Introduction
Total knee arthroplasty (TKA) has become a
successful procedure for treating end-stage osteoarthritis and
rheumatoid arthritis (1–5). The mobile-bearing (MB) TKA design is
assumed to provide a greater freedom of motion compared with the
fixed-bearing (FB) variant, since the insert does not restrict the
natural movements of the femoral component. This enables the
reproduction of tibial internal rotation during flexion, reduces
contact stresses and linear wear of the polyethylene, and improves
patellofemoral tracking (6–10).
This may, in turn, have a positive effect on the fixation of the
prosthesis to the bone, and thereby reduce the risk of a loosening
of the implant occurring.
Numerous trials have focused on the comparison of
clinical outcomes between MB and FB TKAs. During the short-term
follow-up period, no significant difference in clinical improvement
has been demonstrated between MB- and FB-implant groups (11–16).
In a prospective study, Hanusch et al (15) demonstrated that there was no
significant difference in the mean range of motion (ROM) or Knee
Society score (KSS) between MB and FB implants, at a mean follow-up
of 13.4 months. However, short-term results are not always
indicative of mid- and long-term outcomes. Controversy exists with
respect to the clinical and radiological differences in outcomes
between FB and MB TKAs during the mid- to long-term follow-up.
Matsuda et al (17)
revealed that no differences were exhibited in the rotational
alignment or the ROM between MB and FB implants for a total of 61
knee arthroplasties in the mid-term follow-up. By contrast, a study
by Higuchi et al (18), of
76 TKAs, demonstrated that the postoperative-extension ROM was
significantly improved following TKA using an MB implant, in
comparison with that employing an FB implant, at the four-year
follow-up.
The mid- to long-term results of the prosthesis are
important in evaluating the efficiency of implant. Although several
meta-analyses concerning the clinical differences between FB and MB
TKAs have been performed (19–22),
the pooled data were not analyzed according to the different
follow-up periods. In addition, a number of new randomized
controlled trials (RCTs) have recently emerged. Therefore, there is
a requirement for a new systematic review to compare the clinical,
radiological and general health results of the two types of
prostheses, at the mid- to long-term follow-up period.
Methods
Search strategy
We searched the Cochrane Central Register of
Controlled Trials (CENTRAL) in the Cochrane Library, Medline and
Embase. The search strategies used are demonstrated in Table I, along with the time span for the
searches. The bibliography of eligible studies was also searched to
identify further relevant trials.
 | Table I.Search strategies. |
Table I.
Search strategies.
| Database | Period of
search | Search
strategy |
|---|
| Medline
(Pubmed) | 1966-August
2012 | (((((“Arthroplasty,
Replacement, Knee”[Mesh])) OR (((knee)) AND (((((replacement*) OR
arthroplast*) OR prosthe*) OR implant) OR endoprosthe*)))) AND
(((((mobile bearing) OR mobile platform) OR rotating platform) OR
meniscal bearing) OR gliding bearing)) AND ((randomized controlled
trial[pt] OR controlled clinical trial[pt] OR randomized[tiab] OR
placebo [tiab] OR clinical trials as topic[mesh:noexp] OR randomly
[tiab] OR trial[ti]) NOT (animals[mh]NOT humans[mh])) |
| Cochrane Central
Register of Controlled Trials in the Cochrane library | Issue 2, 2012 | #1 MeSH descriptor
Arthroplasty, Replacement, Knee explode all trees |
| #2 (replacement*)
or (arthroplast*) or (prosthe*) or (implant) or (endoprosthe*) |
| #3 (knee) |
| #4 (#2 AND #3) |
| #5 (#1 AND #4) |
| #6 (mobile bearing)
or (mobile platform) or (rotating platform) or (meniscal bearing)
or (gliding bearing) |
| #7 (#1 AND #6) |
| Embase | 1974-August
2012 | ‘knee
arthroplasty’/exp OR ‘total knee replacement’/exp OR (replacement*
OR arthroplast* OR prosthe* OR implant OR endoprosthe* AND knee)
AND (mobile AND bearing OR (mobile AND platform) OR (rotating AND
platform) OR (meniscal AND bearing) OR (gliding AND bearing)) AND
(random* OR blind* OR placebo OR ‘meta analysis’) |
Eligibility criteria
The inclusion criteria for the articles selected
were as follows: i) the studies involved adult patients who had
undergone primary TKA; ii) the studies were RCTs comparing MB- and
FB TKAs and iii) the mean follow-up was >5 years. Animal and
cadaver studies were excluded, and no language restriction was
used.
Data extraction
Data were extracted independently from the included
studies by two reviewers (MC/DC), and disagreements were resolved
through consensus. Relevant data included demographic information,
methodological quality, duration of follow-up, clinical and
radiographical outcomes, patient preferences and complications.
Whenever studies pertained to the same population at different
follow-up periods, the investigation with the longer duration of
follow-up was retained to avoid the duplication of information.
Authors were contacted to request any unclear or missing data.
Disagreements concerning paper eligibility were resolved through
discussion.
Assessment of methodological
quality
The methodological quality of the trials was
evaluated independently by two reviewers (MC/DC), without masking
the trial names. The reviewers followed the instructions provided
in the Cochrane Handbook for Systematic Reviews of Interventions
(23). The following domains were
assessed: sequence generation, allocation concealment, blinding,
incomplete data outcomes, revealing of selective outcomes and any
remaining biases. When the information in the study was inadequate,
attempts were made to contact the authors in order to ensure that
the study was evaluated correctly.
