients,
the guide wire entered the thrombus with assistance from the
catheter. The catheter then entered the thrombus over the guide
wire. This process was repeated until the catheter tip entered the
distal vein lumen without thrombus. A venogram was performed to
ensure the extent of the thrombus and collateral veins. Then, a
thrombolytic catheter (UniFuse; AngioDynamics, Queensbury, NY, USA)
with a 20 or 30 cm-length side-hole was placed into the thrombus.
500,000 IU urokinase was infused for 2 h twice every day through
the thrombolytic catheter. Systemic anticoagulant therapy was
administered by intravenously injecting 50 IU/kg heparin every 6 h.
A cavogram and lower extremity venogram were performed every 3–4
days during thrombolysis therapy. The location of thrombolytic
catheter was adjusted according to the extent of the residual
thrombus.
Filter retrieval
When the symptoms of the bilateral lower extremities
were partly or completely relieved, and no or minimal residual
thrombus remained in the IVC and bilateral iliofemoral veins, the
thrombolytic therapy was terminated and the IVC filter was
retrieved within a limited period.
Through the right jugular vein approach for
retrieval of the GTF, a 5-Fr pig-tail catheter was placed into the
IVC above the bifurcation. An anteroposterior cavogram was
performed to ensure the tilt angle of the GTF and the relationship
between the apical retrieval hook and the IVC wall, and to ensure
that the filter was free of thrombus or had captured <8 mm
thrombus. A 12-Fr sheath was then inserted into the IVC near the
filter. A 15-mm goose-neck snare (Amplatz Goose Neck; ev3 Inc.,
Plymouth, MN, USA) was passed through the sheath. The retrieval
hook of the filter was engaged with the snare, the snare was closed
and the filter was sheathed.
Through the femoral vein approach for retrieval of
the OptEase filter, a pig-tail catheter was placed into the iliac
vein. After ensuring that the filter was free of thrombus or had
captured <8 mm thrombus by an anteroposterior cavogram, a 12-Fr
sheath was inserted into the IVC near the filter. The snare was
passed through the sheath. The retrieval hook of the filter was
engaged with the snare and the filter was sheathed. If repeated
attempts, including operations performed under the Valsalva
maneuver, did not engage the retrieval hook, it was necessary to
use a catheter-directed technique. In the catheter-directed
technique, the snare trapped the head end of a 5-Fr curved
catheter. The catheter was then pushed forward. When the curved
portion of the catheter entered the filter cone, the catheter was
rotated and twisted with the strut of the filter cone. The snare
was loosened slightly and pushed slowly along the catheter under
the Valsalva maneuver. When the snare had trapped the filter cone,
the catheter was drawn back. The snare then encircled the retrieval
hook, the sheath was pushed forward and the filter was
sheathed.
When the filter was enclosed by the sheath, the
filter was retracted and removed. A repeat cavogram and pulmonary
arteriogram were obtained following retrieval to inspect for
complications. The technical and clinical outcome, complications
and postoperative PE were monitored. All patients accepted
long-term anticoagulation treatment by oral warfarin following the
retrieval procedure. The patients were examined by vascular
ultrasound 6 months after the surgery.
