Introduction
Mucocele of the appendix is a cystoid extension of
the appendix resulting from mucus accumulation in the appendix
cavity (1). It is also a rare
pathology of the appendix without characteristic clinical symptoms
(2,3). Although mucocele of the appendix is
often discovered following surgery due to the difficulty in
obtaining a preoperative diagnosis, recent advances in imaging
technology have led to an improved preoperative diagnostic rate.
Kim et al (4) performed a
detailed examination of mucocele of the appendix in 17 patients by
computed tomography (CT) and ultrasonography (US) and suggested
that the presence of a focal nodular lesion in the tumor cavity is
an important predictor of malignancy.
The current report describes a case of mucinous
cystadenocarcinoma of the appendix in which contrast-enhanced US
(CEUS) was useful for the detailed assessment of blood flow in
projections in the mass cavity. The radiographic change was
observed after 1 year and 7 months. Written informed consent was
obtained from the patient.
Case report
A 63-year-old female was admitted to Tokyo Rosai
Hospital with discomfort in the right lower quadrant, which the
patient had being experiencing since approximately January 2011.
Physical examination revealed no tenderness; however, a palpable,
fist-sized mass in the right lower quadrant prompted abdominal CT,
which revealed a 60-mm cystic mass at the site corresponding to the
appendix with calcification in its wall on the appendicular tip.
With no thickening or contrast enhancement in the entire wall of
the mass, cystadenoma, as opposed to carcinoma was suspected
(Fig. 1). Since the possibility of
carcinoma could not be ruled out, surgical removal of the mass was
recommended; however, the patient refused surgery and was placed on
a careful outpatient follow-up program.
Three months later, the patient returned to the
hospital. Abdominal CT revealed no changes compared with the
previous examination. The patient was advised to return to the
outpatient clinic in 3 months; however, the patient did not return.
Later, the patient presented with persistent pain in the right
lower quadrant, which the patient had experienced since August
2012. On examination, a mass was felt in the right lower quadrant
that resembled the one felt previously and tenderness was
experienced at the same site. The patient was then admitted for
workup. The patient had no history of alcohol or smoking and the
prior medical history included surgery for internal hemorrhoids at
the age of 59 years. No signifant family history was reported and
no oral medication was being used. On admission, the patient had
clear sensorium and a blood pressure of 123/73 mmHg, a pulse rate
of 60 beats/min (non-arrhythmic) and a body temperature of 37.5°C.
The palpebral conjunctiva was not anemic and no yellow
discoloration of the bulbar conjunctiva was observed. Heart and
breath sounds were noted to be clear. The abdomen was flat and soft
with a palpable fist-sized mass present in the right lower
quadrant. The mass was slightly hard and minimally movable with
tenderness; however, no rebound tenderness or muscular rigidity was
apparent. The liver and spleen were impalpable. Hematological
examination on admission revealed mild anemia (hemoglobin, 11.4
g/dl) and increased inflammatory reaction (C-reactive protein, 6.5
mg/dl). No increase in the levels of tumor markers was observed
(Table I).
 | Table I.Blood laboratory findings on
admission. |
Table I.
Blood laboratory findings on
admission.
