Introduction
Tracheomalacia, a condition characterized by
excessive expiratory collapse due to the atrophy and/or reduction
of tracheal elastic fibers of the tracheal wall or a reduction in
the integrity of tracheal cartilage, is a significant cause of
morbidity (1). Softening may occur
in part or all of the tracheal cartilage and may even extend beyond
the trachea (tracheobronchomalacia). Methods for the treatment of
severe tracheomalacia in adults are limited and there is no uniform
standard. Surgical treatments, including stent implantation
(2,3), tracheostomy tube insertion (1) and external tracheal stabilization
(4), have been shown to have a
number of therapeutic effects; however, their use requires careful
consideration on an individual basis and is generally restricted to
patients with localized disease. With regards to medical
treatments, the efficacy of corticosteroids in tracheomalacia has
not been scientifically proven and the use of continuous positive
airway pressure (CPAP) in tracheomalacia is rarely reported
(5,6). The present study reports the
diagnosis of an elderly patient with severe tracheomalacia and the
outcomes of treatment with nasal CPAP combined with implantation of
a temporary Chinese Li’s metallic stent devised by Professor Li
Qiang from The Second Military Medical University (Shanghai, China;
Micro-Tech Co., Ltd., Nanjing, Jiangsu, China).
Case report
This study was carried out in accordance with the
Declaration of Helsinki and approved by the Ethics Committee of
Taizhou People’s Hospital, Jiangsu, China. Written informed consent
was obtained from the patient. The 59-year-old female patient
reported experiences of paroxysmal breathlessness during the
previous 5 years and a history of mild repetitive bronchitis,
occurring 2–3 times a year in the coldest months. Two months prior
to admission, the paroxysmal breathlessness, cough and
expectoration had started to occur more frequently, despite
treatment with salbutamol sulfate aerosol (Ventolin, 200 μg four
times daily), salmeterol/fluticasone (50/500 μg twice daily) and
oral moxifloxacin (0.4 g once daily.) As a result of the persistent
dyspnea, the patient had a limited ability to carry out normal
daily activities. Following admission, physical examinations
revealed a body temperature of 37.9ºC, a pulse of 113 beats per
min, a respiratory rate of 28 breaths per min and a blood pressure
of 140/94 mmHg. The patient exhibited an exhausted appearance and
cyanosis of the lips. Respiratory movements and vocal fremitus were
equal bilaterally. Expiratory wheezing was heard throughout both
lungs and no moist rales were noted. The patient had a regular
heart rhythm and no edema was observed in the lower
extremities.
A complete blood test revealed a white cell count of
11.59×109/l and a large white blood cell ratio
(percentage of white blood cells that are neutrophils) of 71.2%. A
blood gas analysis demonstrated a pH of 7.35, 68 mmHg
PaO2, 60 mmHg PaCO2 and 31 mmol/l