Results
Five retrievable filters, including 4 GTFs and 1
OptEase filter, were successfully implanted in 5 patients. The
median duration of the filter implantation surgery was 2.0 min
(range, 1–3 min). Technically and clinically successful
recanalization and thrombolysis were achieved in 5 of 5 patients
and 10 of 10 symptomatic limbs. In 4 patients, the residual
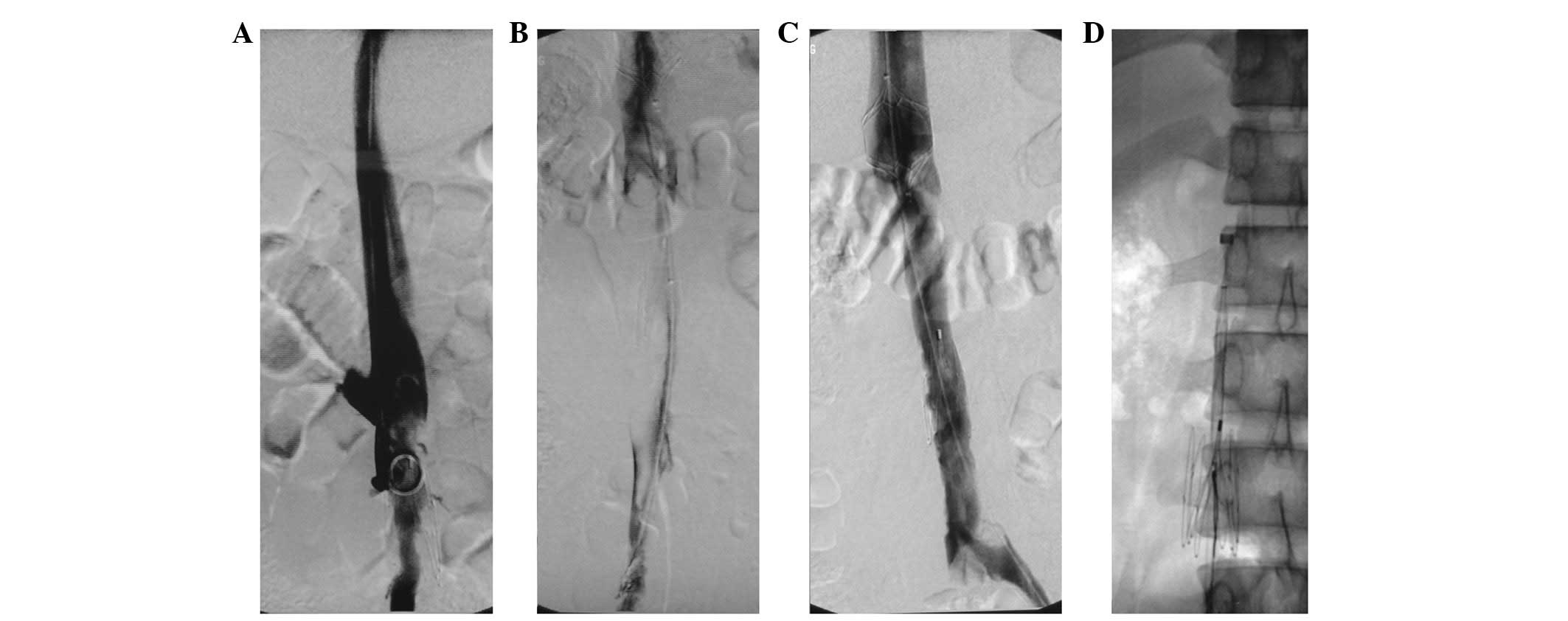
thrombus in the IVC was <10% (Fig.
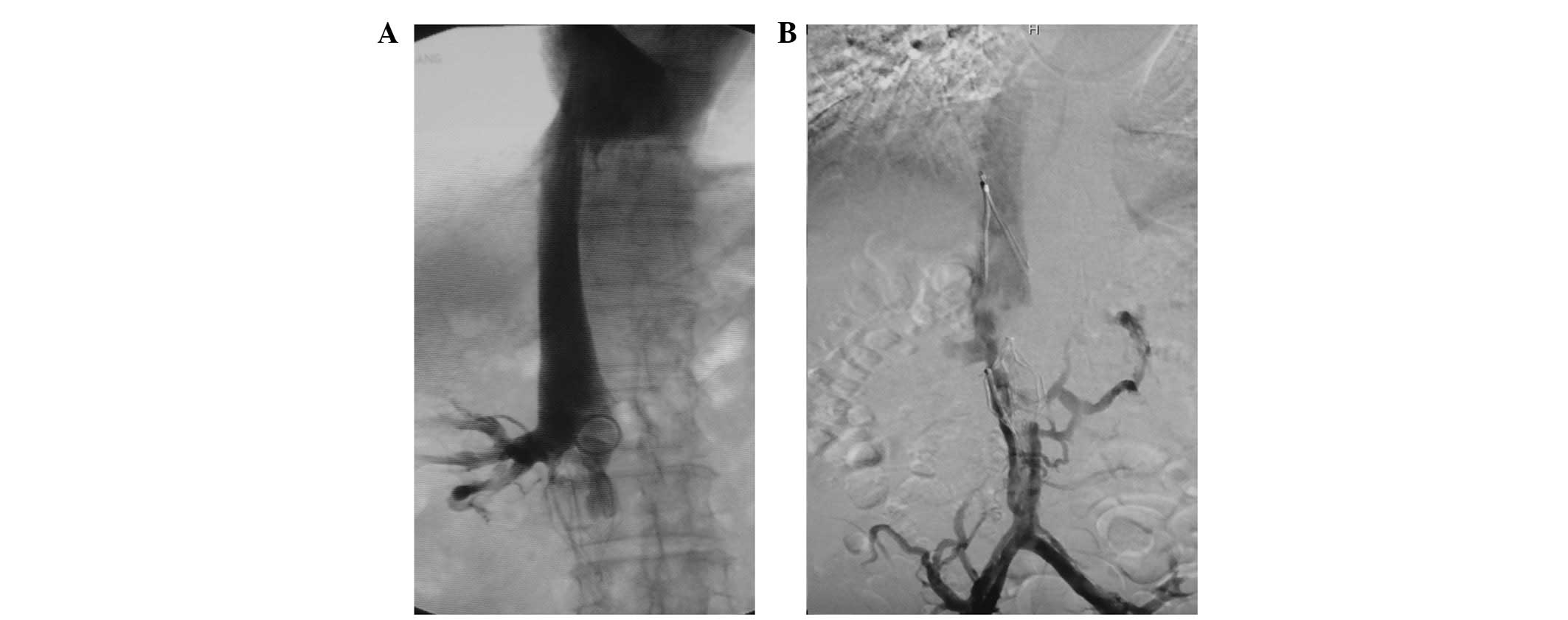
1). The residual thrombus in the IVC was >50% in one patient
(Fig. 2). The median duration of
the IVC recanalization surgery was 5 min (range, 3–15 min). The
median thrombolysis period was 13 days (range, 8–14 days). No major
bleeding occurred during the study.
Six retrievable filters, including GTF (n=4) and
OptEase filters (n=2), were finally retrieved, a success rate of
100% (6/6). In case 2, the OptEase filter in the thrombus was
successfully retrieved using the catheter-directed technique when
the thrombolytic therapy had been administered for 4 days and the
residual thrombus in the IVC and OptEase filter was still large.
The median dwell time for the filters that were removed was 50.5
days (range, 14–73 days). The median duration of the fluoroscopic
retrieval surgery was 5.5 min (range, 2–26 min). No
