Introduction
Glaucoma optic nerve (ON) damage, optic neuritis and
other ophthalmic neurodegenerative diseases are the leading causes
of legally defined blindness in adults. The number of patients with
ophthalmic neurodegenerative diseases increases annually (1). Axonal degeneration is an active
neurodegeneration process, which eventually leads to permanent
vision loss. Wallerian axon degeneration, as observed in numerous
neurodegenerative diseases, is a commonly used model for studying
axonal degeneration (2–4). It is caused by various fracture
traumas. Broken-end distal axons are only able to live for a few
days due to somatic nutritional support. The axon then quickly
denatures and disintegrates. The debris is engulfed by Schwann
cells and macrophages (4).
Wallerian degeneration may be observed in the central nervous
system (CNS) and peripheral nervous system. How it is initiated is
not fully understood and the underlying molecular mechanisms remain
largely unknown (2,3).
The degeneration of transected axons is
significantly delayed in the Wallerian degeneration slow
(Wlds) mouse strain. The phenotype is mainly due
to the overexpression of a chimeric protein,
Wlds(4).
Wlds is composed of a short fragment of the
E4-ubiquitin ligase Ube4b (yeast Ufd2) and a
full-length nicotinamide mononucleotide
adenylyl-transferase-1 (Nmnat-1) (5,6). The
underlying molecular mechanisms of the protective effects of the
Wlds gene or its product on the axon are not
clear, although hypotheses involving overexpression of dominant
negative ubiquitin proteins and Nmnat1-induced biosynthesis
of nicotinamide adenine dinucleotide (NAD) have been proposed
(7).
At present, studies on Wlds mice
have been focused on the molecular mechanisms of its effect on the
delayed peripheral nerve axonal degeneration. However, few studies
have focused on the effects of Wlds on retinal
ganglion cell (RGC) body degeneration. In the present study, the
Wlds gene was observed to not only delay the
degeneration of axons, but also protect RGC bodies in a Wallerian
axon degeneration model.
Materials and methods
Mouse ON surgery
The mouse ON crush injury was performed unilaterally
under deep anaesthesia with intraperitoneal ketamine (10% urethane,
5% chloral hydrate; 30mg/kg). With the aid of an operating
microscope, the superior conjunctiva was incised with spring
scissors and, following blunt dissection, the carefully exposed ON
was crushed for 20 sec with calibrated forceps (type 3C; Dumont,
Montignez, Switzerland), 2–3 mm behind the globe. The eye on which
surgery was performed was covered with ofloxacin ointment (external
application). All the animal experiments undertaken in the present
study were approved by the Nanjing Medical University Animal
Committee.
Electroretinograms (ERGs)
As previously reported (8), ERGs were used to monitor the overall
retinal function prior to and at various time points following
surgery. The wild-type (WT) and Wlds mice were
prepared under dim red illumination. Animals were injected
intraperitoneally with a compound anesthetic (dihydroetorphine
hydrochloride, haloperidol; 0.5 ml/kg) and the pupils were dilated
with 0.1% tropicamide. During the recording session, the mice were
placed on a heating plate to maintain body temperature at 37°C.
ERGs were recorded with an Ag-AgCl electrode placed in contact with
the cornea limbus; a reference electrode was inserted in the cheek
and a ground electrode was placed in the tail. The cornea was kept
moist with carboxymethyl cellulose sodium. The reference and ground
electrodes were stainless steel needles inserted under the skin of
the scalp and tail, respectively. A small drop of balanced salt
solution (Alcon, Fort Worth, TX, USA) was topically applied to the
cornea to prevent dehydration for the duration of the recording. A
visual stimulus of contrast-reversing horizontal bars (field area,
50x58°; mean luminance, 50 cd/m2; spatial frequency,
0.05 cyc/deg; contrast, 98%; temporal frequency, 1 Hz) was aligned
with a projection of the pupil at the viewing distance of 15 cm.
The eyes were not refracted for the viewing distance given that the
mouse eye has a large depth of focus due to the pinhole pupil.
Retinal signals were amplified (10,000-fold) and the
band-pass filtered (1–30 Hz). Three consecutive responses to each
of 600 contrast reversals were recorded. The responses were
superimposed to check for consistency and then averaged (1,800
sweeps). The peak ERG (PERG) is a light-adapted response.
PERGs consisting of a major positive wave followed by a slower
negative wave were automatically analyzed to evaluate the response
amplitude which was defined as the sum of the absolute values of
the maximum and minimum voltages (peak-to-trough
amplitude).
