Introduction
Early elevated intraocular pressure (IOP) following
pars plana vitrectomy frequently complicates vitreoretinal surgery.
Ultrasound biomicroscopy (UBM) is a non-invasive diagnostic
procedure, developed in order to achieve superior visualization of
the anterior segment of the eye. The aim of this study was to
investigate the mechanism of IOP elevation following pars plana
vitrectomy. The ultrasound biomicroscope is an imaging instrument
used in clinical opthalmology that was developed by Palvin in 1990
for use in clinical ophthalmology research (1). Not only does it enable the anterior
segment to be clearly visualized during surgery, it also provides
quantitative measurements, which are an important basis for the
analysis of certain physiological eye processes and the
pathological mechanisms of certain eye diseases. With the
advantages of being non-contact, non-invasive and non-interfering,
UBM is considered to be a superior imaging detection technique for
studies regarding anterior segment morphology (2,3). A
previous study concerning the mechanisms and risk factors of high
IOP in posterior vitreous resectioning neglected the observation of
the anterior chamber angle structure, which is closely associated
with glaucoma (4). Comparison of
the pre- and postsurgical anterior segment structure angle may help
to explain certain mechanisms involved in the increase of IOP, and
further provides a theoretical clinical basis.
Subjects and methods
Subjects
From January 2009 to January 2011, 119 patients (132
eyes) who underwent a posterior vitrectomy at Tianjin First Center
Hospital (Tianjin, China) experienced early postoperative ocular
hypertension. With an average age of 46.5 years, there were 66
males (75 eyes) and 53 females (57 eyes) aged between 19 and 72
years. In all the patients who had undergone posterior vitrectomy,
the possibility of various primary eye diseases, such as primary or
secondary glaucoma, a medical history of ocular hypertension or a
family history of glaucoma, were excluded. This study was conducted
in accordance with the Declaration of Helsinki, and with the
approval of the Ethics Committee of Tianjin First Center Hospital.
Written informed consent was obtained from all participants.
General patient information
The clinical data of the patients were gathered for
retrospective analysis, including general patient characteristics.
In 132 eyes, there were 43 eyes with diabetic retinopathy (DR) and
vitreous hemorrhaging; 24 eyes with DR and tractional retinal
detachment (RD); 32 eyes with RD and proliferative
vitreoretinopathy (PVR) above grade C2; 10 eyes with RD and PVR
less than grade C2; three eyes with traumatic RD; five eyes with
traumatic vitreous hemorrhaging; five eyes with branch retinal vein
occlusion caused by vitreous hemorrhaging; five eyes with
unexplained vitreous hemorrhaging; three eyes with a macular film
and two eyes that exhibited vitreous opacity.
Treatment
All patients were treated with a standard 3-channel
closed vitrectomy. According to the condition of the eye, combined
phacoemulsification and intraocular lens surgery, stripping
surgery, gas-liquid exchange surgery, heavy water injection surgery
or laser photocoagulation was selected. Similarly, the type and
concentration of padding or filler was selected. The measurement of
IOP was conducted using a Schiotz tonometer (Akihito Medical
Devices Co., Ltd. Suzhou, China) at the end of the surgery, and the
IOP was controlled within the range of 5.5/12.0−7.0 mmHg. All
patients accepted a pre- and postsurgical eye examination,
including corrected visual acuity, slit lamp, IOP, gonioscopy,
ophthalmoscopy and UBM examination. Generally, following surgery,
the patients accepted the UBM review within three to seven days,
and gonioscopy was required for patients with elevated IOP. We used
a P40 Type ultrasound biomicroscope, produced by the Zeiss-Paradigm
Company (Hong Kong, China), with a probe frequency of 50 MHz and a
scan depth and width of 5 mm. Using the incidental functions of
distance and angle measurements (3), we used the UBM instrument in a 12, 3,
6 and 9 o’clock radial scan and saved the captured images of the
four quadrants. The main measurement parameters included: i) the
depth of the anterior chamber; ii) the thickness of the ciliary
body; iii) the angle opening distance 500 (AOD500); iv) the angle
between the sclera and the ciliary body; and v) the distance
between the trabecular meshwork and the ciliary body.
Statistical analysis
Statistical data were presented as the mean ± SD.