procedure-related complications occurred. During clinical
follow-up, no clinically detectable PE or lower extremity swelling
were observed. The type of second filter, dose of urokinase, course
of transcatheter thrombolysis, IVC thrombus residue rate and dwell
time of the retrieved filter for each patient are recorded in
Table II.
 | Table II.Interventional therapy of the
patients. |
Table II.
Interventional therapy of the
patients.
| Case no. | First filter | Second filter | Dose of urokinase
(U/bid) | Course of treatment
(days) | IVC thrombus residue
(%) | Dwell time
(days) |
|---|
| 1 | Vena Tech | OptEase | 500,000 | 14 | <10 | 14 |
| 2 | OptEase | Tulip | 500,000 | 8 | <10 | 52 (14)a |
| 3 | Vena Tech | Tulip | 500,000 | 11 | <10 | 49 |
| 4 | OptEase | Tulip | 500,000 | 14 | >50 | 73 |
| 5 | OptEase | Tulip | 500,000 | 13 | <10 | 62 |
Discussion
Complications of inferior vena cava filters include
thrombosis of the IVC, caval occlusion, recurrent DVT, recurrent
pulmonary embolus, filter migration, caval and aortic perforation
and struts fracture (15,16). Thrombosis of the IVC is a
potentially catastrophic complication of caval filter placement,
and its reported incidence ranges from 0.8 to 25%, depending on
filter type, indication of filter implantation and anticoagulant
therapy (5,17–21).