| Diagnostic blood
tests | Results |
|---|
| Biochemistry | |
| CRP (mg/dl) | 6.5 |
| Na (mEq/l) | 137 |
| K (mEq/l) | 4.0 |
| Cl (mEq/l) | 100 |
| TP (g/dl) | 7.9 |
| Alb (g/dl) | 4.0 |
| T Bil
(mg/dl) | 0.6 |
| D Bil
(mg/dl) | 0.4 |
| AST (IU/l) | 28 |
| ALT (IU/l) | 29 |
| LDH (IU/l) | 151 |
| ALP (IU/l) | 267 |
| GGT (IU/l) | 62 |
| T Cho
(mg/dl) | 178 |
| TG (mg/dl) | 166 |
| CK (IU/l) | 57 |
| BUN (mg/dl) | 13 |
| Cr (mg/dl) | 0.53 |
| BS (mg/dl) | 107 |
| HbA1c (%) | 6.0 |
| PT (%) | 86 |
| APTT (sec) | 30.4 |
| Hematology | |
| WBC
(cells/μl) | 5500 |
| RBC
(cells/μl) |
365×104 |
| Hgb (g/dl) | 11.4 |
| Hct (%) | 33.2 |
| PLT
(n/μl) |
23.0×104 |
| Tumor marker | |
| CEA (ng/ml) | 2.7 |
| CA19-9
(U/ml) | 3.0 |
| CA125 (U/ml) | 13.1 |
Abdominal CT on day 2 revealed no change in the size
of the existing cystic mass from the previous CT scan performed in
January 2011; however, it revealed thickening of the mass wall on
the appendicular ostium and contrast enhancement at the
corresponding site. No projection was observed in the mass cavity
(Fig. 2). On abdominal US on day
2, the mass was anechoic overall and demonstrated a partly layered
echo pattern. The mass wall on the appendicular ostium was
thickened with a 13-mm projection protruding toward the cavity from
part of the wall. Another 9-mm projection was also observed in the
appendicular tip (Fig. 3).
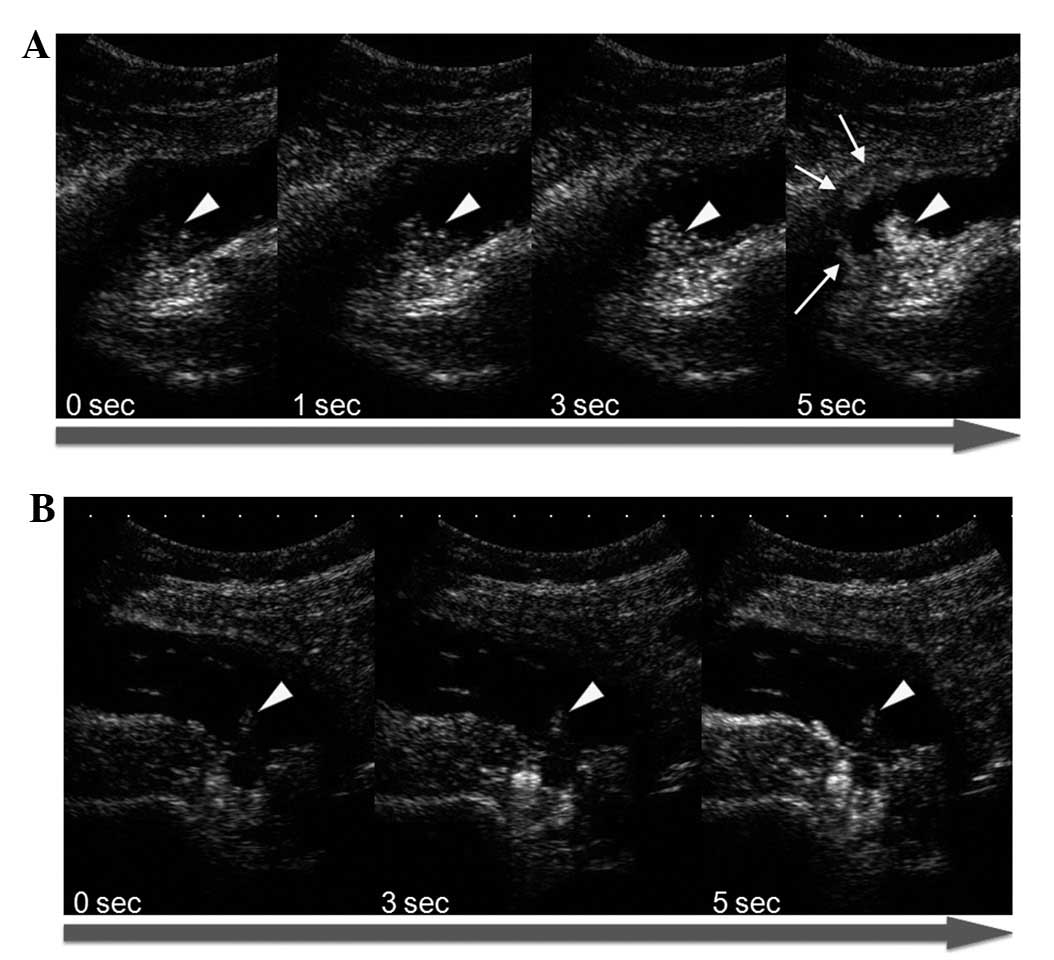
CEUS was then performed to assess blood flow using a
Toshiba SSA-790A US system (Aplio XG; Toshiba Medical Systems,
Otawara, Japan) with a 3.75-MHz convex probe (PVT-375BT). Imaging
was performed with a mechanical index of 0.21 and the focus was
adjusted to the depth of the mass. After imaging conditions were
set, Sonazoid (perfluorobutane; GE Healthcare, Oslo, Norway) was
infused at the recommended dose of 0.015 ml/kg via the cubital
vein. Contrast enhancement was observed in the thickened wall of
the mass on the appendicular ostium and in the projection on the
same side; however, not in the projection on the appendicular tip
(Fig. 4).
