Introduction
Cervical spondylotic myelopathy (CSM) is a cervical
degenerative disease with a prognosis that is correlated with the
cervical disc degeneration, the degree of spinal cord compression
and the age of the patient (1,2). The
prognosis of the disease is not optimistic and the occurrence of a
gradual deterioration with time is high. To date, the pathogenesis
of CSM has not been fully elucidated, although the major
compression theory suggests that the symptoms of CSM are associated
with the stenosis of the spinal canal and the degree of spinal cord
compression (3). However, the
extent of the compression does not fully explain the clinical
symptoms of the spinal cord injury.
VB12 deficiency has been observed to lead
to the development of degenerative diseases of the nervous system,
including the peripheral and central nervous systems, and there
have been numerous studies on subacute combined degeneration of the
spinal cord resulting from VB12 deficiency (4). However, to date, there have been no
studies concerning a VB12 deficiency occurring in
combination with CSM, to the best of our knowledge. This case
report describes two cases of CSM observed in the clinic, where the
patients also presented with VB12 deficiency. This study
was approved by the ethics committee of Huashan Affiliated Hospital
of Fudan University (Shanghai, China). Informed consent was
obtained from all patients.
Case report
Case one
A 68-year-old male was admitted to the clinic. The
patient had a history of a fall two weeks prior to the admission to
the clinic, although no direct external force had been applied to
the head and neck during the fall. The patient complained of
numbness in the forearms and hands, tingling sensations and a lack
of power when clenching the fists. Through the physical
examination, it was observed that the flexion and extension range