Due to the draining of lateral veins, some patients with thrombosis
of the IVC following filter implantation may not suffer symptoms
such as swelling and pain in both lower extremities and the rate of
thrombosis of the IVC following filter implantation may be
significantly higher than that of symptomatic IVC thrombosis. A
comparative analysis revealed that there was a significantly higher
incidence of symptomatic IVC thrombosis with the use of the Bird’s
Nest filters (14.6%) compared with the stainless steel Greenfield
filters (0%), titanium Greenfield filters with a modified hook
(3.6%) or Vena Tech filters (4%; P<0.05) (17). In a clinical study of 400 cases,
Nazzal et al reported that in the group of patients who had
hypercoagulable conditions, the incidence of IVC thrombosis was
higher with TrapEase filters compared with all other filters as a
group (P<0.05) (21). Crochet
et al(22) studied 142
patients with implanted Vena Tech filters and found a caval patency
rate of 80% at a 9-year follow-up. Patients who received filters
due to anticoagulation failure had a significantly higher (P=0.016)
rate of filter occlusion (64.8%) (22). Tardy et al(5) reported that in 30 consecutive cases
with symptomatic IVC filter thrombosis, 25 patients did not receive
anticoagulant at the time of the diagnosis and none of the other
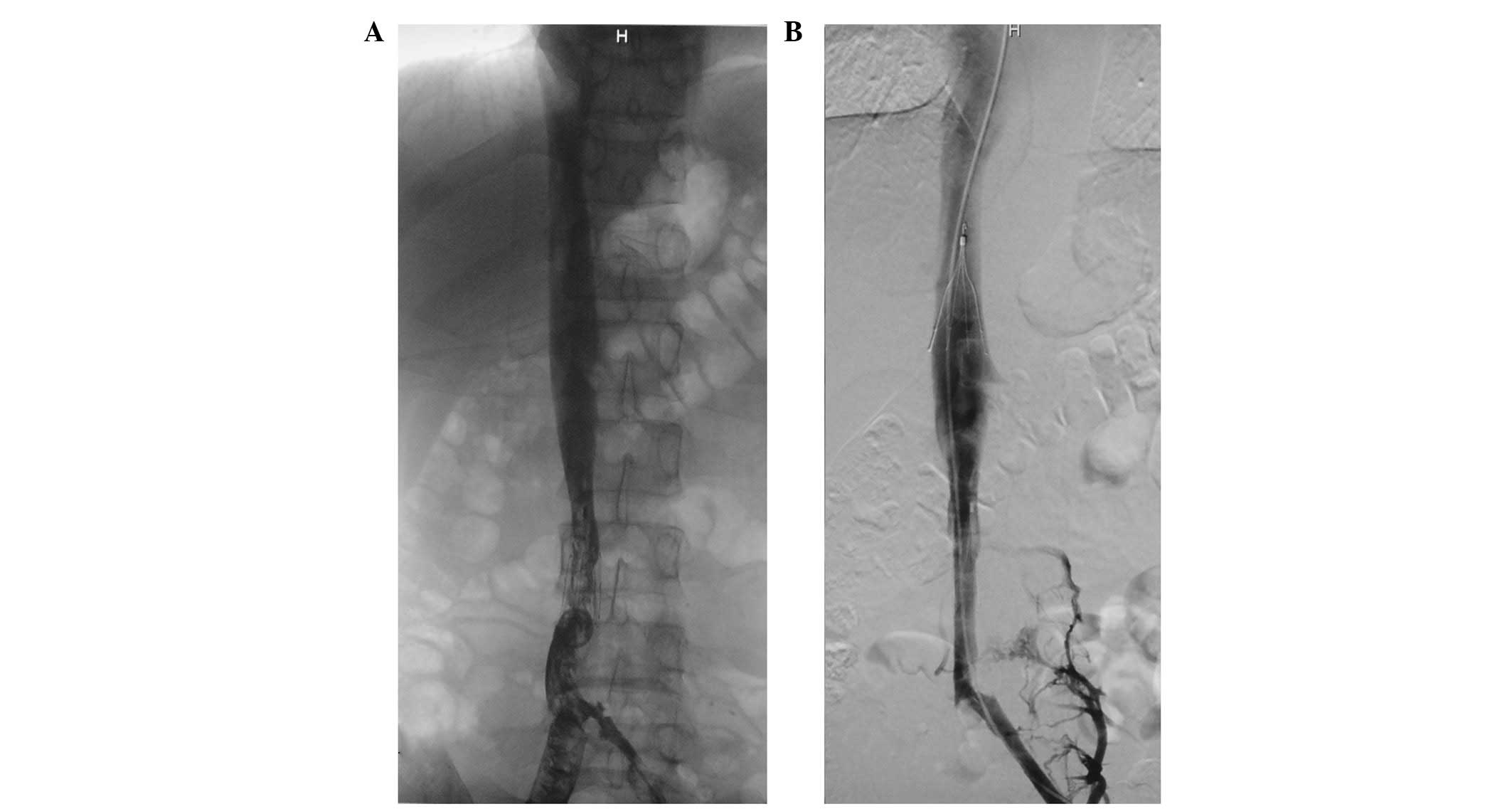
five received adjusted anticoagulation. In the current study, 5
patients suffered symptomatic IVC thrombosis with the use of Vena
Tech filters (n=2; Fig. 3) and
OptEase filters (n=3). In cases 1 and 2, the anticoagulant therapy
following filter implantation was inadequate, the symptoms worsened
gradually, and the patients were referred to our hospital after
being diagnosed with IVC thrombosis. In cases 3–5, the patients
were free from clinical symptoms during the anticoagulant therapy
and the swelling of lower extremities emerged 1 year, 3 months and
4 months after the cessation of anticoagulant therapy,
respectively. The mechanisms of thrombosis of the IVC following
filter implantation remain obscure. The authors consider that it is
related to the hemodynamic changes in the IVC following filter
implantation, captured thrombus in the filter and local thrombosis