Visual evoked potentials (VEPs)
The mice were anesthetized with ketamine (75 mg/kg)
and xylazine (10 mg/kg). A normal body temperature was maintained
using a surrounding hot water bag and the corneas were kept moist
with saline or 2.5% hydroxypropyl methylcellulose (Johnson &
Johnson, Shanghai, China). Stainless steel needle electrodes, 7 mm
in length, were placed subdermally in the occipital midline
(active) and the pinna. A subdermal needle electrode in the midline
near the tail served as the ground electrode. The signals were
amplified by 10,000-fold, filtered from 1–1000 Hz and were
digitized and recorded by a Nicolet 4094 digital oscilloscope
(Nicolet Instruments Technology Inc., Madison, WI, USA) set for
averaging (0.396 sec trace duration, digitization rate =
10,000/sec). No artifact rejection was used. During the recording
of the VEPs, the ambient illuminance was dim (2.9 lx) as measured
at the eye. The surrounding luminance was 0.3–0.6 lx. The
mice were placed prone, facing a Grass PS22 flash lamp diffusing
faceplate (Grass Instruments Co., Quincy, MA, USA) at a distance of
20 cm. The mice were stimulated binocularly at 1 flash/sec. The
flash illuminance at the eyes was 88 μsec and flash duration
was 10 μsec. A total of 120 traces synchronized with flash
onset were averaged to produce one VEP. Four VEPs were recorded
from each mouse. Noise controls were produced in the same manner
but with the flash occluded by a black opaque cloth. The digitized
waveforms were saved as ASCII files with Vu-Point II
(Maxwell Laboratories Inc., La Jolla, CA, USA).
Retinal histopathology evaluation after
ON surgery
As previously reported (8), at the completion of the ERGs, the
mice were sacrificed by cervical dislocation. The two eyes were
enucleated and fixed in Feteke's solution for 2 h, followed by a
12-h fixation in 4% paraformaldehyde. After dehydration in a graded
ethanol series, the eyes were embedded in paraffin. Sections (5
μm in thickness) were cut along the vertical meridian at
0.05 mm intervals, yielding 18 sections from each eye, and stained
with hematoxylin and eosin (HE) to evaluate the retinal histology.
The presence of inflammatory cell infiltration was assessed with a
4-point scale. No infiltration, 0; mild cellular
infiltration of the ON or ON sheath, 1; moderate infiltration, 2;
severe infiltration, 3; massive infiltration, 4.
Luxol Fast Blue (LFB) staining
Sections were cut from the paraffin-embedded
tissue. The slides were placed in LFB solution overnight at 55°C,
differentiated in alcohol, dipped in 0.05% lithium carbonate
solution and then counterstained with cresyl violet.
Terminal deoxynucleotidyl transferase
(TdT)-mediated dUTP nick end labeling (TUNEL) staining
A TUNEL assay was used to evaluate the apoptosis of
retinal cells following ON injury. The eyes were enucleated 1, 2
and 3 weeks after surgery and the retinas were dissected as
described previously. The tissue was then fixed with 10%
formaldehyde for 24 h. The whole retina was divided into two parts
through the optic disc and then dehydrated and embedded in
paraffin. Sagittal sections (5 mm in thickness) were cut through
the optic disc and mounted. The deparaffinized sections were
treated with the In Situ Cell Death Detection kit (Roche
Molecular Biochemicals, Indianapolis, IN, USA), which is based on
the binding of digoxigenin-dUTP to the 3′-OH end of
DNA by TdT followed by incubation with an anti-digoxigenin
antibody conjugated to peroxidase. The sections were examined under
x40 magnification. Six microscopic fields of each eye with three
adjacent areas on each side of the ON head (1 mm from the ON head)
were used to count the TUNEL-positive cells in the ganglion
cell layer (GCL). The average number of TUNEL-positive cells
in these layers per field was used for analysis.
Electron microscopy
Nerve segments 3 and 15–20 mm distal to the
ON transection lesion were immersion fixed with 2.5% glutaraldehyde
and 2% paraformaldehyde in 0.1 M cacodylate buffer for 5–14
days at 4°C. Subsequently the segments were extensively washed in
0.1 M cacodylate buffer, post-fixed in 4% aqueous
OsO4 and 1% uranyl acetate and then dehydrated in graded
ethanol and propylene oxide. Final resin embedding was performed
using Durcupan (Fluka Chemie, Buchs, Switzerland). After
polymerization for 48 h at 60°C, 50–100 nm transverse
sections were cut on a Leica ultramicrotome, mounted on
formvar-coated copper grids, counterstained with uranyl acetate and
lead citrate and examined with a Zeiss EM 902 transmission electron
microscope.