of the patient’s body and neck were normal and that there was no
sign of tenderness. The flexion and extension strength of the
patient’s elbow muscle was of Grade III, there was numbness and
hyperalgesia in the bilateral forearm and hand, the grip of the
patient’s two hands was weak, the bilateral Hoffmann sign was (+)
and the lower extremity muscle strength was graded as Class IV.
Furthermore, the muscle tone was normal, the tendon reflex was
(+++), the patellar clonus was (−) and the ankle clonus was (−).
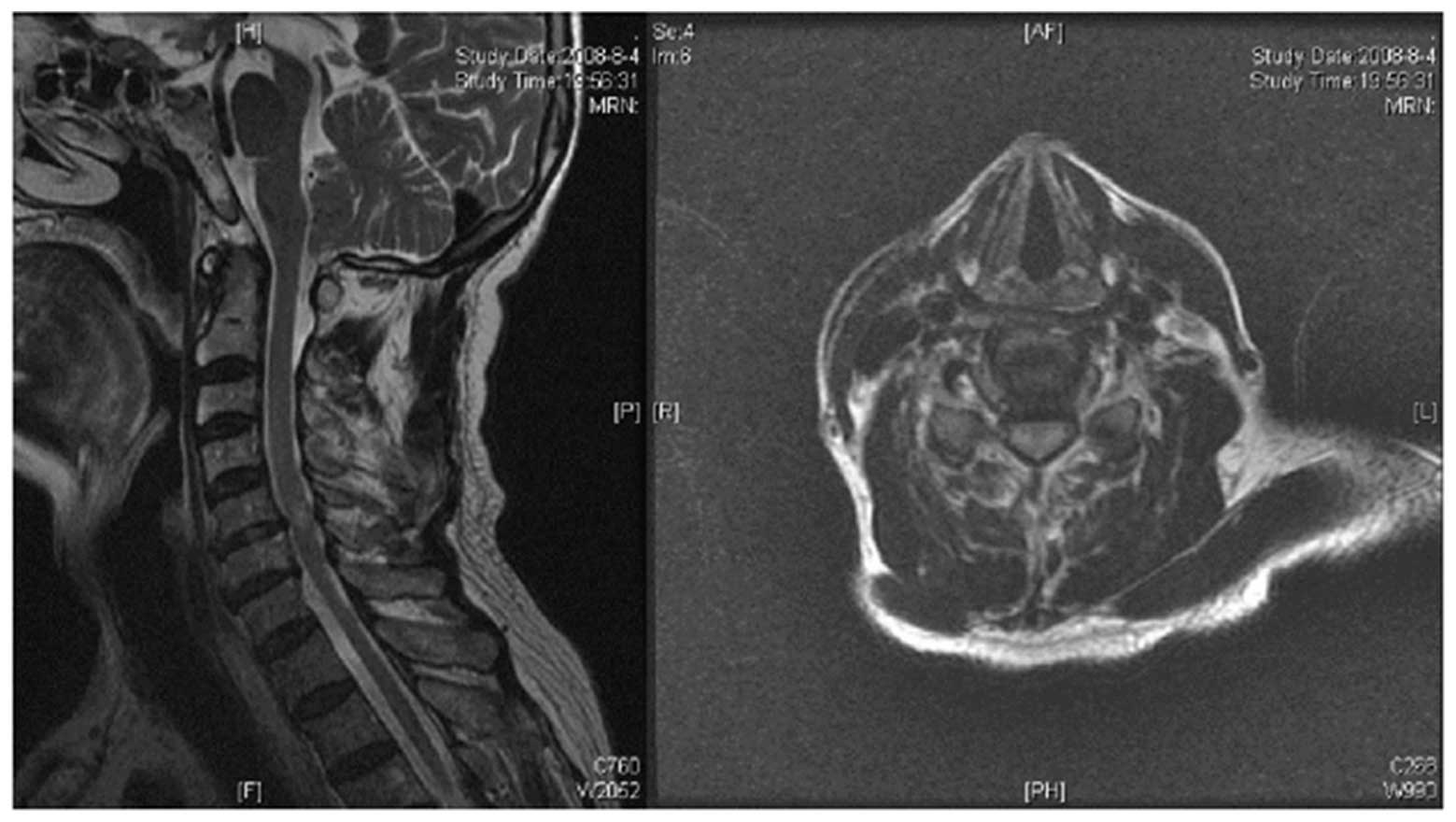
Cervical magnetic resonance imaging (MRI) examination revealed that
cervical disc degeneration was apparent at C5–6 level with backward
extrusion, and that there were high signal changes within the same
level of the spinal cord. Mild dural compression was observed in
the cross section (Fig. 1).
According to the study by Nagata et al (5), the degree of spinal cord compression
may be classified into one of four groups: Level 0, no pressure on
the spinal cord; Level 1, mild compression on the spinal cord;
Level 2, the degree of spinal cord compression is <1/3; Level 3,
the degree of spinal cord compression is >1/3.
In this case, the degree of spinal cord compression
on the MRI imaging was classed as Level 1, i.e. only mild
compression; however, T2-weighted (T2W) MRI examination revealed
that there were high signal changes in the spinal cord. Therefore,
although the clinical manifestations and symptoms indicated damage
to the central beam of the spinal cord, this was not consistent
with the mild degree of compression. Laboratory examinations
revealed that the level of serum VB12 was 173 pg/l,
which was below the normal range (211–946 pg/l). It is possible
that VB12 deficiency may be the cause of spinal cord
injury in this patient in whom there is only a mild degree of
spinal cord compression.