at the site where the filter struts contact the IVC wall due to the
stimulus of the filter’s radial force, and anticoagulant therapy
after filter implantation may reduce the extent of thrombosis in
these conditions. In addition, filter retrieval when the risk of PE
has decreased may be a prophylactic method for IVC thrombosis.
The therapeutic methods for symptomatic IVC
thrombosis following filter implantation include anticoagulant
therapy, systemic thrombolysis, catheter-directed thrombolysis,
mechanical thrombectomy, balloon dilation, stent placement and
filter retrieval (5,7,23–31).
Anticoagulation therapy is largely ineffective in
relieving the symptoms of thrombosed IVC in the lower extremities
(32). Thrombolytic therapy is of
value in acute thrombosis. Bihorac and Kitchens reported that
systemic thrombolytic therapy successfully treated acute kidney
injury secondary to thrombosis of a suprarenal IVC filter (23). Infusion of tissue plasminogen
activator (tPA) through a thrombolytic catheter has successfully
treated a patient with bilateral renal vein thrombosis due to IVC
filter migration and thrombosis (7). Angle et al reported that
thrombolysis for symptomatic IVC thrombosis was successful in 7 of
8 (88%) patients with no or minimal residual thrombus using local
catheter-directed infusion of urokinase and the 7 patients had no
lower extremity swelling after the procedure (24). In the current study, after infusion
of urokinase through a thrombolytic catheter, the residual thrombus
in the IVC was <10% in 4 of 5 patients with a thrombo-occlusive
IVC filter, the blood flow in the IVC was recovered in all 5
patients, and swelling of the lower extremity disappeared or was
relieved in all 10 limbs.
Bleeding is a severe complication of thrombolytic
therapy. Patients who have an anticoagulant contraindication or a
bleeding tendency are not suitable for treatment with thrombolytic
drugs. Under such conditions, percutaneous mechanical thrombectomy
has been used as an alternative therapy which may result in rapid
symptomatic relief (25). In
addition, combined catheter-directed thrombolysis and mechanical
thrombectomy may shorten the course of treatment and decrease the
dose of thrombolytic agent for acute IVC thrombosis (26).