Data analysis
The meta-analysis was conducted in accordance with
the recommendations of the Cochrane Collaboration, using Review
Manager (RevMan) software, version 5 (Copenhagen: The Nordic
Cochrane Centre, The Cochrane Collaboration, 2008). For continuous
outcomes, the weighted mean difference (WMD) and the 95% confidence
interval (CI) were calculated. For dichotomous outcomes, the
relative ratio (RR) and the 95% CI were calculated. Heterogeneity
was explored using the χ2 test and the I2
statistic. Heterogeneity was considered to be significant when the
P-value from the χ2 test was <0.10, or when the
I2 statistic was >50%. A fixed-effect model was used
if there was no statistical evidence of heterogeneity; otherwise, a
random-effect model was selected. The analysis was conducted on an
intention-to-treat bias, whenever possible, and a funnel plot was
used to explore the publication bias. P<0.05 was considered to
indicate a statistically significant difference.
Results
Description of studies
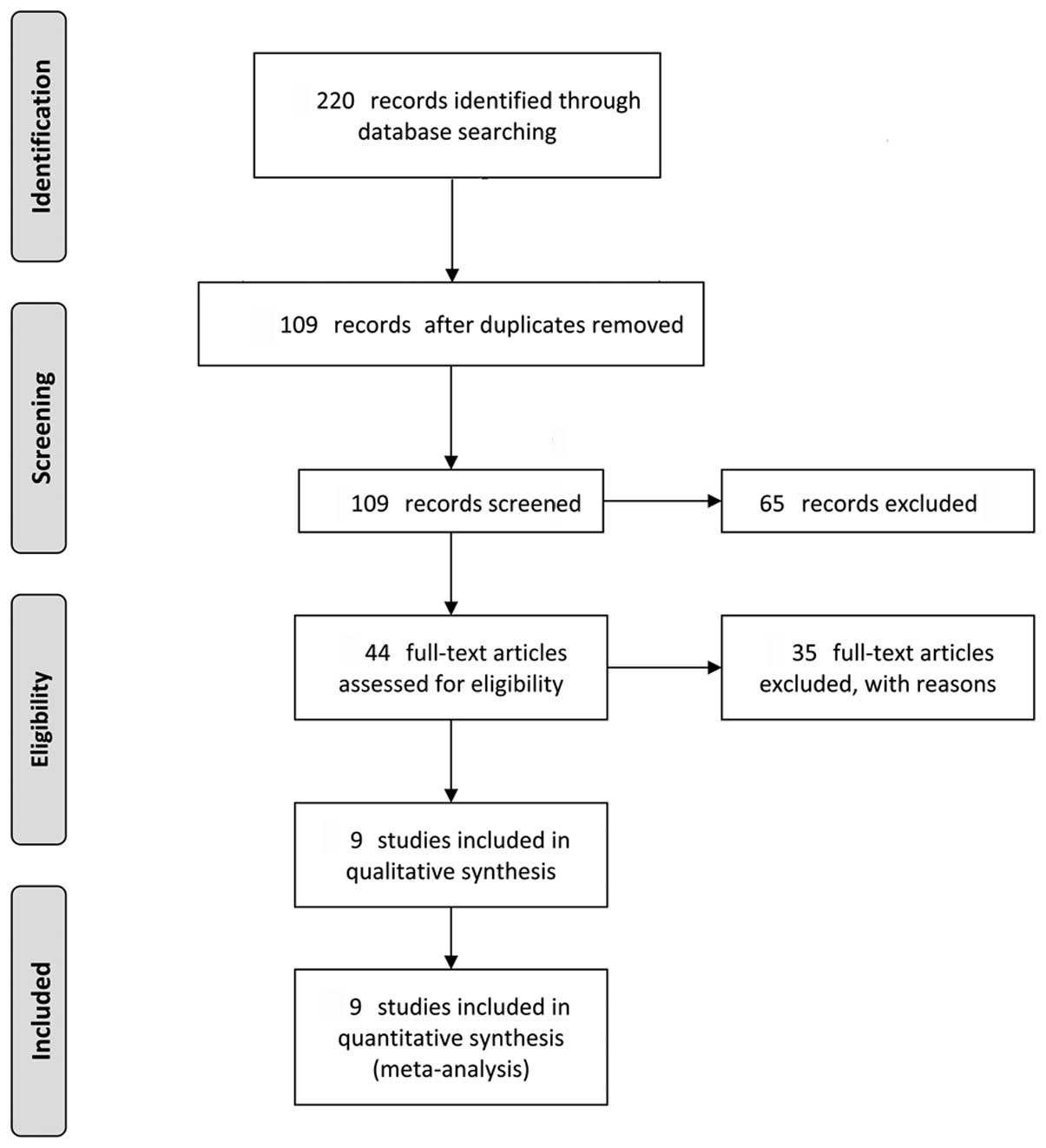
A preferred reporting items for systematic reviews
and meta-analyses (PRISMA) flow diagram outlining the literature
search results is summarized in Fig.