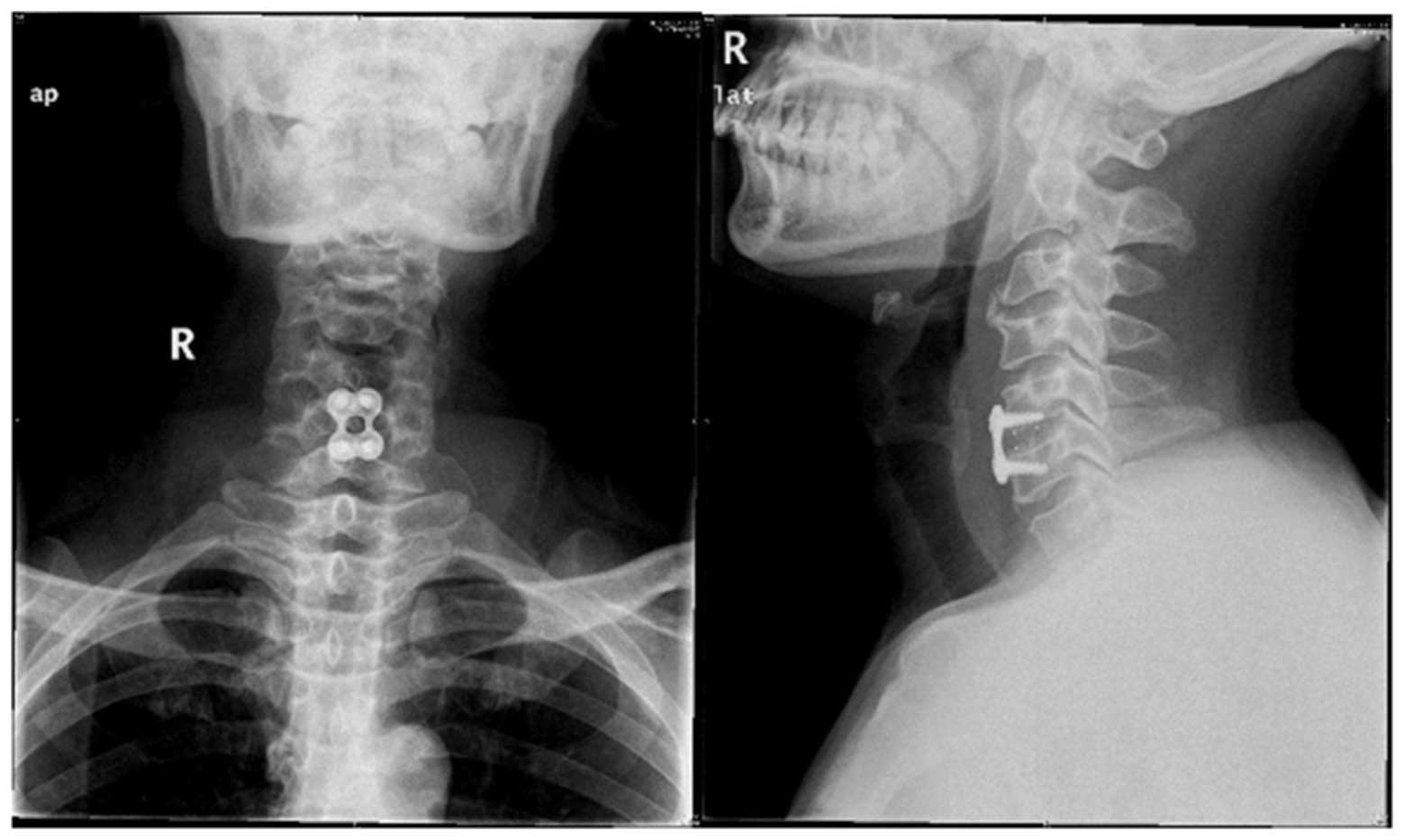
The patient underwent anterior cervical
decompression-fusion and internal fixation (Fig. 2), at the same time as receiving
three months of oral VB12 replacement therapy. One week
later, the tingling feeling in the patient’s hands was
significantly improved and his fist-clenching ability was restored
and two weeks later the patient’s muscle strength reached Grade
III; three months subsequently, the numb feeling in the forearms
and hands of the patient had almost disappeared, the patient’s
finger activities had returned to normal and the fist muscle
strength had recovered to Class IV.