The data were analyzed using SPSS 14.0 software (SPSS, Inc.,
Chicago, IL, USA) with a t-test to determine whether two groups
were statistically different. P<0.05 was considered to indicate
a statistically significant difference.
Results
Slit lamp and ophthalmoscopy
Of 50 eyes with early postoperative elevated IOP,
there were 32 eyes that exhibited eyelid swelling, 26 eyes with
corneal edema, 31 eyes with an inflammatory reaction, nine eyes
with anterior chamber hemorrhaging and eleven eyes with bloody
sediment attached to the corneal wall. In addition, there were four
eyes with silicone oil in the anterior chamber, three eyes in which
a fibrous membrane had formed at the pupil, two eyes which held an
intraocular lens, three eyes that had a barrier of bubbles in the
pupil area and two eyes that exhibited partial anterior
synechia.
Gonioscopy
Of the 132 eyes in which the angle of the anterior
chamber of the eye was preoperatively observed by angle gonioscopy,
85 had a wide-angle and 47 had an NI angle. Iris morphology was
normal in all eyes. No neovascularization was observed in the
anterior chamber angle. Postsurgical examination findings within
two weeks of surgery were the same those from the preoperative
examination.
UBM
This study compared differences between various
measurement parameters pre- and postoperatively in a phakic group
and an intraocular lens group (65 and 54 patients, repectively).
Due to the low number of cases, an aphakic group was not included
in the statistical analysis. In the phakic group, the postoperative
anterior chamber depth of the eyes with elevated IOP was
significantly different from that in the eyes with a normal IOP
(t=2.000, P=0.049). Moreover, the difference between the pre- and
postoperative measurements of anterior chamber depth also differed
significantly between the elevated and normal IOP groups (t=2.534,
P=0.042). In summary, we considered that the postsurgical anterior
chamber depth was reduced compared with that preoperatively in the
phakic group. Furthermore, the difference in the postoperative
AOD500 between the eyes with elevated IOP and those with normal IOP
in the phakic group was considered to be statistically significant
(t=2.069, P=0.050). Similarly, the difference between the pre- and
postoperative measurements of the AOD500 also differed
significantly between the elevated and normal IOP groups (t=2.073,
P=0.047). The AOD500 is a parameter which reflects the degree of
angle width; therefore, the AOD following surgery was markedly
reduced in the phakic group with elevated IOP. In our study, in a
pre- and postoperative comparison of the distance between the
ciliary body and the trabecular meshwork and the angle between the
sclera and the ciliary body, no statistically significant
differences were identified between the patients with elevated IOP
and those with normal IOP (P>0.05).
However, in the intraocular lens group, the
postoperative anterior chamber depth of the eyes with elevated IOP
was observed to be statistically significantly different from that
of the eyes with normal IOP (t=2.066, P=0.050), but the difference
between the pre- and postoperative anterior chamber depth
measurements was not shown to differ significantly between the
elevated and normal IOP groups (t=0.212, P=0.834). This may be
explained by the small size of the intraocular lens compared with
the phakic lens and the deeper postoperative anterior chamber depth
compared with that preoperatively. Using the t-test, other
parameters, such as the AOD500, the distance between the ciliary
body and the trabecular meshwork and the angle between the sclera
and the ciliary body were not considered to be statistically
significant (P>0.05). The difference in the postoperative
measurements of ciliary body thickness between the eyes with
elevated IOP and those with normal IOP was considered to be
statistically significant (t=1.926, P=0.037), but the difference
between the pre- and postoperative measurements of the thickness of
the ciliary body were not considered to differ significantly
according to IOP status (t=1.094, P=0.279). Therefore, it is not
possible to conclude that the thickness of the ciliary body
increases in patients with elevated IOP following surgery.
Discussion
With advances in technology, pars plana vitrectomy
has become an important treatment for ocular posterior segment
disease. However, high IOP is a common clinical complication, which
may occur at any time following surgery but is most common after
one or two weeks. According to previous studies, the mechanism for
early postoperative high IOP following the pathogenesis of
vitrectomy includes open-angle and angle-closure mechanisms.
Open-angle mechanisms include: intraocular expansion by gas
injection, inflammatory substances blocking the trabecular
meshwork, silicone oil glaucoma and ghost cell glaucoma.
Close-angle mechanisms include: pupillary blocking, ciliary body
edema and anterior synechia (5).