1. In the initial search, a total of 220 references were
identified electronically (Embase, 75; Medline, 92 and CENTRAL,
53). Following the application of the inclusion and exclusion
criteria to the study titles and abstracts, only nine trials
fulfilled the inclusion criteria.
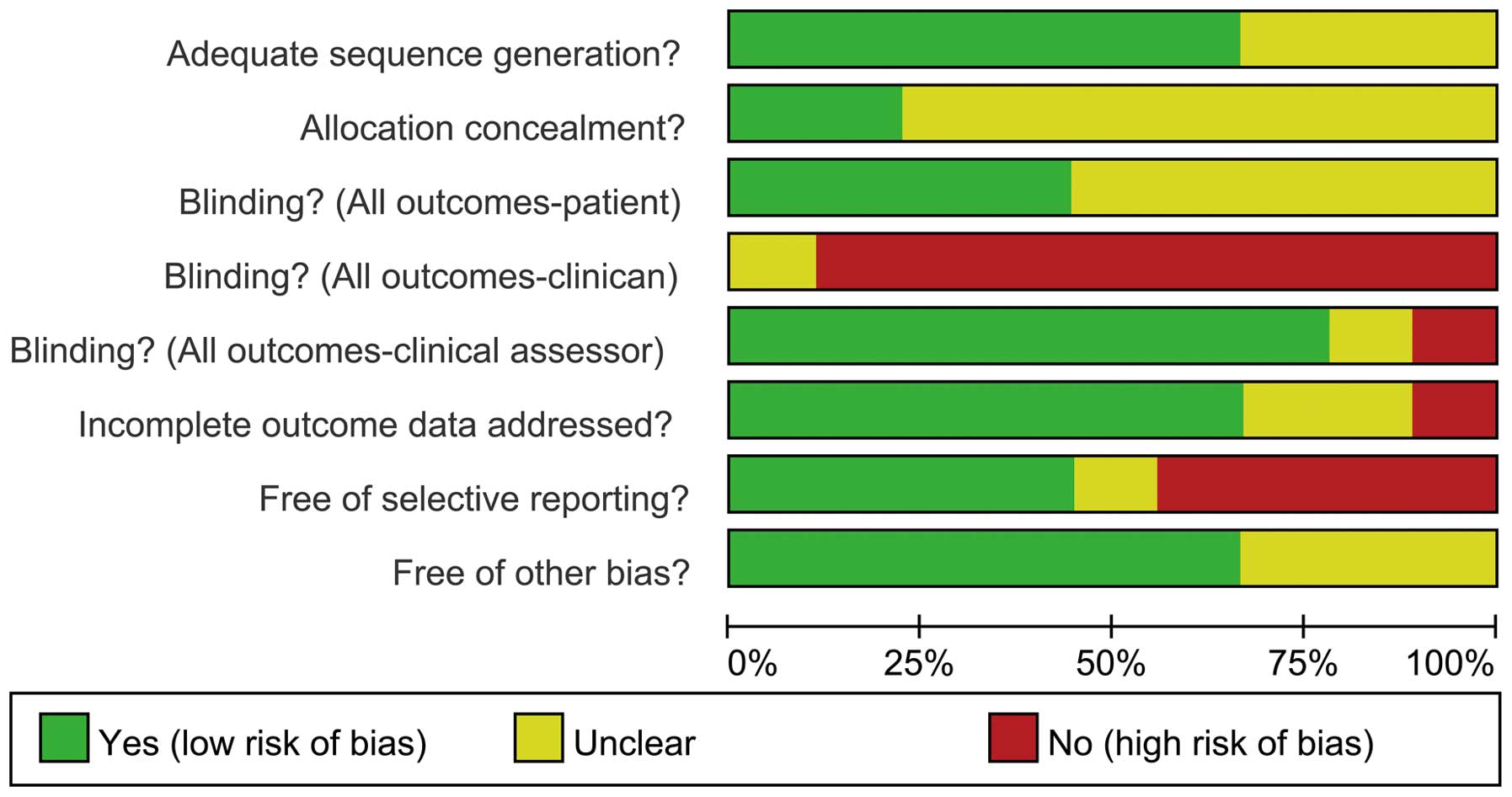
Risk of bias in included studies
The risk of bias is demonstrated graphically
(Fig. 2) and also summarized
(Fig. 3). Six (24–29)
of the nine trials (66.7%) exhibited adequate sequence generation
in the randomization process. However, only two trials (24,25)
stated the method of allocation concealment. In the study by
Lädermann et al (25), the
allocation concealment was performed using sealed opaque envelopes,
which were opened within 24 h prior to surgery; whereas in the
study by Mahoney et al (24), allocation concealment was ensured
by centralized randomization. Four of the nine trials (24–26,29)
performed patient blinding. Clinician blinding of the implant type
was impossible. All studies demonstrated assessor blinding, with
the exception of two trials (24,30).