Statistical analysis
All data are expressed as mean ± SEM. When comparing
data from the WT with Wlds mice, P<0.05 was
considered to indicate statistically significant differences using
one-way analysis of variance (ANOVA) with time or genotype as the
independent factor. When ANOVA showed significant differences,
pairwise comparisons between the means were tested by Bonferroni
post-hoc testing (GraphPad Prism 4.0).
Results
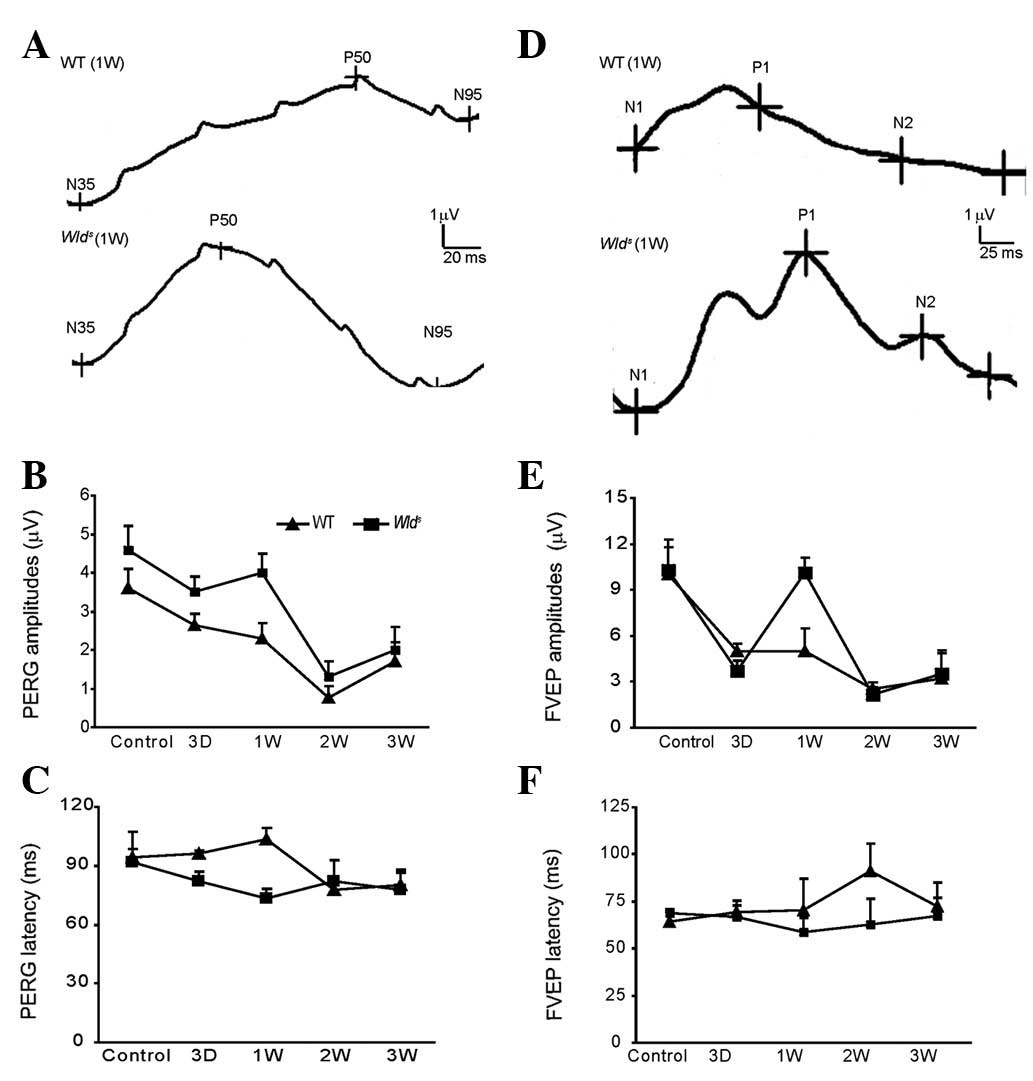
Electrophysiology
The electrophysiological properties of retina RGCs
were examined first (Fig. 1A). No
significant differences in the eye PERG amplitude and mean PERG
latency were observed between the WT and Wlds
mice prior to ON surgery. However, one week after ON surgery, the
eye PERG was significantly higher in the Wlds
mice (P<0.05 vs. WT) and PERG latency was also higher (P<0.05
vs. WT; Fig. 1A and B). The mean
eye PERG latency was 70±3 msec in WT and 100±3 msec in
Wlds mice (Fig.
1C; P<0.05). However, two weeks after ON surgery, no
significant differences were observed between the WT and
Wlds mice (Fig. 1A
and C; P>0.05).