HCO3− (performed during oxygen inhalation at
a low flow rate). A lung function test indicated severe obstructive
ventilation disorder with a FEV1/FVC ratio of 37%. Chest
radiography showed signs consistent with chronic obstructive
pulmonary disease (COPD) and chest computed tomography (CT)
demonstrated evident stenosis of the tracheal lumen at the end of
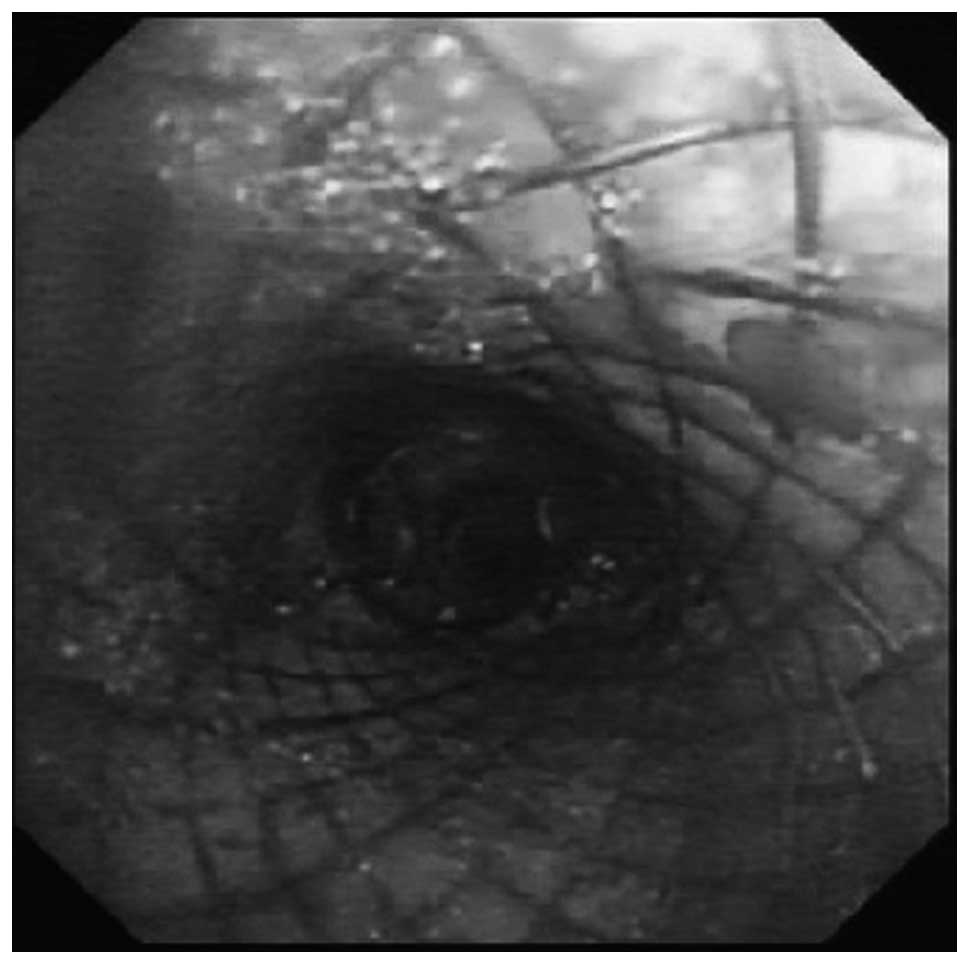
expiration (Fig. 1). Bronchoscopy
revealed a widening of the membranous part of the trachea, folds,
significant airway collapse at the end of expiration and a 91%
reduction in the cross-sectional area of the tracheal lumen
(Fig. 2).
The patient was diagnosed with adult tracheomalacia
and nasal CPAP was administered to improve ventilation. This was
combined with antibiotics (intravenous moxifloxacin, 0.4 g once
daily), inhaled medication for asthma (budesonide, 4 mg twice
daily) and mucolytics (intravenous ambroxol hydrochloride, 120 mg
once daily). During CPAP, the pressure level was initially set at 8
cm H2O and was then increased in 1 cm H2O
increments until a level associated with clinical alleviation of
the stridor, the greatest reduction in breathing rate and an
increase in SaO2 was identified. The optimal pressure
level for this patient was 12 cm H2O. Symptoms,
including cough, expectoration, fever and dyspnea, were improved by
day 4 following admission and episodes of wheezing and stridor
occurred less frequently. On day 16, the patient had improved
substantially and was discharged.
Following discharge, the patient was treated with
nasal CPAP, the level of which was regulated down to 10 cm
H2O. For the subsequent 3 months, the patient reported
feeling healthy and had an increased level of activity; however,
attempts to discontinue the nasal CPAP were accompanied by a marked
increase in respiratory distress.
Four months following the initiation of nasal CPAP,
breathlessness recurred in the patient and was refractory to an
increase in CPAP to 13 cm H2O. The patient was
readmitted to hospital and a temporary Chinese Li’s metallic stent
was implanted using flexible bronchoscopy. The stent was positioned
6 cm below the vocal cords and 2 cm above the eminence, markedly
opening the trachea (Fig. 3).
Chest radiography confirmed that the positioning and
expansion of the metallic stent were successful (Fig. 4). The patient was also administered
nasal CPAP, combined with antibiotics (intravenous moxifloxacin,
0.4 g once daily), inhaled medication for asthma (budesonide, 4 mg
twice daily) and mucolytics. Respiratory symptoms, including
dyspnea, breathlessness, expectoration and fever, were
significantly improved in the patient following placement of the
stent.
Three weeks following surgery, the metallic stent
was removed since the patient exhibited a marked improvement in
breathlessness. Episodes of stridor and respiratory distress were
not aggravated by intervention with nasal CPAP combined with
salmeterol/fluticasone (50/500 μg twice daily, respectively) and
the patient was discharged.