Based on the thickened and contrast-enhanced wall of
the mass on the appendicular ostium on abdominal CT and US, as well
as contrast enhancement of the projection on the appendicular
ostium on US, the mass was diagnosed as mucinous cystadenocarcinoma
of the appendix and ileocecal resection was performed on day 10.
The mass was excised with surrounding connective tissue with care
taken not to break the mass.
Gross pathological findings
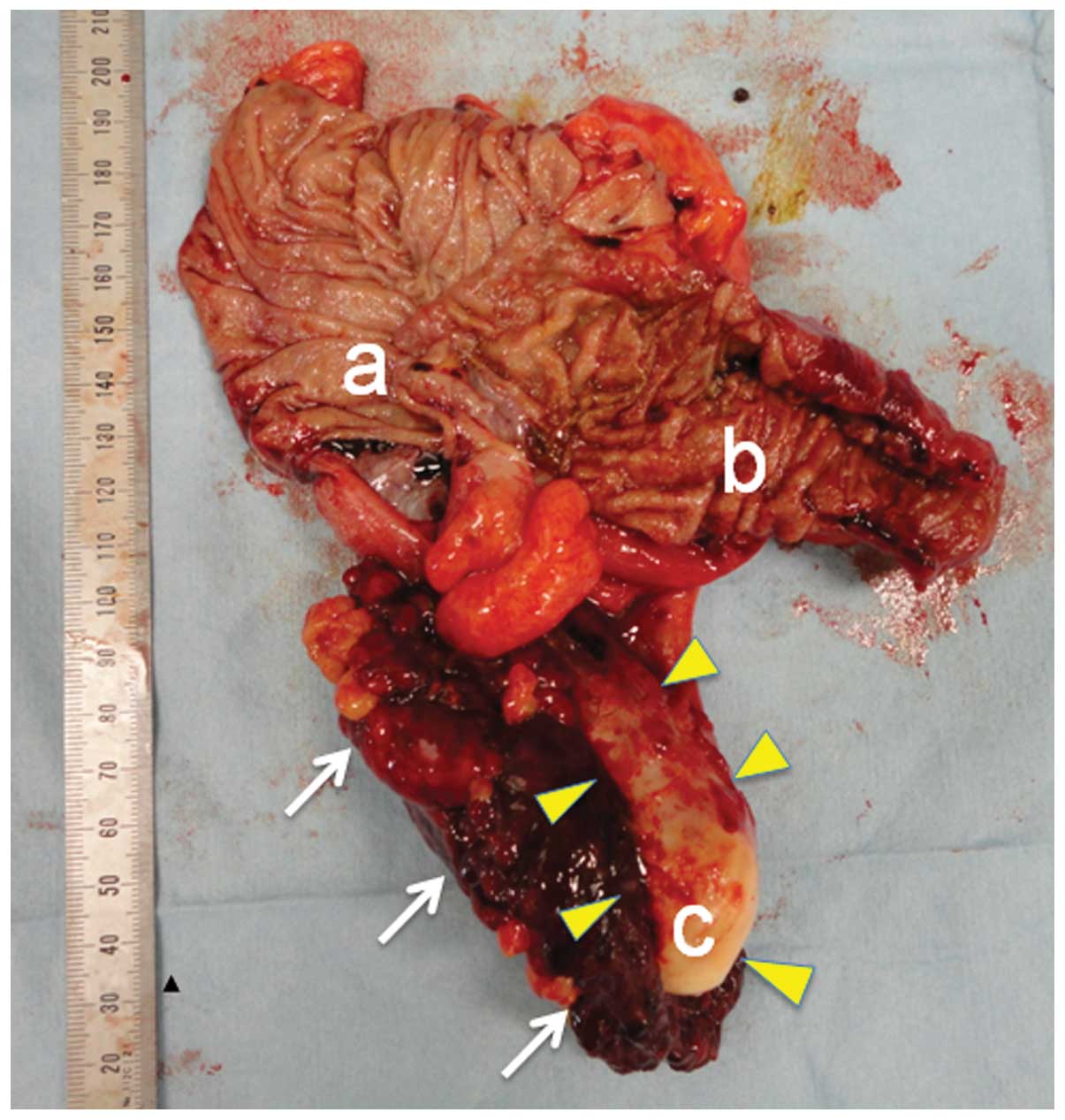
The appendix was swollen with a 60-mm cyst with a
glossy white surface. No rupture of the mass was observed (Fig. 5).
Histopathological findings
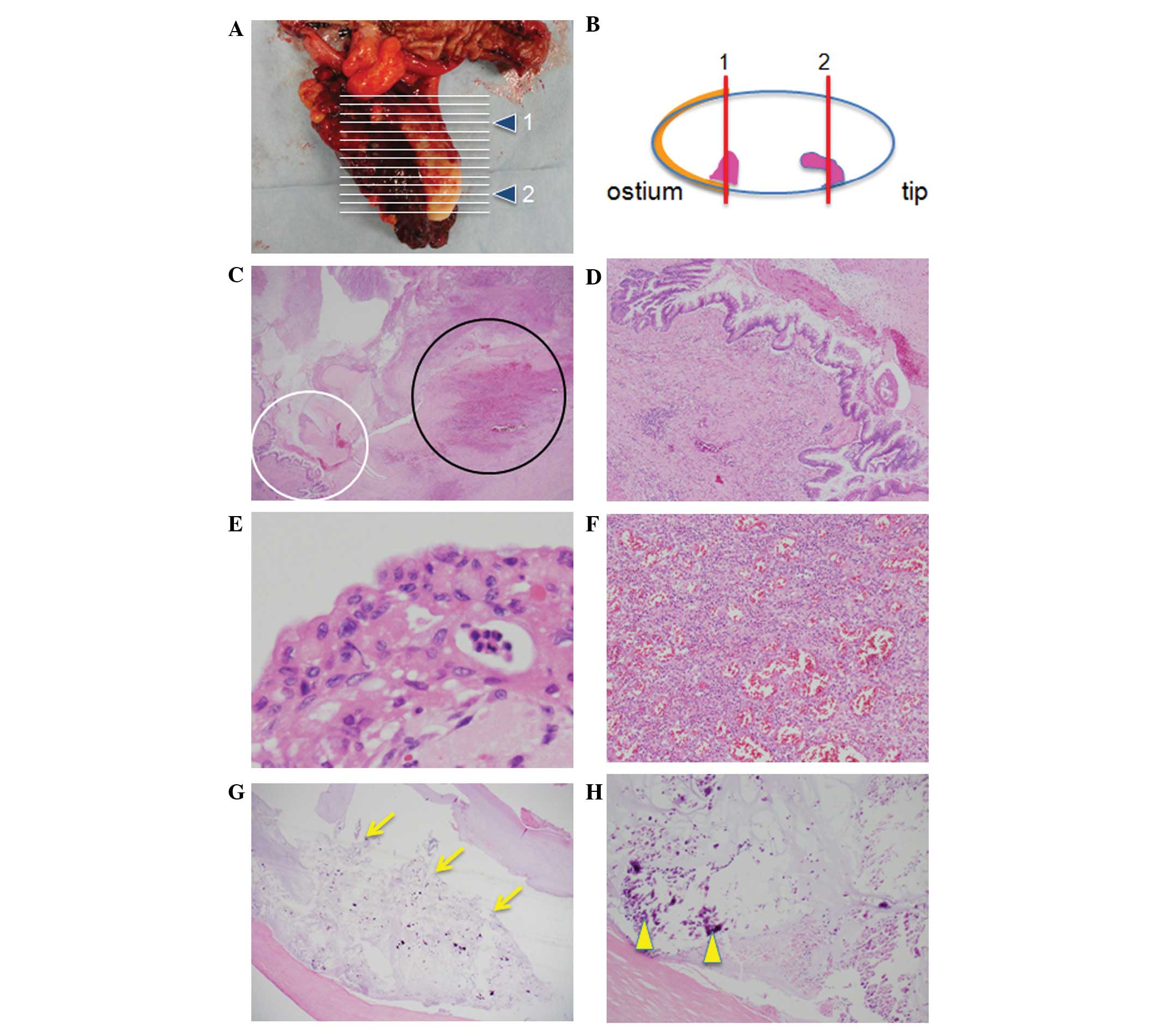
The mass wall was thickened on the appendicular
ostium and accompanied by enlarged nuclei and pseudostratified
cells, leading to the diagnosis of adenocarcinoma. The protrusion
on the appendicular ostium was located inside the thickened wall
and composed of granulation tissue with proliferating capillaries.
The protrusion on the appendicular tip was composed of mucus, and
part of the wall was calcified (Fig.
6).
Discussion
Mucocele of the appendix is a cystoid extension of
the appendix resulting from mucus accumulation in the appendix
cavity that was initially described as hydrops processus
vermiformis by Rokitansky in 1842 (1). It is a rare pathology of the