Case two
A 61-year-old male was admitted to the clinic with
numb upper limbs, feelings of weakness and an unstable gait that
had been apparent for more than one month. The patient complained
of a sense of strapping in his chest and an inability to grip with
his hands or hold objects without dropping them. Furthermore, the
patient had weak fine finger movements, such as writing, and felt
his walking was like walking on cotton. Physical examination
revealed normal neck and bilateral shrug activities, Grade IV
flexion and extension strength of the elbow muscle, numbness in the
bilateral forearms and hands and weak fist-clenching abilities. The
bilateral Hoffmann sign was (+), the lower extremity muscle
strength was of Grade IV, the muscle tension was high and the
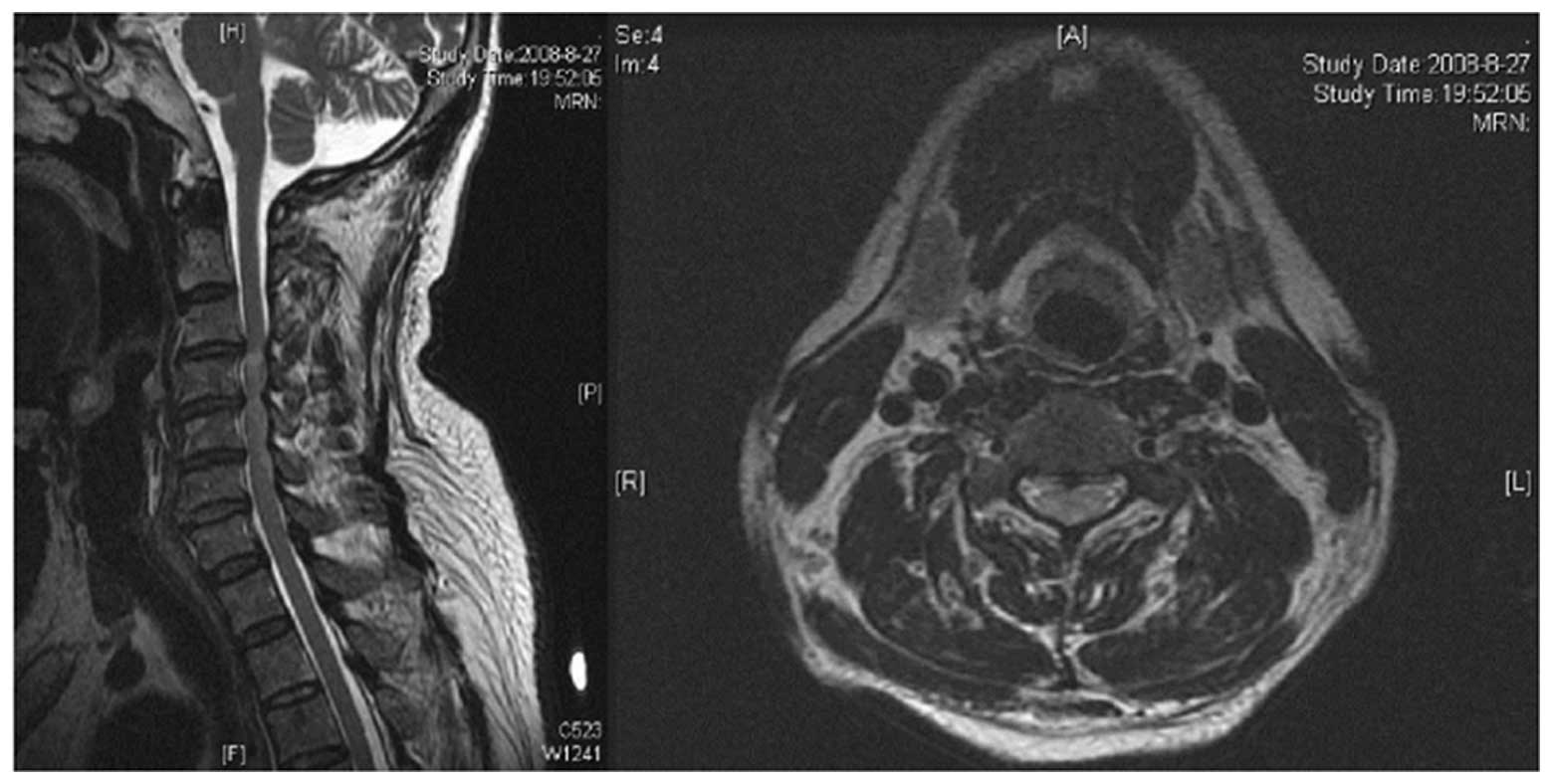
tendon hyperreflexia was (++++). The cervical MRI revealed high
signal changes at the C3–4 level in the spinal cord and slipped
discs were observed at C3–4 and C4–5 (Fig. 3).