VEP
Reprehensive VEPs for the WT and
Wlds mice before and after ON surgery are shown
in Fig. 1D. The amplitude was
10±0.3 μV for the WT and Wlds mice prior
to ON surgery (Fig. 1E). However,
a significant difference in VEPs was observed one week after ON
surgery. The mean VEPs amplitude was 5.0±0.5μV for the WT
mice and 10±0.5 μV for the Wlds mice
(Fig. 1E; P<0.05). Significant
PERG latency differences were also observed two weeks after ON
surgery (P<0.05; Fig. 1F).
These results indicate that the Wlds gene
protects the ON from axonal degeneration in Wlds
mice.
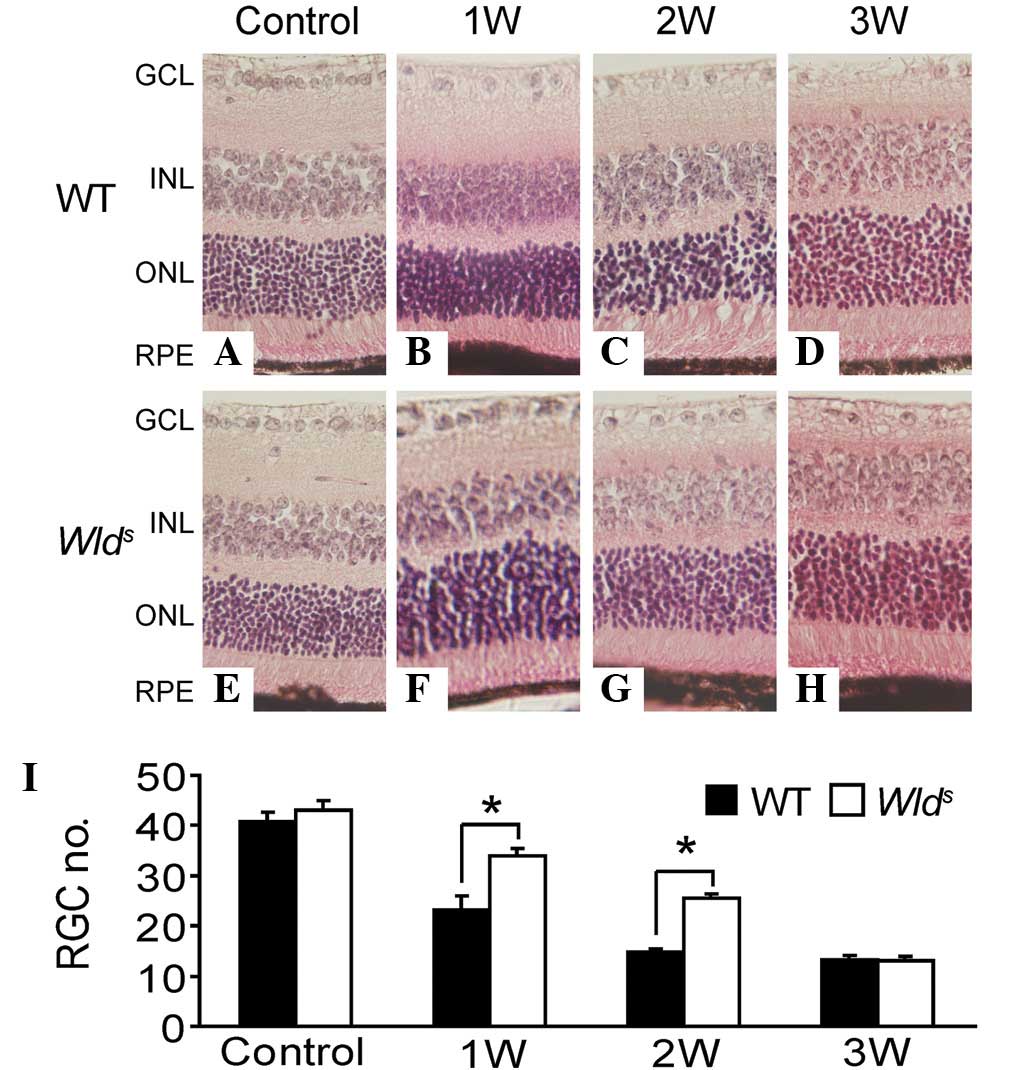
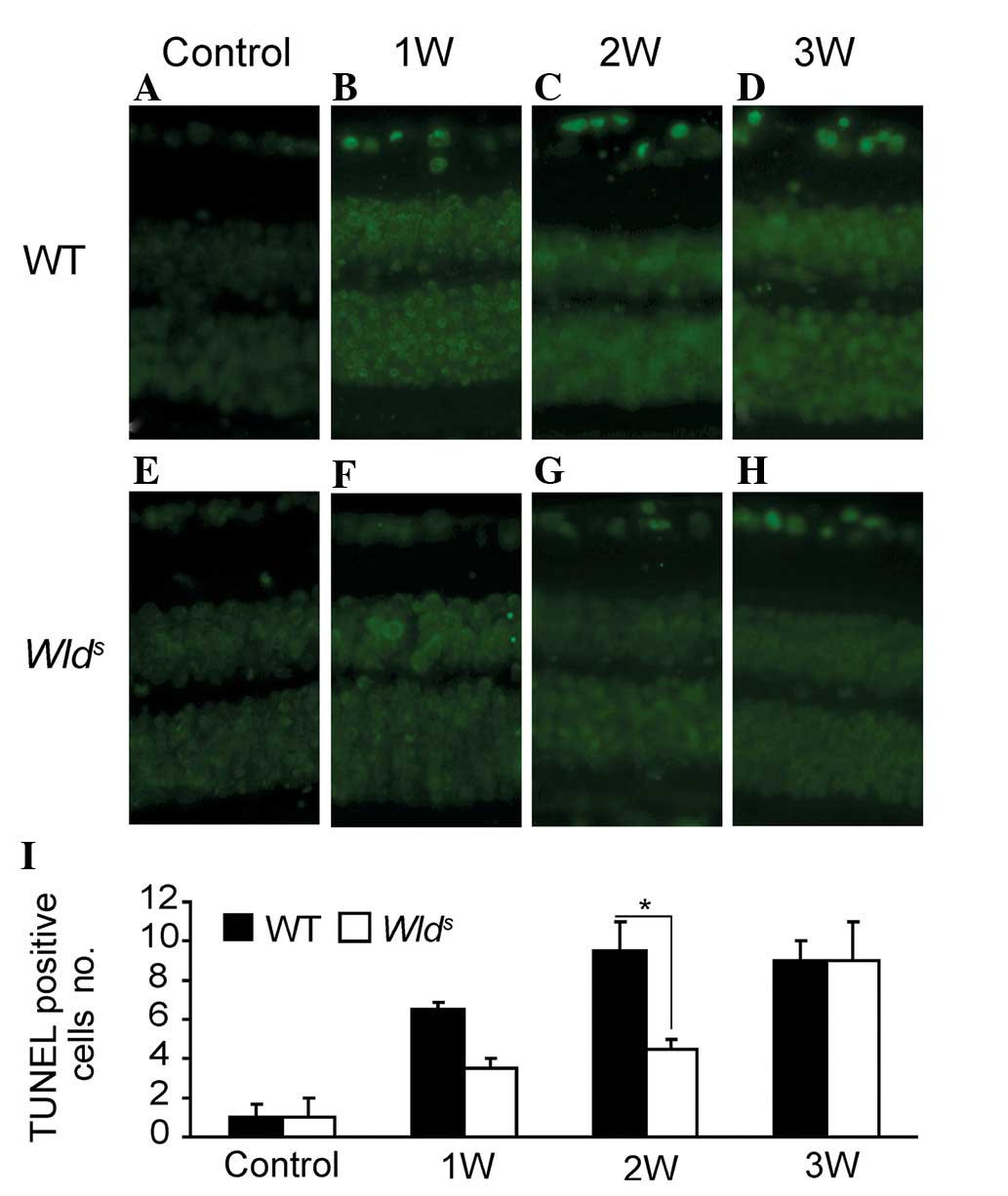
HE and TUNEL
Prior to ON surgery, no significant difference was
observed the number of RGCs between the WT and
Wlds mice (Fig.
2I). One week after ON surgery, a local collapse of RGC cells
was observed in the WT mice, as the number of RGCs declined
significantly (Fig. 2I). By
contrast, the number of RGC cells in the Wlds
mice was close to that prior to surgery (Fig. 2F). Morphological observations
further confirmed the results (Fig.
2A–H). Three weeks after ON surgery, the retina exhibited a
marked loss of RGC in both the WT and Wlds mice
(Fig. 2), with >65% of retinal
pigment epithelial (RPE) cells lost in the two mouse lines
(Fig. 2I). The RGC loss following
the surgery appeared to result from apoptotic cell death, as
increases in the number of TUNEL-positive RGC cells (a marker of
cell apoptosis) were detected in the WT (at any stage) and
Wlds mice (late stages; Fig. 3). Sections of whole eyes from the
WT or Wlds mice were removed one, two and three
weeks after surgery. TUNEL labeling was performed to stain cells
undergoing active apoptosis. Few TUNEL-positive cells were observed
within the RGC cell layer after one week in the
Wlds mice (Fig.
3A–D), whereas a significant number of TUNEL-positive cells
were present in the GCL of the WT mice (Fig. 3E–H). Three weeks after surgery, the
two mouse lines showed a significant number of TUNEL-positive
cells.