appendix, accounting for 0.07-0.3% of all appendectomy cases
(2,3). Mucocele of the appendix commonly
affects middle-aged to older females and is often accompanied by
discomfort or pain and a palpable mass in the right lower quadrant.
However, symptoms are non-specific in a number of cases and 20–30%
of cases are diagnosed without symptoms (5).
Kalmon and Winningingham (6) defined three factors that lead to the
development of mucocele of the appendix: progressive narrowing of
the valvular opening of the appendix, aseptic content and sustained
mucus production. Causes of obstruction include inflammation,
bending, torsion and ileocecal tumor. The most commonly used
pathological classification system was developed by Higa et
al (7), who defined the
following three types and reported their respective incidence: i)
focal or diffuse mucosal hyperplasia (25%); ii) mucinous
cystadenoma (63%); and iii) mucinous cystadenocarcinoma (12%).
With conventional imaging techniques, findings
suggestive of adenoma have been observed in a number of cases of
mucinous cystadenocarcinoma of the appendix, making it difficult to
distinguish precisely between the two types of lesions. In
addition, since a ruptured mass may lead to pseudomyxoma peritonei
(8), surgery is often performed
immediately after diagnosis. However, recent advances in imaging
modalities have led to improved accuracy of preoperative diagnosis
of the condition (9,10), and US and CT have proved effective
for diagnosing mucocele of the appendix (4,11).
On CT, the lesion is visualized as a round or oval,
encapsulated, large cystic mass (12,13).
Calcification of the cyst wall is highly specific to this lesion
and has been shown to be a useful feature for differentiating the
cyst from an abscess (4,14,15).
It is considered difficult to distinguish between the two lesions
based only on wall thickening and the presence of a focal nodular
lesion in the tumor cavity in the cyst cavity is considered a
potentially important predictor of malignancy (4). Balthazar et al (16) suggested that mucinous
cystadenocarcinoma of the appendix is visualized on CT as an
irregular, unilocular or multilocular, low-density area with
infiltration into adjacent organs, which is specific compared with
other types of mucocele of the appendix. In the present case,
however, the lesion was visualized as a round, low-density area.
This is may be due to the fact that the carcinoma arising from the
appendicular ostium infiltrated only up to the mesoappendix, as
confirmed pathologically.
Characteristic US findings include an anechoic or
hypoechoic area in the mass (4),
as well as fine punctuate, spiral or layered echo patterns
(4,11,17–19).