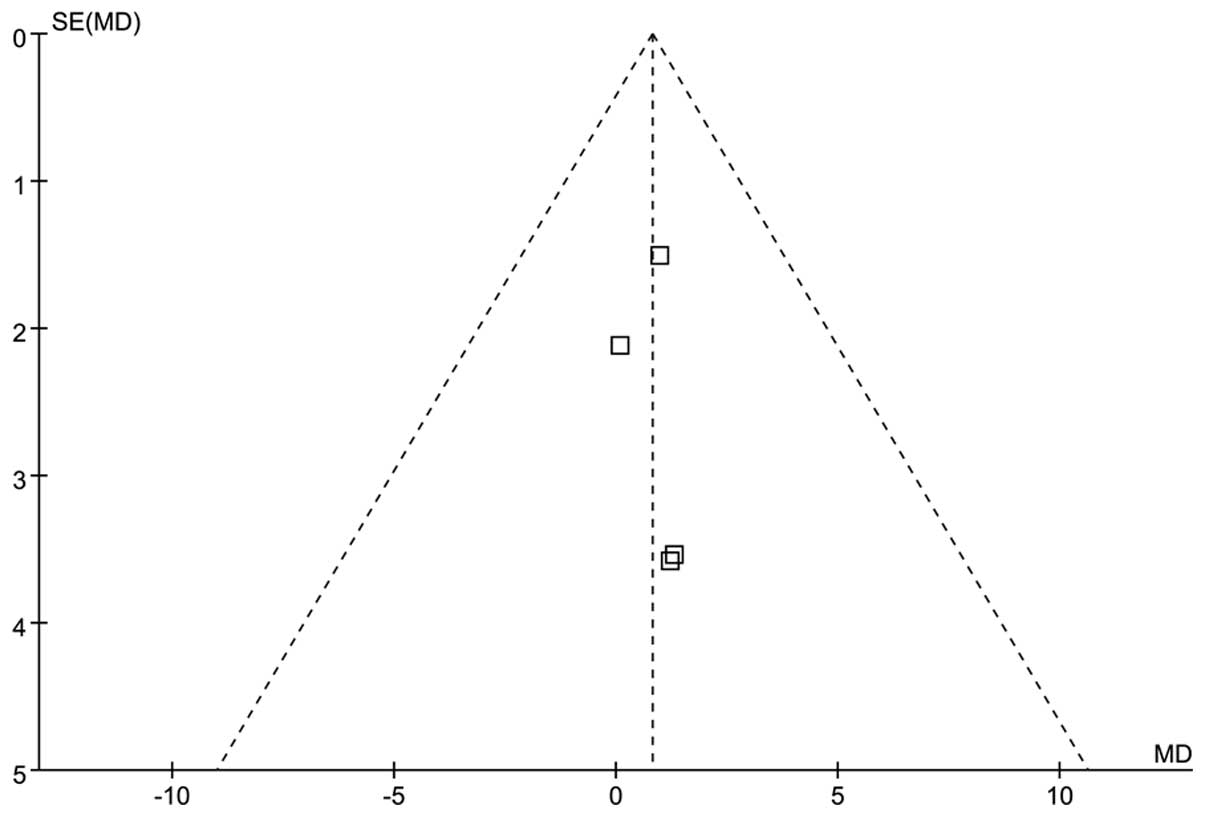
A funnel plot analysis of the combined trials indicated a symmetry,
demonstrating minimal recording bias (Fig. 4).
Effects of intervention
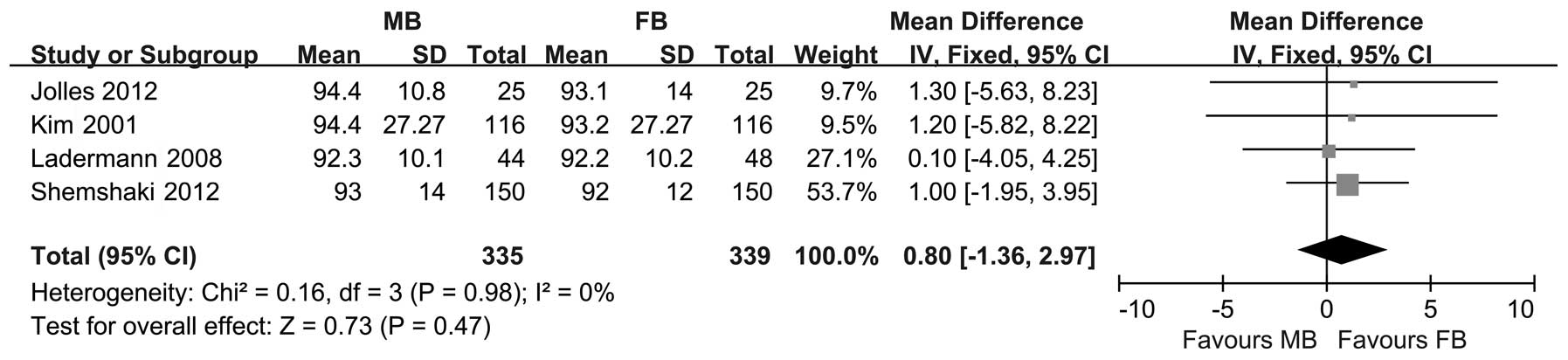
Knee score
The KSS (25,26,29,31),
the Hospital for Special Surgery (HSS) knee score (30,31)
and the Western Ontario and McMaster Universities Osteoarthritis
Index (WOMAC) (26) were used for
the clinical assessment of the patients (in four, two and one
trials, respectively). The meta-analysis revealed no significant
difference in the KSS between the FB and MB groups (WMD=0.80; 95%
CI, −1.36–2.97; P=0.47), and heterogeneity tests indicated minimal
interstudy heterogeneity (P=0.98 and I2=0%; fixed-effect
analysis; Fig. 5). In addition, a
fixed-effect model of the pooled data demonstrated that there was
no statistical difference in the HSS knee score between the two
groups (WMD=−0.65; 95% CI, −3.07-1.77; P=0.60). The study conducted
by Jolles et al (26) was
the sole study to assess WOMAC scores, and revealed that there was
no significant difference between the groups (P=0.94).