The MRI examination indicated that the compression
at the C3–4 level of the patient’s spinal cord was of Level 2,
according to the Nagata grading, and T2W MRI revealed high signal
changes within the same level of the spinal cord. In addition, the
patient exhibited symptoms typical of motor neuron injury in CSM.
Laboratory tests measured that the level of serum VB12
was 182 pg/l, which was below the normal range (211–946 pg/l).
Although the spinal cord compression was not serious, there were
high signal changes in the intramedullary spinal cord that were
apparent with T2W MRI, and the clinical manifestations were typical
of spinal cord injury. The VB12 deficiency of the
patient may have been the factor leading to the spinal cord
damage.
Similar to the patient in case one, the patient in
the present case underwent anterior decompression-fusion and
internal fixation and, following three months of VB12
replacement therapy, the balance of the patient when walking
improved markedly and the sense of strapping in the chest
disappeared, although the numbness of upper limbs was still
apparent. Furthermore, the fist action of the patient recovered and
muscle strength was measured to be Grade III.
Discussion
CSM is one of the main types of cervical
degenerative disease, with clinical manifestations that are
indicative of spinal cord compression. The development of CSM is
normally slow and insidious, making early diagnosis and treatment a
challenge. By the time it is posssible for a clear clinical
diagnosis to be made, the condition of the patients has often
deteriorated beyond the point when treatment is most efficacious
(6).
The pathogenesis of CSM is not fully understood,
although its incidence is correlated with the volume of the spinal
canal, the degree of disc degeneration and spinal cord compression
(7). Mechanical compression is
considered the primary factor leading to the functional injury of
the spinal cord; however, the compression theory alone is not able
to explain all the clinical manifestations. It has been suggested
that the apolipoprotein E allele increases the chances of CSM
developing in patients under long-term spinal cord compression
(8). Histological examinations of
the pathological changes in patients with CSM have demonstrated
mildly atrophic white matter, reductions in the number of neurons
and pale medullary sheaths in the lateral and posterior cord
(9).
It has often been observed in the clinic that
certain CSM patients with a severe slipped disc and spinal cord
compression on imaging do not have a spinal cord injury in the area
of the clinical manifestations, while others exhibit a mild slipped
disc and mild spinal cord compression on imaging, yet have a severe
spinal cord injury in the area of the clinical manifestations. The
degree of spinal cord compression on imaging and the clinical
spinal cord injury performance are, therefore, not always
consistent. This led to the consideration of whether there were
other factors affecting the ability of the spinal cord to bear
mechanical pressure.
VB12 is an indispensable catalyst of
nucleic acid synthesis and protein metabolism in cells in
vivo; at present, VB12 deficiency is a common
disease (10,11). VB12 deficiency leads to
a wide range of neuropathies, of which subacute combined
degeneration of the spinal cord is particularly common. Neural
changes caused by VB12 deficiency may be correlated with
subcortical dysfunction and neuronal metabolism changes (12). Dalla Torre et al described
two cases of isolated sensory axon neuropathy resulting from
VB12 deficiency, and suggested that there was a
requirement for serum VB12 levels to be detected for
distal symmetric neuropathy (13).
There have been rare studies on the role of VB12 in
cervical spinal cord diseases and it is used as a conventional
neurotrophic drug; however, there have been no studies concerning
the effects of VB12 on the pathogenesis of spinal cord
disease.