Spiral or layered echo patterns observed on US are considered to
represent highly viscous mucus, which is referred to by Caspi et
al as an ‘onion skin sign’, a finding specific to mucocele of
the appendix (17). In the present
case, layered echo patterns consisting primarily of an anechoic
area were also observed in the mass. In addition, a thickened mass
wall on the appendicular ostium and projections in the mass cavity
were also observed. A previous study suggested that a definitive
diagnosis of carcinoma was not made on the basis of wall thickening
alone since the presence of projections in the mass cavity is an
important finding that strongly suggests carcinoma (4). A detailed examination of the surgical
specimen revealed that the projection on the appendicular ostium
was a granulation tissue that protruded into the lumen and came
into contact with the carcinoma. Although it is unclear how the
granulation tissue was formed, we assume that it was a secondary
reaction to proliferating carcinoma cells. Thus, a mucocele of the
appendix with projection(s) in the mass cavity is likely to be
solidified mucus, a mass of carcinoma cells or granulation tissue
formed in response to carcinoma proliferation. The projections in
the mass cavity were subjected to CEUS for assessment of blood
flow. CEUS is being increasingly used as a first-line tool for
detecting and characterizing hepatic liver lesions (20–25).
Since its introduction to Japan in January 2007, the ultrasound
contrast agent Sonazoid has been used in detailed studies on liver
tumors (26–34), chronic liver disease (35–40)
and other organs (41,42).
While the usefulness of color Doppler US has been
suggested for determining whether a projection is mucus or a solid
mass (43), CEUS provides a higher
level of spatial resolution and more detailed information on blood
flow and is thus used to rule out solidified mucus. We consider
that CEUS is an important tool for determining the treatment
strategy. With no previous study closely examining the mucocele of
the appendix by CEUS, future studies should consider this modality
as an important preoperative diagnostic tool for this
condition.
We experienced a case of mucinous cystadenocarcinoma
of the appendix in which thickening of the mass wall was observed 1
year and 7 months after the first presentation. In the present
case, projections in the mass cavity, which were not visualized on
abdominal CT, were successfully visualized by B-mode US.
Furthermore, the use of CEUS made it possible to determine
precisely whether the projections were solidified mucus or a solid
tumor. These findings suggest the utility of B-mode US combined
with CT for diagnostic imaging of mucocele, with CEUS being
particularly useful for the assessment of blood flow in
projections.
Abbreviations:
|
CT
|
computed tomography;
|
|
US
|
ultrasonography
|
References
|
1.
|
Rokitansky KF: Beritrage zur Erkrankungen
der Wurmfortsazentzundung. Wien Med Presse. 26:428–435. 1866.(In
German).
|
|
2.
|
González Moreno S, Shmookler BM and
Sugarbaker PH: Appendiceal mucocele. Contraindication to
laparoscopic appendectomy. Surg Endosc. 12:1177–1179.
1998.PubMed/NCBI
|
|
3.
|
Blair NP, Bugis SP, Turner LJ and MacLeod
MM: Review of the pathologic diagnoses of 2,216 appendectomy
specimens. Am J Surg. 165:618–620. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Kim SH, Kim HK, Lee WJ, et al: Mucocele of
the appendix; ultrasonographic and CT findings. Abdom Imaging.
23:292–296. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Yajima H, Kokudo N, Takahashi T, et al: A
case of appendiceal mucocele diagnosed preoperatively by
ultrasonography. J Med Ultrasonics. 29:171–175. 2002.(In
Japanese).
|
|
6.
|
Kalmon EH and Winningingham EV: Mucocele
of the appendix. Am J Roentgenol Radium Ther Nucl Med. 72:432–435.
1954.PubMed/NCBI
|
|
7.
|
Higa E, Rosai J, Pizzimbono CA and Wise L:
Mucosal hyperplasia, mucinous cystadenoma, and mucinous
cystadenocarcinoma of the appendix. A re-evaluation of appendiceal
“mucocele”. Cancer. 32:1525–1541. 1973.PubMed/NCBI
|
|
8.
|
Morson BC: Gastrointestinal Pathology. 2nd
edition. Blackwell Scientific Publications; London: pp. 449–482.