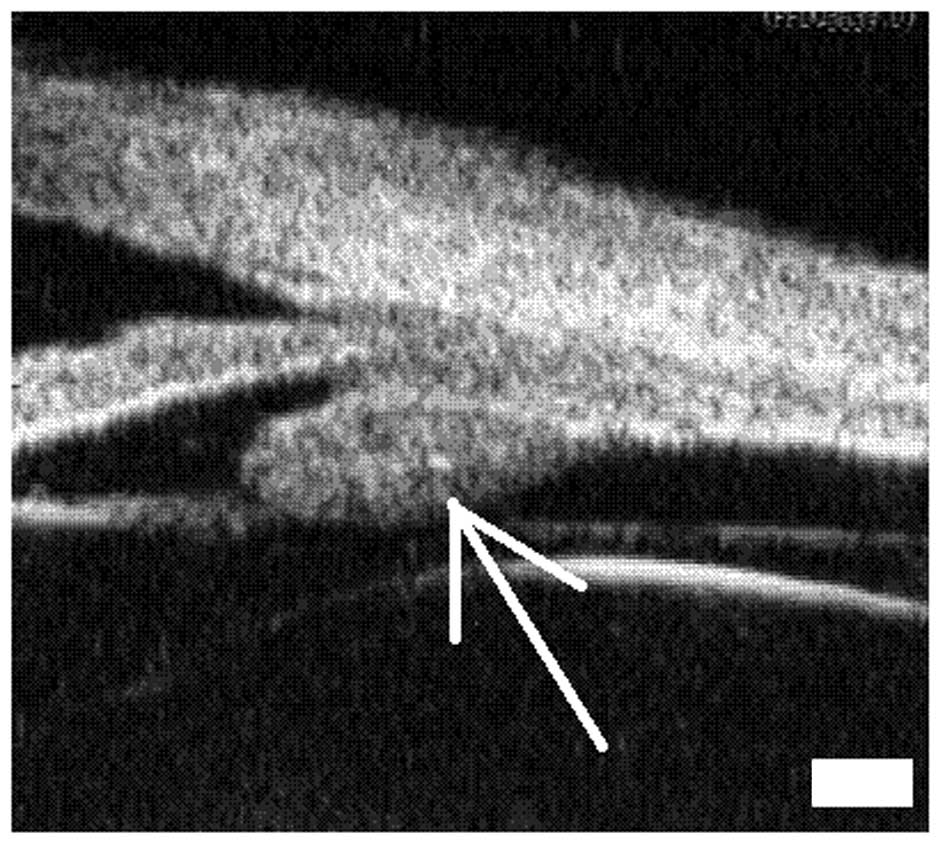
By the use of UBM, the current study established
that there were 16 eyes (12.12%) in the high IOP group in which
ciliary body detachment (full 360º) had occurred (Fig. 1). According to a previous study
(6), following surgery, a
wide-ranging detachment of the ciliary body, edema of the ciliary
body, and forward rotation of ciliary processes may create pressure
on the peripheral iris, causing it to move to the trabecular
meshwork, leading to angle closure, and an increase in the IOP.
Furthermore, when the ciliary body is detached, the ciliary body
and choroidal liquid push on the ciliary body and the suspensory
ligament, which causes the lens to move forward and the anterior
chamber to become shallower. In the current study, three eyes in
the elevated IOP group exhibited edema of the ciliary body. The
swollen ciliary processes had rotated forward to the root of the
iris and accumulated in the gap between the iris root and the
equitorial lens region, which had moved forward (Fig. 2). Clinically, in certain cases the
reduction of IOP was due to surgical trauma where a large area of
condensation and the secretion of aqueous humor was affected by the
ciliary membrane. Due to a reduction in the IOP, the liquid rapidly
accumulated in the suprachoroidal space, which caused the
detachment of the choroid. Therefore, choroidal detachment further
aggravated hypotony and an inflammatory reaction exacerbated this
cycle.