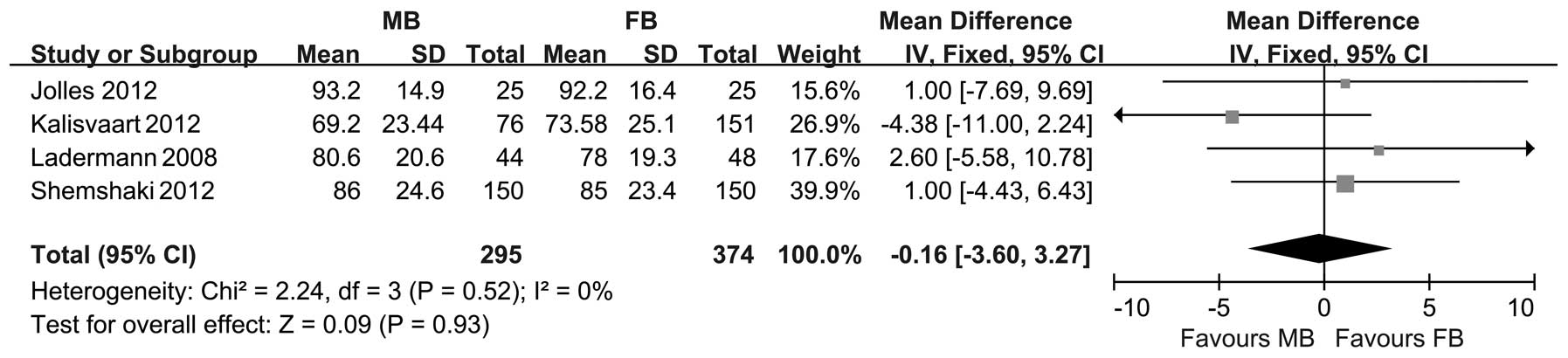
Four of the trials stated the KSS-function outcomes
(25–27,29).
There was no indication of statistical heterogeneity between the
trials (P=0.52 and I2=0%), and a fixed-effect model of
the pooled data revealed no significant difference in the
KSS-function outcomes between the FB and MB TKAs (WMD=−0.16; 95%
CI, −3.60-3.27; P=0.93; Fig.
6).
Maximum knee flexion
There were three trials (551 knees) that stated the
maximum knee flexion (25,27,31).
The meta-analysis did not demonstrate a significant difference
between the two groups (WMD=−0.52; 95% CI, −3.36-2.32; P=0.72), and
there was minimal interstudy heterogeneity (P=0.47 and
I2=0%; fixed-effect analysis).
Pain
The meta-analysis of the visual analog scales (VAS)
of pain in two of the trials indicated no significant difference
between the MB and FB TKAs (WMD=−0.02; 95% CI, −0.62-0.59; P=0.96),
with minimal interstudy heterogeneity (P=0.66 and I2=0%;
fixed-effect analysis) (25,26).
Patient preference
Only one trial revealed the patients’ preferences
with regard to their knee replacements. In the study by Matsuda
et al (17), 13 patients
underwent bilateral arthroplasty, where one knee was replaced with
an FB prosthesis and the other with an MB prosthesis. In these
patients, one patient favored the knee with the FB prosthesis, two
patients favored the MB prosthesis and the remaining ten patients
stated that there was no difference between their knees.
Quality of life
Three methods were used to measure the quality of
life in the selected studies. Shemshaki et al (29) evaluated short form 36 (SF-36)
scores, Lädermann et al (25) assessed SF-12 scores and Jolles
et al (26) used EuroQol-5D
scores. No significant differences in the quality of life scores
between the MB and FB TKAs were demonstrated in the studies
(P>0.05).
Radiological outcomes
There were two trials (277 knees) that revealed the
occurrence of nonprogressive radiolucent lines around the tibial or
femoral components (26,27). The meta-analysis demonstrated that
there was no significant difference between the FB and MB TKAs
(RR=1.05; 95% CI, 0.50–2.18; P=0.90).
Survivorship
Three studies (24,27,28)
revealed the Kaplan-Meier survival estimates for the prostheses;
however, two of these studies (24,28)
did not contain sufficient information for the meta-analysis.
Kalisvaart et al (27)
indicated that no difference was detected in implant durability or
fixation between the FB and MB prostheses after five years;
Kaplan-Meier analysis demonstrated five-year implant survival rates
of 98.0 and 98.7% for the FB and MB groups, respectively, with
revision surgery for any reason taken as the end point. Kim et
al (28) reported that the
Kaplan-Meier survival estimate revealed 99 and 100% survival rates
of the prosthesis in the MB and FB groups, respectively, after five
years (95% CI, 0.89–0.97), with all reasons for failure taken into
account. Mahoney et al (24) indicated that survival was similar
(P=0.351) between the MB and FB groups, with revision of any
component for any reason taken as the end point [90.1% (95% CI,
84.1–93.9) and 94.2% (95% CI, 90.1–96.6) for the MB and FB groups,
respectively).