1979
|
|
9.
|
Kahn M and Friedman IH: Mucocele of the
appendix: diagnosis and surgical management. Dis Colon Rectum.
22:267–269. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Simmons K and Sage MR: Mucocele of the
appendix. Australas Radiol. 23:33–35. 1979. View Article : Google Scholar
|
|
11.
|
Degani S, Shapiro I, LeibovitZ Z and Ohel
G: Sonographic appearance of appendiceal mucocele. Ultrasound
Obstet Gynecol. 19:99–101. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Horgan JG, Chow PP, Richter JO, et al: CT
and sonography in the recognition of mucocele of the appendix. AJR
Am J Roentgenol. 143:959–962. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Matsumoto K, Kanazawa S and Segawa K: A
case of mucinous cystadenoma of appendix with a characteristic
image on abdominal ultrasonography. Gastroenterol Endosc.
30:999–1004. 1988.(In Japanese).
|
|
14.
|
Pickhardt PJ, Levy AD, Rohrmann CA Jr and
Kende AI: Primary neoplasms of the appendix: radiologic spectrum of
disease with pathologic correlation. Radiographics. 23:645–662.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Madwed D, Mindelzun R and Jeffrey RB Jr:
Mucocele of the appendix: imaging findings. AJR Am J Roentgenol.
159:69–72. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Balthazar EJ, Megibow AJ, Gordon RB, et
al: Computed tomography of the abnormal appendix. J Comput Assist
Tomogr. 12:595–601. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Caspi B, Cassif E, Auslender R, et al: The
onion skin sign: a specific sonographic marker of appendiceal
mucocele. J Ultrasound Med. 23:117–121. 2004.PubMed/NCBI
|
|
18.
|
Athey PA, Hacken JB and Estrada R:
Sonographic appearance of mucocele of the appendix. J Clin
Ultrasound. 12:333–337. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Fallon MJ, Low VH and Yu LL: Mucunous
cystadenoma of the appendix with unusual sonographic appearance.
Australas Radiol. 38:339–341. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Bartolotta TV, Midiri M, Quaia E, et al:
Benign focal liver lesions: spectrum of findings on
SonoVue-enhanced pulse-inversion ultrasonography. Eur Radiol.
15:1643–1649. 2005. View Article : Google Scholar
|
|
21.
|
Dietrich CF: Characterisation of focal
liver lesions with contrast enhanced ultrasonography. Eur J Radiol.
51(Suppl): S9–S17. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Iijima H, Moriyasu F, Tsuchiya K, et al:
Decrease in accumulation of ultrasound contrast microbubbles in
non-alcoholic steatohepatitis. Hepatol Res. 37:722–730. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Fujita Y, Watanabe M, Sasao K, et al:
Investigation of liver parenchymal flow using contrast-enhanced
ultrasound in patients with alcoholic liver disease. Alcohol Clin
Exp Res. 28(Suppl Proceedings): 169S–173S. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Ogawa S, Kumada T, Toyoda H, et al:
Evaluation of pathological features of hepatocellular carcinoma by
contrast-enhanced ultrasonography: comparison with pathology on
resected specimen. Eur J Radiol. 59:74–81. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Basilico R, Blomley MJ, Harvey CJ, et al:
Which continuous US scanning mode is optimal for the detection of
vascularity in liver lesions when enhanced with a second generation
contrast agent? Eur J Radiol. 41:184–191. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Takahashi M, Maruyama H, Ishibashi H,
Yoshikawa M and Yokosuka O: Contrast-enhanced ultrasound with
perflubutane microbubble agent: evaluation of differentiation of
hepatocellular carcinoma. AJR Am J Roentgenol. 196:W123–W131. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
27.
|
Hiraoka A, Hirooka M, Koizumi Y, et al:
Modified technique for determining therapeutic response to
radiofrequency ablation therapy for hepatocellular carcinoma using
US-volume system. Oncol Rep. 23:493–497. 2010.
|
|
28.
|
Luo W, Numata K, Kondo M, et al:
Sonazoid-enhanced ultrasonography for evaluation of the enhancement
patterns of focal liver tumors in the late phase by intermittent
imaging with a high mechanical index. J Ultrasound Med. 28:439–448.