Treatment with suction thrombectomy and thrombolysis
is usually ineffective for chronic thrombosis. To maintain the
fluency of the IVC, balloon dilation and stent implantation have
been performed following the recanalization of chronic IVC
thrombosis. Joshi et al reported that following
thrombolysis, thrombectomy and percutaneous removal of the filter
did not succeed and an expandable metallic Gianturco Z stent (Cook,
Bloomington, IN, USA) was used to extract the TrapEase filter from
the vessel lumen (27). In 25
patients with an obstructed IVC filter, following recanalization by
a guide wire and balloon dilation, the filter was markedly
displaced sidewise or remodeled (28). Following the implantation of a
stent across the filter and re-dilation, the lumen of the IVC was
recovered. Stenting maneuvers through a previous IVC filter have
been safely performed with no tearing of the IVC, no clinical
bleeding or abdominal symptoms and no pulmonary embolism (28–30).
Retrieval of a thrombo-occlusive IVC filter may not
only remove a thrombosis-evoking factor, but also help to increase
the efficacy of other therapies for previous thrombus. The
retrieval surgeries of thrombotic IVC filters are usually
complicated and time-consuming. In a clinical study, Kuo et
al reported the experience of filter retrieval for treating
symptomatic filter-related IVC stenosis and thrombotic
complications (31). In the
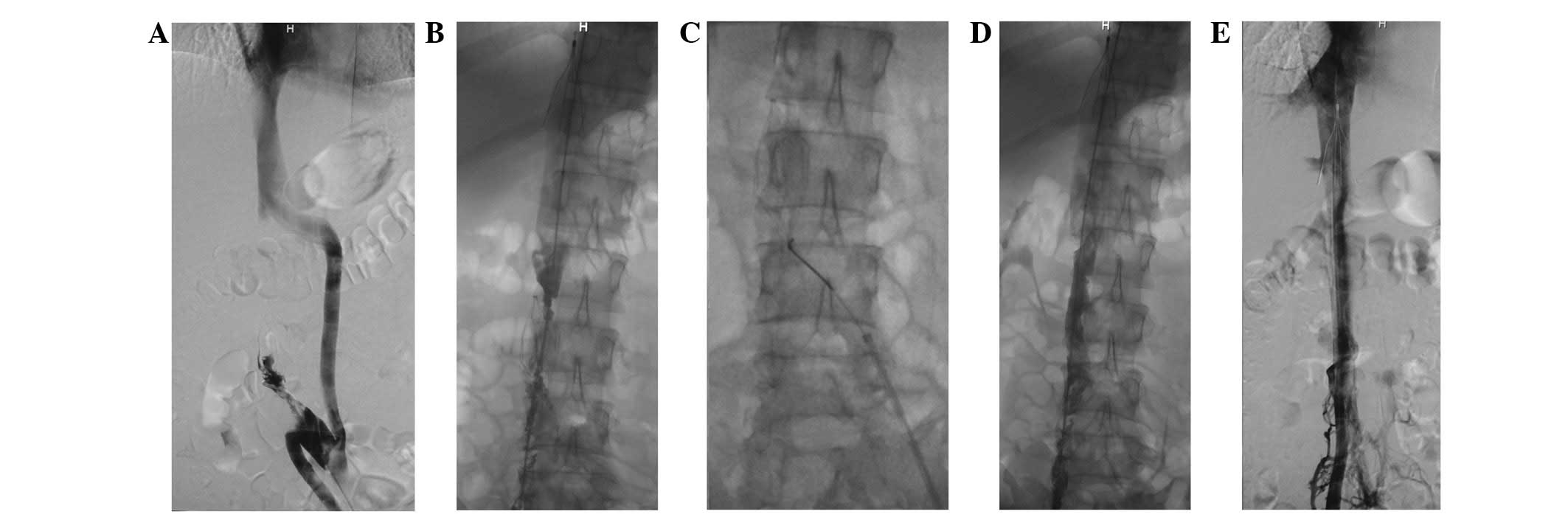
current study, an OptEase filter with inner thrombosis was
successfully retrieved during transcatheter thrombolytic therapy.