Complications
Five of the studies provided data on postoperative
complications, including aseptic loosening, infection, revision,
patellar crepitus, complete wear of the polyethylene tibial bearing
and knee stiffness (19,20,22,23,27).
The meta-analysis did not identify any significant differences in
the RRs between MB and FB TKAs, with respect to aseptic loosening,
infection, revision, patellar crepitus or knee stiffness (Table II). Kim et al (31) reported two cases of complete wear
of the polyethylene tibial bearing in the FB cohort, and one case
of dislocation of the medial polyethylene tibial bearing in the MB
cohort.
 | Table II.Meta-analysis of the complications in
fixed-bearing and mobile-bearing TKAs. |
Table II.
Meta-analysis of the complications in
fixed-bearing and mobile-bearing TKAs.
| Complication | Studies
assessed | Incidence
| Relative Risk (95%
CI) | Overall effect
(P-value) | Heterogeneity
|
|---|
| Mobile | Fixed | I2
(%) | χ2
(P-value) |
|---|
| Aseptic
loosening | (19,22) | 2/328 | 3/406 | 1.11 (0.21,
5.89) | 0.90 | 44 | 0.18 |
| Revision | (19,20,27) | 25/412 | 17/419 | 1.48 (0.82,
2.67) | 0.20 | 0 | 0.60 |
| Infection | (19,20,22,27) | 7/546 | 2/628 | 2.75 (0.81,
9.33) | 0.11 | 0 | 0.85 |
| Patellar
crepitus | (22,23) | 45/250 | 53/325 | 0.86 (0.61,
1.21) | 0.39 | 0 | 0.55 |
| Knee stiffness | (19,20,22) | 9/372 | 7/454 | 1.56 (0.62,
3.94) | 0.35 | 0 | 0.55 |
Discussion
There has been a great interest in MB prostheses,
due to their assumed reduction in polyethylene wear and component
loosening, in comparison with FB prostheses (32–34).
The current study was designed to determine whether this
theoretical superiority has been translated into improved clinical
outcomes at the mid- to long-term follow-up. The results of this
review demonstrated that there was no significant difference with
respect to clinical, functional or radiological outcomes, or
complication rates between the FB and MB TKA designs. However, the
review has revealed two factors to be considered.
The mean follow-up duration of the trials included
in this study was 5 years, and only two trials (25,31)
had a follow-up duration of >7 years. The expected advantages of
the MB prosthesis, i.e. reduced wear and diminished implant
loosening, may only become apparent following a long period of
time. Therefore, trials with a longer follow-up duration are
required before a definite conclusion may be reached. In addition,
different MB implant designs were used in different trials.
Although all the designs featured polyethylene-bearing mobility,
the MB implants differed according to whether the posterior
cruciate ligament was retained or sacrificed, or whether the
implant was substituted with a different brand. It has been
demonstrated that different types of implant elicit different
effects on the ROM achieved following the TKA (35). It is possible that the variability
amongst the different MB and FB prostheses may have adversely
impacted the accuracy of the conclusion of the present study.
Polyethylene wear was a predominant reason for the
development of MB designs. The aim of the MB design is to reduce
the overall polyethylene wear through increased contact area and
congruency, while minimizing the constraint and maintaining the
normal knee motion. A study conducted by Parks et al
(36) demonstrated that an
undersurface stress existed between the MB undersurface of the
polyethylene and the metal tray that was 40% of the uppersurface
stress, and retrieval studies indicated that the MB inserts had an
improved wear rate in comparison with the FB inserts (0.04 versus
0.07 mm/year, respectively) (37).
However, Kelly et al (38)
demonstrated that the MB surface was damaged to an extent similar
to that of the FB surface, in a study of 48 retrieved MB TKAs. Kim
et al (31) revealed that
there were two cases that were revised due to complete wear of the
polyethylene tibial bearing in the FB cohort; however, no wear rate
was revealed in any of the trials included in the present
study.
As mentioned previously, the MB TKAs may
theoretically prolong the implant survival by reducing shear forces
at the polyethylene interface, reducing contact forces and enabling
the mobility of the bearing surface (39–41).
However, in the current review, the three studies that revealed the
Kaplan-Meier survival estimates did not demonstrate any significant
differences between the MB and FB TKAs at the five-year follow-up.
Certain studies revealed the survivorship for TKA as 91% at 14
years (42) and 92% at 15 years
(43), with repeated surgery for
any reason as the endpoint. Therefore, a sufficiently long-term
follow-up is required in order to evaluate the survivorship of
TKA.
Allocation concealment is one of the most important
biases to minimize when establishing the quality of the evidence.
Since only two of the nine trials clearly described the method of
allocation concealment used, it is possible that allocation bias
occurred in the other trials. The blinding of patients was
accomplished in <50% of trials, and the evidence was
indeterminate, as it related to functional assessment. However, the
blinding of the clinical assessors was performed in the majority of
the studies, which reduced the detection bias. Certain trials did
not reveal important results, which diminished the ability of the
present study to estimate the effectiveness of the treatments. The
interpretation of the results of the studies was limited, as,
according to the criteria for the judgement of the risk of bias,
all the studies were at a high risk of bias.