Furthermore, the vorticose veins were pressed on
during surgery, which blocked the drainage of ciliary body venous
blood, resulting in ciliary body edema. This resulted in the
swollen ciliary processes reversing forward, so that the peripheral
iris pressed against the trabecular meshwork, which aggravated the
closed angle and caused an increase in the IOP. Anterior chamber
hemorrhaging blocked the peripheral iridotomy opening holes, which
in turn blocked the flow of aqueous humor in the anterior and
posterior chambers. In addition, aqueous humor accumulated in the
posterior chamber, which caused intravitreal silicone oil to
protrude into the pupil area, resulting in the formation of a pupil
block (Fig. 3), and thereby the
occurrence of elevated IOP (7).
Azzolini et al(8)
considered that silicone oil droplets may display a strong
reflection ring, and floating and emulsified silicone oil droplets
were due to the lack of a reflection ring. Due to their light
weight, silicone emulsion droplets were able to float up and move
closer to the cornea; therefore, floating, small, highly reflective
and clear-cut drops of silicone oil were observed in the anterior
chamber. When moving closer to cornea, the silicone oil droplets
may be observed as solidified matter in the corneal endothelium
(9). In the current study, there
were two eyes in the high IOP group with secondary surgery in which
emulsified silicone oil droplets were visible on the iris surface
under the slit lamp prior to surgery. UBM examination revealed fine
oil droplets attached to the corneal endothelium, and indicated
that the angle of the anterior chamber had opened (Fig. 4). Therefore, the emulsified
silicone oil droplets and phagocytic macrophages blocked the
trabecular meshwork, which led to an increase in the IOP (10).
According to the comparison between the eyes with
high IOP and those with normal IOP in the phakic group, the
anterior chamber depth became shallower and the AOD reduced
following surgery; however, it is not possible to conclude that
early postoperative elevated IOP has a direct relationship with
this condition. In the intraocular lens group, every preoperative
and postoperative measurement parameter exhibited no significant
change, which may be related to the fact that the thickness of the
human lens is 4.0 mm, while the thickness of an intraocular lens is
only 0.8 mm. Combined with phacoemulsification and intraocular lens
implantation, the anterior chamber depth is likely to increase
following surgery.
In conclusion, the mechanism of early postoperative
elevated IOP following vitrectomy is complicated. This study
identified that the possible mechanism of early postoperative
ocular hypertension by UBM comprises the following: postoperative
edema of ciliary body; the anterior chamber becomes shallower and
is rotated forward; and the increase in IOP is caused by angle
narrowing. Every measurement parameter suggested that the AOD
decreased and the anterior chamber became shallower in the phakic
IOP group following surgery.
References
|
1
|
Pavlin CJ, Sherar MD and Foster FS:
Subsurface ultrasound microscopic imaging of the intact eye.
Ophthalmology. 97:244–250. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pavlin CJ, Harasiewicz K, Sherar MD and
Foster FS: Clinical use of ultrasound biomicroscopy. Ophthalmology.
98:287–295. 1991. View Article : Google Scholar
|
|
3
|
Lei L, WenLi Y and Wenbin W: Ocular
Ultrasound Biomicroscopy. Diagnostics Beijing Science and
Technology Press; Beijing: pp. 43–44. 2002
|
|
4
|
Henderer JD, Budenz DL, Flynn HW Jr, et
al: Elevated intraocular pressure and hypotony following silicone
oil retinal tamponade for complex retinal detachment: incidence and
risk factors. Arch Ophthalmol. 117:189–195. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Xiaoxin L and Jingzhao W: Vitreoretinal
Surgery Study. 2. 1st edition. Bei Jing, BJ: pp. 48–49. 2000
|
|
6
|
Massicotte EC and Schuman JS: Malignant
glaucoma-like syndrome following pars plana vitrectomy.
Ophthalmology. 106:1375–1379. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ruby AT, Grand MG, Williams D and Thomas
MA: Intraoperative acetazolamide in the prevention of intraocular
pressure rise after pars plana vitrectomy with fluid-gas exchange.
Retina. 19:185–187. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Azzolini C, Pierro L, Codenotti M,
Bandello F and Brancato R: Ultrasound biomicroscopy following the
intraocular use of silicone oil. Int Ophthalmol. 19:191–195. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ru Xia C: Ultrasound biomicroscopy in
vitreoretinal disease diagnosis. Ophthalmic Research. 21:100–102.
2003.
|
|
10
|
Su Yan L, Wenji W and Qin Ruan C: After
silicone oil tamponade glaucoma and angle changes. Ophthalmol.
17:105–107. 2001.
|