The thrombolytic therapy was continued for another 4 days until the
residual thrombus in the IVC and iliofemoral veins was <10%
(Fig. 4). The course of
thrombolytic therapy in this patient was the shortest in our
study.
Endovascular recanalization and transcatheter
thrombolysis of IVC thrombosis are efficient, feasible and safe,
even in the presence of an IVC filter. The prompt diagnosis and
interventional therapy are likely to improve the prognosis of
symptomatic IVC thrombosis following filter implantation.
Acknowledgements
This study was supported by research
grants from the Scientific Research Fund of Liaoning Science and
Technology Agency, China (No. 2008225010-5), the Scientific
Research Fund of Liaoning Education Agency, China (No. 2007T183)
and the Scientific Research Fund of First Hospital of CMU (No.
FSFH1006).
References
|
1.
|
Kinney TB: Update on inferior vena cava
filters. J Vasc Interv Radiol. 14:425–440. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Berczi V, Bottomley JR, Thomas SM, Taneja
S, Gaines PA and Cleveland TJ: Long-term retrievability of IVC
filters: should we abandon permanent devices? Cardiovasc Intervent
Radiol. 30:820–827. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
PREPIC Study Group: Eight-year follow-up
of patients with permanent vena cava filters in the prevention of
pulmonary embolism: the PREPIC (Prevention du Risque d’Embolie
Pulmonaire par Interruption Cave) randomized study. Circulation.
112:416–422. 2005.
|
|
4.
|
Hajduk B, Tomkowski WZ, Malek G and
Davidson BL: Vena cava filter occlusion and venous thromboembolism
risk in persistently anticoagulated patients: a prospective,
observational cohort study. Chest. 137:877–882. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Tardy B, Mismetti P, Page Y, et al:
Symptomatic inferior vena cava filter thrombosis: clinical study of
30 consecutive cases. Eur Respir J. 9:2012–2016. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Marcy PY, Magné N, Frenay M and Bruneton
JN: Renal failure secondary to thrombotic complications of
suprarenal inferior vena cava filter in cancer patients. Cardiovasc
Intervent Radiol. 24:257–259. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Janvier AL, Hamdan H and Malas M:
Bilateral renal vein thrombosis and subsequent acute renal failure
due to IVC filter migration and thrombosis. Clin Nephrol.
73:408–412. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Senitko M, Sims R, Dolmatch B, Vazquez MA
and Lu CY: Inferior vena cava (IVC) filter thrombosis in a renal
transplant recipient. Clin Nephrol. 71:456–459. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Gloviczki P, Pairolero PC, Toomey BJ, et
al: Reconstruction of large veins for nonmalignant venous occlusive
disease. J Vasc Surg. 16:750–761. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Mewissen MW, Seabrook GR, Meissner MH,
Cynamon J, Labropoulos N and Haughton SH: Catheter-directed
thrombolysis for lower extremity deep venous thrombosis: report of
a national multicenter registry. Radiology. 211:39–49. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Grossman C and McPherson S: Safety and
efficacy of catheter-directed thrombolysis for iliofemoral venous
thrombosis. AJR Am J Roentgenol. 172:667–672. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Castaneda F, Li R, Young K, Swischuk JL,
Smouse B and Brady T: Catheter-directed thrombolysis in deep vein
thrombosis with use of reteplase: immediate results and
complications from a pilot study. J Vasc Interv Radiol. 13:577–580.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Comerota AJ, Throm RC, Mathias SD,
Haughton S and Mewissen M: Catheter-directed thrombolysis for
iliofemoral deep venous thrombosis improves health-related quality
of life. J Vasc Surg. 32:130–137. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Verhaeghe R, Stockx L, Lacroix H, Vermylen
J and Baert AL: Catheter-directed lysis of iliofemoral vein
thrombosis with use of rt-PA. Eur Radiol. 7:996–1001. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Joels CS, Sing RF and Heniford BT:
Complications of inferior vena cava filters. Am Surg. 69:654–659.