In conclusion, the results of this meta-analysis
suggest that MB and FB prostheses have no statistically significant
differences in clinical or radiological outcomes, or in
complication rates. In order to perform an improved assessment of
the efficacy of MB implants, well-designed RCTs that compare FB and
MB prostheses, and have a long-term follow-up, are required.
References
|
1.
|
Gandhi R, Dhotar H, Razak F, Tso P, Davey
JR and Mahomed NN: Predicting the longer term outcomes of total
knee arthroplasty. Knee. 17:15–18. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Gioe TJ, Sinner P, Mehle S, Ma W and
Killeen KK: Excellent survival of all-polyethylene tibial
components in a community joint registry. Clin Orthop Relat Res.
464:88–92. 2007.PubMed/NCBI
|
|
3.
|
Ritter MA: The Anatomical Graduated
Component total knee replacement: a long-term evaluation with
20-year survival analysis. J Bone Joint Surg Br. 91:745–749.
2009.PubMed/NCBI
|
|
4.
|
Robertsson O, Bizjajeva S, Fenstad AM, et
al: Knee arthroplasty in Denmark, Norway and Sweden. Acta Orthop.
81:82–89. 2010. View Article : Google Scholar
|
|
5.
|
Spencer SJ, Baird K, Young D and Tait GR:
The Rotaglide mobile bearing knee arthroplasty: A 10- to 13-year
review from an independent centre. Knee. 19:20–23. 2012.PubMed/NCBI
|
|
6.
|
Bottlang M, Erne OK, Lacatusu E, Sommers
MB and Kessler O: A mobile-bearing knee prosthesis can reduce
strain at the proximal tibia. Clin Orthop Relat Res. 447:105–111.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Dennis DA and Komistek RD: Kinematics of
mobile-bearing total knee arthroplasty. Instr Course Lect.
54:207–220. 2005.PubMed/NCBI
|
|
8.
|
Stukenborg-Colsman C, Ostermeier S,
Hurschler C and Wirth CJ: Tibiofemoral contact stress after total
knee arthroplasty: comparison of fixed and mobile-bearing inlay
designs. Acta Orthop Scand. 73:638–646. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Li ZJ, Zhang K and Kim TK: Mobile- and
fixed-bearing total knee arthroplasty for knee osteoarthritis:
Comparisons of early clinical outcomes. Journal of Clinical
Rehabilitative Tissue Engineering Research. 12:9589–9593. 2008.(In
Chinese).
|
|
10.
|
Callaghan JJ, Insall JN, Greenwald AS, et
al: Mobile-bearing knee replacement: concepts and results. Instr
Course Lect. 50:431–449. 2001.PubMed/NCBI
|
|
11.
|
Jacobs WC, Christen B, Wymenga AB, et al:
Functional performance of mobile versus fixed bearing total knee
prostheses: a randomised controlled trial. Knee Surg Sports
Traumatol Arthrosc. 20:1450–1455. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Holinka J, Bahrami N, Lass R, Frantal S,
Windhager R and Wanivenhaus HA: No difference in ROM and knee
function between mobile and floating platforms in TKA. Knee Surg
Sports Traumatol Arthrosc. Jun 29–2012.(Epub ahead of print).
|
|
13.
|
Lampe F, Sufi-Siavach A, Bohlen KE, Hille
E and Dries SP: One year after navigated total knee replacement, no
clinically relevant difference found between fixed bearing and
mobile bearing knee replacement in a double-blind randomized
controlled trial. Open Orthop J. 5:201–208. 2011.
|
|
14.
|
Ball ST, Sanchez HB, Mahoney OM and
Schmalzried TP: Fixed versus rotating platform total knee
arthroplasty: a prospective, randomized, single-blind study. J
Arthroplasty. 26:531–536. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Hanusch B, Lou TN, Warriner G, Hui A and
Gregg P: Functional outcome of PFC Sigma fixed and
rotating-platform total knee arthroplasty. A prospective randomised
controlled trial. Int Orthop. 34:349–354. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Harrington MA, Hopkinson WJ, Hsu P and
Manion L: Fixed-vs mobile-bearing total knee arthroplasty: does it
make a difference? - a prospective randomized study. J
Arthroplasty. 24:24–27. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Matsuda S, Mizu-uchi H, Fukagawa S, et al:
Mobile-bearing prosthesis did not improve mid-term clinical results
of total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc.
18:1311–1316. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Higuchi H, Hatayama K, Shimizu M,
Kobayashi A, Kobayashi T and Takagishi K: Relationship between
joint gap difference and range of motion in total knee
arthroplasty: a prospective randomised study between different
platforms. Int Orthop. 33:997–1000. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Wen Y, Liu D, Huang Y and Li B: A
meta-analysis of the fixed-bearing and mobile-bearing prostheses in
total knee arthroplasty. Arch Orthop Trauma Surg. 131:1341–1350.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Carothers JT, Kim RH, Dennis DA and
Southworth C: Mobile-bearing total knee arthroplasty: a
meta-analysis. J Arthroplasty. 26:537–542. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Smith TO, Ejtehadi F, Nichols R, Davies L,
Donell ST and Hing CB: Clinical and radiological outcomes of fixed-
versus mobile-bearing total knee replacement: a meta-analysis. Knee
Surg Sports Traumatol Arthrosc. 18:325–340. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Oh KJ, Pandher DS, Lee SH, Sung Joon SD Jr
and Lee ST: Meta-analysis comparing outcomes of fixed-bearing and
mobile-bearing prostheses in total knee arthroplasty. J
Arthroplasty. 24:873–884. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Higgins JPT and Green S: Cochrane Handbook
for Systematic Reviews of Interventions Version 510 [updated March
2011]. The Cochrane Collaboration. 2011.Available from https://www.cochrane-handbook.org.