2009.PubMed/NCBI
|
|
29.
|
Shiozawa K, Watanabe M, Kikuchi Y, et al:
Evaluation of sorafenib for hepatocellular carcinoma by
contrast-enhanced ultrasonography: a pilot study. World J
Gastroenterol. 18:5753–5758. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
30.
|
Kudo M: New sonographic techniques for the
diagnosis and treatment ofhepatocellular carcinoma. Hepatol Res.
37(Suppl 2): S193–S199. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
31.
|
Wakui N, Takayama R, Kamiyama N, et al:
Diagnosis of hepatic hemangioma by parametric imaging using
sonazoid-enhanced US. Hepatogastroenterology. 58:1431–1435. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
32.
|
Shiozawa K, Watanabe M, Takayama R, et al:
Evaluation of local recurrence after treatment for hepatocellular
carcinoma by contrast-enhanced ultrasonography using Sonazoid:
comparison with dynamic computed tomography. J Clin Ultrasound.
38:182–189. 2010.
|
|
33.
|
Wakui N, Sumino Y and Kamiyama N: A case
of high-flow hepatic hemangioma: analysis by parametoric imaging
using sonazoid-enhanced ultrasonography. J Med Ultrasonics.
37:87–90. 2010. View Article : Google Scholar
|
|
34.
|
Wakui N, Takayama R, Matsukiyo Y, et al: A
case of poorly differentiated hepatocellular carcinoma with
intriguing ultrasonography findings. Oncol Lett. 4:393–397.
2012.PubMed/NCBI
|
|
35.
|
Wakui N, Takayama R, Kanekawa T, et al:
Usefulness of arrival time parametric imaging in evaluating the
degree of liver disease progression in chronic hepatitis C
infection. J Ultrasound Med. 31:373–382. 2012.PubMed/NCBI
|
|
36.
|
Wakui N, Takayama R, Mimura T, Kamiyama N,
Maruyama K and Sumino Y: Drinking status of heavy drinkers detected
by arrival time parametric imaging using sonazoid-enhanced
ultrasonography: study of two cases. Case Rep Gastroenterol.
26:100–109. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
37.
|
Wakui N, Fujita M, Oba N, et al:
Endoscopic nasobiliary drainage improves jaundice attack symptoms
in benign recurrent intrahepatic cholestasis: A case report. Exp
Ther Med. 5:389–394. 2013.PubMed/NCBI
|
|
38.
|
Ishibashi H, Maruyama H, Takahashi M, et
al: Assessment of hepatic fibrosis by analysis of the dynamic
behaviour of microbubbles during contrast ultrasonography. Liver
Int. 30:1355–1363. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
39.
|
Yoshikawa S, Iijima H, Saito M, et al:
Crucial role of impaired Kupffer cell phagocytosis on the decreased
Sonazoid-enhanced echogenicity in a liver of a nonalchoholic
steatohepatitis rat model. Hepatol Res. 40:823–831. 2010.
View Article : Google Scholar
|
|
40.
|
Wakui N, Takayama R, Matsukiyo Y, et al:
Visualization of segmental arterialization with arrival time
parametric imaging using Sonazoid-enhanced ultrasonography in
portal vein thrombosis: A case report. Exp Ther Med. 5:673–677.
2013.PubMed/NCBI
|
|
41.
|
Onji K, Yoshida S, Tanaka S, et al:
Microvascular structure and perfusion imaging of colon cancer by
means of contrast-enhanced ultrasonography. Abdom Imaging.
37:297–303. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
42.
|
Imazu H, Uchiyama Y, Matsunaga K, et al:
Contrast-enhanced harmonic EUS with novel ultrasonographic contrast
(Sonazoid) in the preoperative T-staging for pancreaticobiliary
malignancies. Scand J Gastroenterol. 45:732–738. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
43.
|
Kameda T, Kawai F, Kase K, et al: Three
cases of appendiceal mucocele: specific ultrasonographic findings.
Jpn J Med Ultrasonics. 33:229–237. 2006.(In Japanese).
|