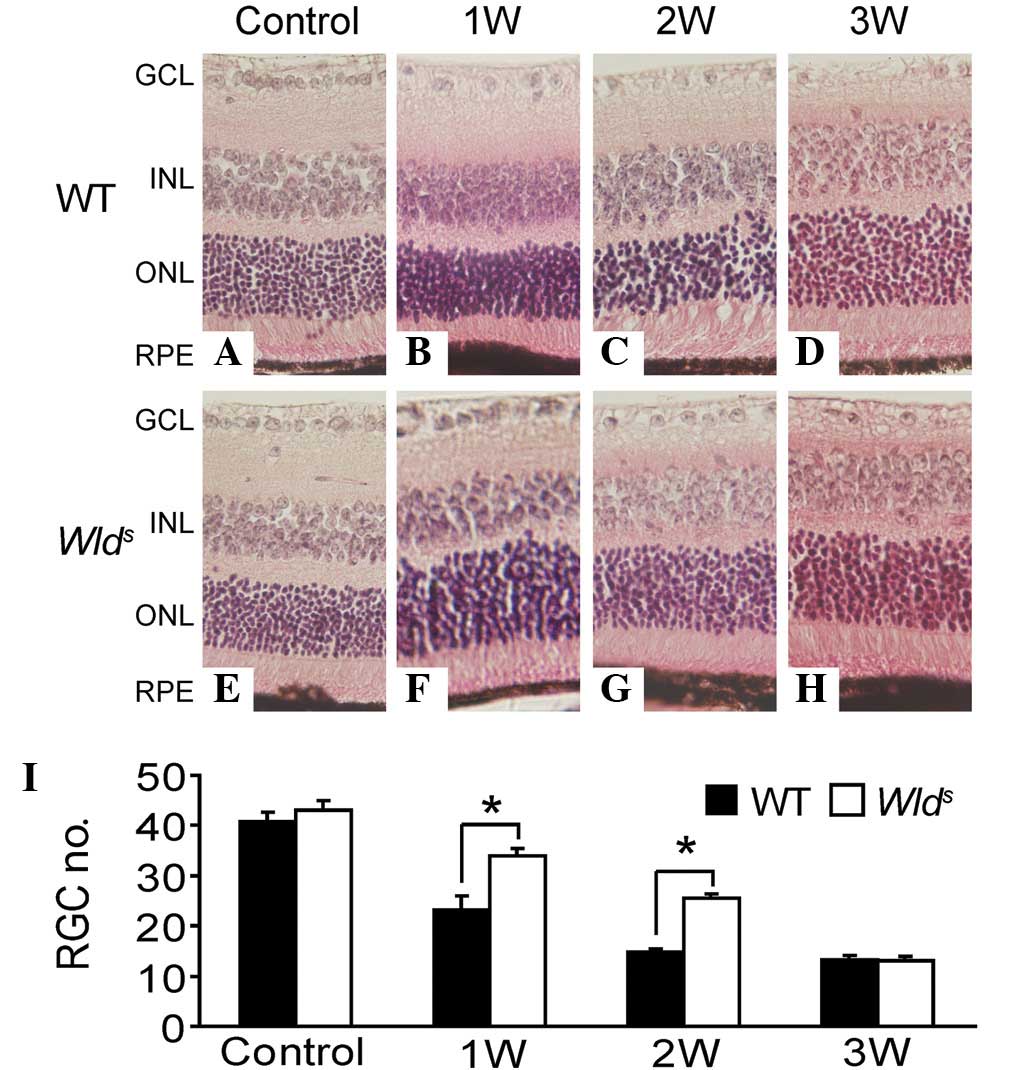 | Figure 2.(A–H) Representative retinal HE
staining of the WT and Wlds mice before and 1, 2
and 3 weeks after ON surgery (1:200). (I) Quantitative results of
number of RGCs in WT and Wlds retina before or 1,
2 and 3 weeks after ON surgery. GCL, ganglion cell layer; INL,
inner nuclear layer; ONL, outer nuclear layer; RPE, retinal pigment
epithelium; HE, hematoxylin and eosin; WT, wild-type;
Wlds, Wallerian degeneration slow; ON, optic
nerve; RGC, retinal ganglion cell. |
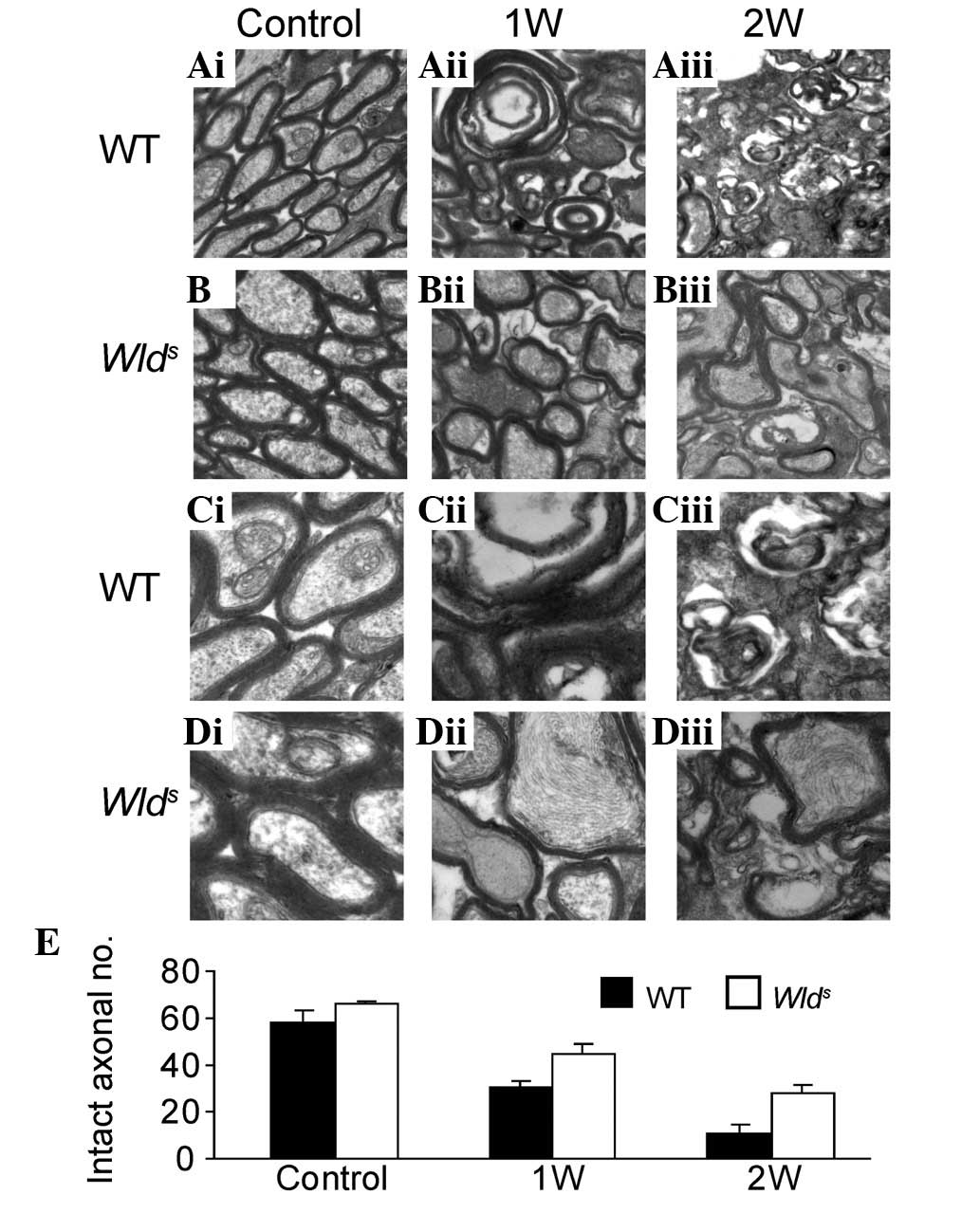
ON degeneration was delayed in
Wlds mice
One week after ON injury, ∼50% (for WT mice) and 70%
(for Wlds mice) of myelinated axons were observed
to be structurally preserved at the lesion site (Fig. 4Aii and Bii; P<0.05). Two weeks
after the ON lesion was created, more intact axons were preserved
in the Wlds mice than the WT mice (P<0.05;
Fig. 4Aiii and Biii), with 19.0%
of myelinated axons preserved in the WT mice (Fig. 3Aiii), compared with 42.0% in the
Wlds mice (Fig.
4Biii; P<0.05). The ON degeneration was mostly completed
within one week in the WT mice (Fig.
4Cii) and two weeks in Wlds mice (Fig. 4Diii). These results clearly
demonstrate that the progression of axon degeneration was
significantly delayed in injured Wlds ONs.
Plastic sections prepared from degenerating WT and
Wlds mouse nerves at various time points were
also examined and the numbers of morphologically preserved axons
were counted (Fig. 4E). Completely
degenerated nerves were observed one week after injury in WT mice
and two weeks in Wlds mice (Fig. 4E), suggesting that it takes ∼two
weeks for the Wlds mouse ONs to complete
morphological degeneration.