|
|
24.
|
Mahoney OM, Kinsey TL, D’Errico TJ and
Shen J: The John Insall Award: no functional advantage of a mobile
bearing posterior stabilized TKA. Clin Orthop Relat Res. 470:33–44.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Lädermann A, Lübbeke A, Stern R, Riand N
and Fritschy D: Fixed-bearing versus mobile-bearing total knee
arthroplasty: a prospective randomised, clinical and radiological
study with mid-term results at 7 years. Knee. 15:206–210.
2008.PubMed/NCBI
|
|
26.
|
Jolles BM, Grzesiak A, Eudier A, et al: A
randomised controlled clinical trial and gait analysis of fixed-
and mobile-bearing total knee replacements with a five-year
follow-up. J Bone Joint Surg Br. 94:648–655. 2012.PubMed/NCBI
|
|
27.
|
Kalisvaart MM, Pagnano MW, Trousdale RT,
Stuart MJ and Hanssen AD: Randomized clinical trial of
rotating-platform and fixed-bearing total knee arthroplasty: no
clinically detectable differences at five years. J Bone Joint Surg
Am. 94:481–489. 2012.PubMed/NCBI
|
|
28.
|
Kim YH, Kim DY and Kim JS: Simultaneous
mobile- and fixed-bearing total knee replacement in the same
patients. A prospective comparison of mid-term outcomes using a
similar design of prosthesis. J Bone Joint Surg Br. 89:904–910.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
29.
|
Shemshaki H, Dehghani M, Eshaghi MA and
Esfahani MF: Fixed versus mobile weight-bearing prosthesis in total
knee arthroplasty. Knee Surg Sports Traumatol Arthrosc.
20:2519–2527. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
30.
|
Wohlrab D, Hube R, Zeh A and Hein W:
Clinical and radiological results of high flex total knee
arthroplasty: a 5 year follow-up. Arch Orthop Trauma Surg.
129:21–24. 2009.PubMed/NCBI
|
|
31.
|
Kim YH, Kook HK and Kim JS: Comparison of
fixed-bearing and mobile-bearing total knee arthroplasties. Clin
Orthop Relat Res. 392:101–115. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
32.
|
Buechel FF Sr: Long-term followup after
mobile-bearing total knee replacement. Clin Orthop Relat Res.
404:40–50. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
33.
|
Sorrells RB, Stiehl JB and Voorhorst PE:
Midterm results of mobile-bearing total knee arthroplasty in
patients younger than 65 years. Clin Orthop Relat Res. 390:182–189.
2001.PubMed/NCBI
|
|
34.
|
Buechel FF: Mobile-bearing knee
arthroplasty: rotation is our salvation! J Arthroplasty. 19(Suppl
1): 27–30. 2004.PubMed/NCBI
|
|
35.
|
Jacobs WC, Clement DJ and Wymenga AB:
Retention versus sacrifice of the posterior cruciate ligament in
total knee replacement for treatment of osteoarthritis and
rheumatoid arthritis. Cochrane Database Syst Rev. CD0048032005.
|
|
36.
|
Parks NL, Engh GA, Topoleski LD and
Emperado J: The Coventry Award. Modular tibial insert micromotion A
concern with contemporary knee implants. Clin Orthop Relat Res.
356:10–15. 1998.PubMed/NCBI
|
|
37.
|
Berry DJ, Currier JH, Mayor MB and Collier
JP: Knee wear measured in retrievals: a polished tray reduces
insert wear. Clin Orthop Relat Res. 470:1860–1868. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
38.
|
Kelly NH, Fu RH, Wright TM and Padgett DE:
Wear damage in mobile-bearing TKA is as severe as that in
fixed-bearing TKA. Clin Orthop Relat Res. 469:123–130. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
39.
|
Schunck J and Jerosch J: Knee
arthroplasty. Mobile- and fixed-bearing design. Orthopade.
32:477–483. 2003.(In German).
|
|
40.
|
Chouteau J, Lerat JL, Testa R, Moyen B,
Fessy MH and Banks SA: Mobile-bearing insert translational and
rotational kinematics in a PCL-retaining total knee arthroplasty.
Orthop Traumatol Surg Res. 95:254–259. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
41.
|
Vogt JC and Saarbach C: LCS mobile-bearing
total knee replacement. A 10-year’s follow-up study. Orthop
Traumatol Surg Res. 95:177–182. 2009.
|
|
42.
|
Parsch D, Krüger M, Moser MT and Geiger F:
Follow-up of 11-16 years after modular fixed-bearing TKA. Int
Orthop. 33:431–435. 2009.PubMed/NCBI
|
|
43.
|
Roberts VI, Esler CN and Harper WM: A
15-year follow-up study of 4606 primary total knee replacements. J
Bone Joint Surg Br. 89:1452–1456. 2007.PubMed/NCBI
|