2003.PubMed/NCBI
|
|
16.
|
Maleux G, Heye S, Verhamme P, Vaninbroukx
J and Delcroix M: Penetration of a fractured Bird’s Nest filter
strut into the liver parenchyma: report of two cases. Acta Radiol.
52:643–645. 2011.PubMed/NCBI
|
|
17.
|
Mohan CR, Hoballah JJ, Sharp WJ, Kresowik
TF, Lu CT and Corson JD: Comparative efficacy and complications of
vena caval filters. J Vasc Surg. 21:235–245. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Linsenmaier U, Rieger J, Schenk F, Rock C,
Mangel E and Pfeifer KJ: Indications, management, and complications
of temporary inferior vena cava filters. Cardiovasc Intervent
Radiol. 21:464–469. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Ahmad I, Yeddula K, Wicky S and Kalva SP:
Clinical sequelae of thrombus in an inferior vena cava filter.
Cardiovasc Intervent Radiol. 33:285–289. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Ziegler JW, Dietrich GJ, Cohen SA,
Sterling K, Duncan J and Samotowka M: PROOF trial: protection from
pulmonary embolism with the OptEase filter. J Vasc Interv Radiol.
19:1165–1170. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Nazzal M, Chan E, Nazzal M, et al:
Complications related to inferior vena cava filters: a
single-center experience. Ann Vasc Surg. 24:480–486. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Crochet DP, Brunel P, Trogrlic S,
Grossetëte R, Auget JL and Dary C: Long-term follow-up of Vena
Tech-LGM filter: predictors and frequency of caval occlusion. J
Vasc Interv Radiol. 10:137–142. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Bihorac A and Kitchens CS: Successful
thrombolytic therapy for acute kidney injury secondary to
thrombosis of suprarenal inferior vena cava filter. J Thromb
Thrombolysis. 28:500–505. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Angle JF, Matsumoto AH, Al Shammari M,
Hagspiel KD, Spinosa DJ and Humphries JE: Transcatheter regional
urokinase therapy in the management of inferior vena cava
thrombosis. J Vasc Interv Radiol. 9:917–925. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Poon WL, Luk SH, Yam KY and Lee AC:
Mechanical thrombectomy in inferior vena cava thrombosis after
caval filter placement: a report of three cases. Cardiovasc
Intervent Radiol. 25:440–443. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Yan BP, Kiernan TJ, Gupta V, Ajani AE and
Schainfeld RM: Combined pharmacomechanical thrombectomy for acute
inferior vena cava filter thrombosis. Cardiovasc Revasc Med.
9:36–40. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
27.
|
Joshi A, Carr J, Chrisman H, et al:
Filter-related, thrombotic occlusion of the inferior vena cava
treated with a Gianturco stent. J Vasc Interv Radiol. 14:381–385.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
28.
|
Neglén P, Oglesbee M, Olivier J and Raju
S: Stenting of chronically obstructed inferior vena cava filters. J
Vasc Surg. 54:153–161. 2011.PubMed/NCBI
|
|
29.
|
Golarz SR and Grimsley B: Use of Wall
stent to exclude a thrombosed inferior vena cava filter. Ann Vasc
Surg. 24:690.e5–e7. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
30.
|
Vedantham S, Vesely TM, Parti N, et al:
Endovascular recanalization of the thrombosed filter-bearing
inferior vena cava. J Vasc Interv Radiol. 14:893–903. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
31.
|
Kuo WT, Tong RT, Hwang GL, et al:
High-risk retrieval of adherent and chronically implanted IVC
filters: techniques for removal and management of thrombotic
complications. J Vasc Interv Radiol. 20:1548–1556. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
32.
|
Razavi MK, Hansch EC, Kee ST, Sze DY,
Semba CP and Dake MD: Chronically occluded inferior venae cavae:
endovascular treatment. Radiology. 214:133–138. 2000. View Article : Google Scholar : PubMed/NCBI
|