The two cases described in this study had the same
characteristics, such as a shorter duration of time before
occurrence of typical symptoms, and the clinical manifestations of
typical CSM symptoms, including unsteady gait, a sense of strapping
in the chest, numb hands, reduced fist muscle strength and
pathological signs, such as the Hoffmann sign (+). The patients
were not receiving oral VB12 treatment. MRI examinations
revealed that the degree of spinal cord compression was not severe
at Levels 1–2, although high signal changes on T2W MRI were
observed within the spinal cord. Laboratory tests revealed that the
serum VB12 levels were below the normal range, classing
the patients as having a VB12 deficiency, which may have
been one of the factors leading to the cervical spinal cord
disease. Following anterior cervical decompression-fusion and
internal fixation and VB12 replacement therapy, the
clinical symptoms of the two patients significantly improved.
At present, there is still a lack of investigation
into the role of VB12 in the pathogenesis of CSM. The
two cases in the present study indicated that the detection of the
VB12 levels of patients who do not exhibit serious
spinal cord compression on imaging may be helpful in explaining the
disease. Further studies to investigate the incidence of
VB12 deficiency in patients with cervical myelopathy may
be of value.
In conclusion, the two cases described in the
present study suggested that the incidence of CSM may be correlated
with VB12 deficiency, particularly for cases in which
the clinical manifestations and the imaging do not fully match. In
cases such as these, it may be beneficial to check serum
VB12 levels.
References
|
1.
|
Naderi S, Ozgen S, Pamir MN, Ozek MM and
Erzen C: Cervical spondylotic myelopathy: surgical results and
factors affecting prognosis. Neurosurgery. 43:43–49. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Holly LT, Matz PG, Anderson PA, et al:
Clinical prognostic indicators of surgical outcome in cervical
spondylotic myelopathy. J Neurosurg Spine. 11:112–118. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Levine DN: Pathogenesis of cervical
spondylotic myelopathy. J Neurol Neurosurg Psychiatry. 62:334–340.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Lee GR: Pernicious anemia and other causes
of vitamin B12(cobalamin) deficiency. Wintrobe’s
Clinical Hematology. Lee GR, Foerster J, Lukens J, Paraskevas F,
Greer JP and Rodgers GM: 10th edition. Lippincott Williams and
Wilkins; Baltimore, MD: pp. 941–964. 1999
|
|
5.
|
Nagata K, Kiyonaga K, Ohashi T, et al:
Clinical value of magnetic resonance imaging for cervical
myelopathy. Spine (Phila Pa 1976). 15:1088–1096. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Baron EM and Young WF: Cervical
spondylotic myelopathy: a brief review of its pathophysiology,
clinical course, and diagnosis. Neurosurgery. 60(Suppl 1): S35–S41.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Tracy JA and Bartleson JD: Cervical
spondylotic myelopathy. Neurologist. 16:176–187. 2010. View Article : Google Scholar
|
|
8.
|
Setzer M, Hermann E, Seifert V and
Marquadt G: Apolipoprotein E gene polymorphism and the risk of
cervical myelopathy in patients with chronic spinal cord
compression. Spine (Phila Pa 1976). 33:497–502. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Ito T, Oyanagi K, Takahashi H, et al:
Cervical spondylotic myelopathy. Clinicopathologic study on the
progression pattern and thin myelinated fibers of the lesions of
seven patients examined during complete autopsy. Spine (Phila Pa
1976). 21:827–833. 1996. View Article : Google Scholar
|
|
10.
|
Clarke R, Grimley Evans J, Schneede J, et
al: Vitamin B12 and folate deficiency in later life. Age Ageing.
33:34–41. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Andrès E, Loukili NH, Noel E, et al:
Vitamin B12 (cobalamin) deficiency in elderly patients. CMAJ.
171:251–259. 2004.
|
|
12.
|
Kalita J, Agarwal R, Chandra S and Misra
UK: A study of neurobehavioral, clinical psychometric, and P3
changes in vitamin B12 deficiency neurological syndrome. Nutr
Neurosci. 16:39–46. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Dalla Torre C, Lucchetta M, Cacciavillani
M, Campagnolo M, Manara R and Briani C: Reversible isolated sensory
axonal neuropathy due to cobalamin deficiency. Muscle Nerve.
45:428–430. 2012.PubMed/NCBI
|