Discussion
Adult tracheomalacia may be classified into
congenital (for example, Mounier-Kuhn syndrome) or acquired forms,
including those resulting from chest trauma, tracheostomy,
inflammation, chronic irritation, malignancy or mechanical
anatomical factors. Softening may affect either part or all of the
tracheal cartilage, and may even extend beyond the trachea
(tracheobronchomalacia). Although previous studies have shown that
adult tracheomalacia occurs in elderly patients and is
significantly associated with COPD and smoking, the implications of
the coexistence of COPD and tracheomalacia are not fully
understood, and the pathological progression of COPD to
tracheomalacia has not been clearly demonstrated (5,7).
Since it is difficult to differentiate between tracheomalacia and
COPD, we were unable to confirm which of the conditions occurred
first in the patient.
Although the techniques and criteria for the
diagnosis of tracheomalacia are not standardized, thorax CT and
bronchoscopy are the preferred methods in previously published
studies (8–10). With regards to the degree of airway
stenosis, a collapse of <50% is within normal limits, 50–75% is
mild, 75–90% is moderate and 91–100% (close proximity of the
posterior membrane to the anterior luminal surface) is considered
to indicate severe malacia (3).
Tracheomalacia patients have no overt symptoms during the initial
stages; however, as the disease progresses, they are likely to
present with shortness of breath, cough, sputum and other
obstructive and infectious symptoms of the respiratory tract. In
particular, inspiratory stridor is the distinctive symptom. With
increasing levels of awareness and improved diagnosis of the
disease, the incidence of reported tracheomalacia has increased
significantly (1). Asymptomatic
patients require close observation without treatment, and there is
no uniform standard treatment for patients with the severe form of
the disease. Generally, patients are treated on an individual
basis. The efficacy of corticosteroids for the treatment of
tracheomalacia has not been scientifically proven. Surgical
treatments, including stent implantation (2,3),
tracheostomy tube insertion (1)
and the external tracheal stabilization technique (4), are generally restricted to patients
with localized disease and thus require careful consideration.
CPAP is relatively simple to use, non-invasive and
has few side-effects. It exerts its therapeutic effects by
increasing tidal volume, which reduces airway collapse and reduces
respiratory effort. Consequently, CPAP is the preferred method of
treatment in previously published studies (1). There is no uniform standard for
adjusting CPAP ventilation to the optimal level. Ferguson and
Benoist (6) evaluated expiratory
airflow and airway collapse during the acute administration of
nasal CPAP in three tracheobronchomalacia patients for whom
conventional medical management had failed. It was observed that
FVC increased and dynamic airway collapse decreased with increasing
levels of CPAP. Davis et al(11) reported that the optimal level of
CPAP in infants with severe tracheomalacia may be achieved by
increasing the lung volume to a level at which the infant is not
flow-limited during tidal breathing, without simultaneously
increasing the effort of breathing by reducing pulmonary
compliance. In the present study, the procedure was initiated with
the adjustment of CPAP ventilation to the optimal level. The
pressure level was initially set at 8 cm H2O and was
then progressively increased in 1 cm H2O increments and
set at a level associated with the clinical alleviation of the
stridor, the greatest fall in breathing rate and an increase in
SaO2. As the procedure has the advantages of rapid
evaluation, simple operation, low cost and being non-invasive, it
was preferred by the doctors in the Department of Respiratory
Medicine, Taizhou People’s Hospital (Taizhou, China) and acceptable
to the patient.
To the best of our knowledge, there has been no
comparative study between CPAP and bilevel positive airway pressure
(BIPAP) in the treatment of adult tracheomalacia. Essouri et
al(12) reported that
non-invasive ventilation using CPAP and BIPAP is associated with a
significant and comparable reduction in respiratory effort in
infants with severe upper airway obstruction. CPAP ventilation
remains the preferred mode over BIPAP, since the inspiratory and
expiratory trigger sensitivity of BIPAP mode ventilation is
insufficient in patients with a high respiratory rate or small
tidal volume, resulting in patient-ventilator asynchrony.
In our experience, a nasal mask is preferable to an
oronasal mask for the following reasons: i) Nasal masks are smaller
and associated with a reduction in dead space; ii) certain
side-effects, including abdominal distention resulting from an
ingression of gas to the gastrointestinal tract, are alleviated;
iii) the nasal mask is well tolerated and there is reduced gas
leakage, particularly in elderly patients with facial bone
malformation. Furthermore, since patients may be dependent on CPAP
for an extended duration following the diagnosis of tracheomalacia,
custom-made nasal masks designed according to the facial bones of
the patient may be beneficial.
Intratracheal stent implantation has been used in
the treatment of adult tracheomalacia since 1965, primarily in
severe cases where traditional treatments have failed (13,14,15).