Discussion
The phenotype of Wlds mice is the
overexpression of a chimeric Wlds gene product,
the fusion protein Nmnat1 (6),
which is a key enzyme in the synthesis of NAD. Overexpression of
Nmnat1 may delay the mechanical or chemical axonal injury (9) and may even have protective effects
against toxic neuronal injury induced by vincristine (6). The protective effect of the gene has
been demonstrated to have several aspects, including the high
expression of the transgenic mouse motor nerve conduction fusion
protein, synaptic transmission, vesicle cycle and lesion morphology
of the motor nerve. Inhibition of the protein ubiquitination system
activity may also slow Wallerian degeneration, possibly through the
early stability of the axonal microtubule skeleton structure of
Wallerian degeneration (10).
However, the potential effects of the Wlds gene
against axonal injury-induced RGC cell body damage are not
fully understood.
Compared with the WT mice, the present results
showed that the VEP amplitude was decreased in
Wlds mice and the peak was delayed by at least
one week following the ON damage. These results together with the
the morphological changes suggest that the Wlds
gene delays RGC cell degeneration. Furthermore, the
immunohistochemical and electron microscopy findings in the ON
demonstrated that the ON demyelination and structural
disintegration in Wlds mice occurred at least one
week later than in the WT mice. Similarly, the ERG amplitude in
Wlds mice decreased and the PERG was delayed. The
decline in the number of RGCs also occurred in the later stages
(after two weeks) in Wlds mice. The RGC
functional loss was delayed by one week vs. the WT mice. These
results were further supported by the morphological observations.
One week after the ON injury, the retina immunohisothcemical
staining results showed that the volume of normal RGCs in the
Wlds mice were significantly higher than that of
the WT mice and the number of TUNEL-positive cells was lower.
Together these results indicate that the Wlds
gene delays axonal degeneration and may also be protective for RGC
cell bodies.
Abbreviations:
|
VEP
|
visual evoked potential
|
|
CNS
|
central nervous system
|
|
NAD
|
nicotinamide adenine dinucleotide
|
|
RGC
|
retinal ganglion cell
|
|
ERGs
|
electroretinograms
|
|
Wlds
|
Wallerian degeneration slow
|
|
LFB
|
Luxol fast blue
|
|
TUNEL
|
terminal deoxynucleotidyl transferase
(TdT)-mediated dUTP nick end-labeling
|
Acknowledgements
This work was generously supported by
grants from the National Natural Science Foundation of China (Nos.
ky1040511101111116, 81271028), a grant from Nanjing Medical
University (2011NJMU143) and Post-doc fund of Jiangsu Province (No.
1002009B).
References
|
1.
|
Jackson GR and Owsley C: Visual
dysfunction, neurodegenerative diseases, and aging. Neurol Clin.
21:709–728. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Wang JT, Medress ZA and Barres BA: Axon
degeneration: molecular mechanisms of a self-destruction pathway. J
Cell Biol. 196:7–18. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Feng Y, Yan T, He Z and Zhai Q:
Wld(S), Nmnats and axon degeneration - progress in the past
two decades. Protein Cell. 1:237–245. 2010. View Article : Google Scholar
|
|
4.
|
Wang J and He Z: NAD and axon
degeneration: from the Wlds gene to neurochemistry. Cell Adh
Migr. 3:77–87. 2009. View Article : Google Scholar
|
|
5.
|
Fernando FS, Conforti L, Tosi S, Smith AD
and Coleman MP: Human homologue of a gene mutated in the slow
Wallerian degeneration [C57BL/Wld(s)] mouse. Gene.
284:23–29. 2002.PubMed/NCBI
|
|
6.
|
Xue L, Fletcher GC and Tolkovsky AM:
Autophagy is activated by apoptotic signalling in sympathetic
neurons: an alternative mechanism of death execution. Mol Cell
Neurosci. 14:180–198. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Fainzilber M and Twiss JL: Tracking in the
Wlds- the hunting of the SIRT and the luring of the Draper.
Neuron. 50:819–821. 2006.
|
|
8.
|
Yuan S, Zhang W, Ding J, Yao J, Jiang Q
and Hu G: Increased sensitivity to retinal light damage in
aquaporin-4 knockout mice. Exp Eye Res. 89:119–122. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Araki T, Sasaki Y and Milbrandt J:
Increased nuclear NAD biosynthesis and SIRT1 activation prevent
axonal degeneration. Science. 305:1010–1013. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Zhai Q, Wang J, Kim A, et al: Involvement
of the ubiquitin-proteasome system in the early stages of wallerian
degeneration. Neuron. 39:217–225. 2003. View Article : Google Scholar : PubMed/NCBI
|