Intratracheal stents are divided into two major types: silicone
stents and shape-memory alloy stents. Silicone stents are easily
implanted and removed, but have complications including infection,
expectoration and the tendency to undergo migration. Furthermore,
they require a high-cost surgery involving rigid bronchoscopy and
general anesthesia (16). The
above-mentioned limitations of silicone stents are overcome by
shape-memory alloy stents; however, the use of these in benign
airway stenosis is controversial since they are known to be
associated with complications, including restenosis, the excessive
growth of granulation tissue and stent migration (17). To the best of our knowledge, airway
infection is one of the factors leading to the aggravation of adult
tracheomalacia and is difficult to control in a short period of
time. Chinese Li’s metallic stents not only have the advantages of
traditional memory-alloy stents, but may also be adjusted and
removed before the hyperplasia of granulation tissue occurs
(usually at 3 weeks) due to the unique design of a double recycling
line at both ends of the stent. This time-effective advantage
allows the earlier application of traditional treatments, including
CPAP respiratory support, anti-infection and asthma treatment,
which improves the success rate of clinical rescue.
In conclusion, severe adult tracheomalacia is a
dangerous disease that is challenging to manage, particularly at
the time of airway infection, and has a high mortality rate
(8). Nasal CPAP combined with the
implantation of a temporary Chinese Li’s metallic stent may be an
effective treatment for temporarily alleviating symptoms of the
disease.
References
|
1
|
Carden KA, Boiselle PM, Waltz DA and Ernst
A: Tracheomalacia and tracheobronchomalacia in children and adults:
an in-depth review. Chest. 127:984–1005. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Thornton RH, Gordon RL, Kerlan RK, et al:
Outcomes of tracheobronchial stent placement for benign disease.
Radiology. 240:273–282. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ernst A, Majid A, Feller-Kopman D, et al:
Airway stabilization with silicone stents for treating adult
tracheobronchomalacia: a prospective observational study. Chest.
132:609–616. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cho JH, Kim H and Kim J: External tracheal
stabilization technique for acquired tracheomalacia using a
tailored silicone tube. Ann Thorac Surg. 94:1356–1358. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kandaswamy C and Balasubramanian V: Review
of adult tracheomalacia and its relationship with chronic
obstructive pulmonary disease. Curr Opin Pulm Med. 15:113–119.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ferguson GT and Benoist J: Nasal
continuous positive airway pressure in the treatment of
tracheobronchomalacia. Am Rev Respir Dis. 147:457–461. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Murgu SD and Colt HG: Treatment of adult
tracheobronchomalacia and excessive dynamic airway collapse : an
update. Treat Respir Med. 5:103–115. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jiang A and Lu H: Early diagnosis and
management of tracheomalacia with invasive bronchopulmonary
aspergillosis in an adult. Braz J Infect Dis. 16:215–216. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gilkeson RC, Ciancibello LM, Hejal RB,
Montenegro HD and Lange P: Tracheobronchomalacia: dynamic airway
evaluation with multidetector CT. AJR Am J Roentgenol. 176:205–210.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Aquino SL, Shepard JA, Ginns LC, et al:
Acquired tracheomalacia: detection by expiratory CT scan. J Comput
Assist Tomogr. 25:394–399. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Davis S, Jones M, Kisling J, Angelicchio C
and Tepper RS: Effect of continuous positive airway pressure on
forced expiratory flows in infants with tracheomalacia. Am J Respir
Crit Care Med. 158:148–152. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Essouri S, Nicot F, Clément A, et al:
Noninvasive positive pressure ventilation in infants with upper
airway obstruction: comparison of continuous and bilevel positive
pressure. Intensive Care Med. 31:574–580. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sommer D and Forte V: Advances in the
management of major airway collapse: the use of airway stents.
Otolaryngol Clin North Am. 33:163–177. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Casiano RR, Numa WA and Nurko YJ: Efficacy
of transoral intraluminal Wallstents for tracheal stenosis or
tracheomalacia. Laryngoscope. 110:1607–1612. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ernst A, Odell DD, Michaud G, Majid A,
Herth FF and Gangadharan SP: Central airway stabilization for
tracheobronchomalacia improves quality of life in patients with
COPD. Chest. 140:1162–1168. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Murgu SD and Colt HG: Complications of
silicone stent insertion in patients with expiratory central airway
collapse. Ann Thorac Surg. 84:1870–1877. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chen W and Ruan Y: Late complications of
nickel-titanium alloy stent in tracheal stenosis. Laryngoscope.
122:817–820. 2012. View Article : Google Scholar : PubMed/NCBI
|