Introduction
Bladder paraganglioma (pheochromocytoma) is rare,
accounting for <0.05% of all bladder tumors and ∼10% of
extra-adrenal paragangliomas (1).
Hematuria and the symptoms induced by micturition or defecation due
to an excess of catecholamines, including hypertension,
palpitations and headache, are typical clinical findings in
patients with bladder paragangliomas. Computed tomography (CT) and
magnetic resonance imaging (MRI) may provide specific
characteristic signs for the diagnosis of paraganglioma (2–4),
particularly in cases where patients lack the typical symptoms.
However, bladder paraganglioma is not considered as the primary
pre-operative diagnosis for patients with bladder neoplasm, and
these unsuspected paragangliomas greatly increase the peroperative
mortality rate in patients undergoing even relatively minor
surgical procedures (5). In the
present study, a case of unsuspected bladder paraganglioma is
reported, in which characteristic signs of the condition were
exhibited on CT images, and a severe hypertensive episode occurred
during cystoscopic tumor resection. The study was approved by the
ethics committee of West China Hospital of Sichuan University,
Chengdu, China. Written informed consent was obtained from the
patient.
Case report
A 26-year-old male patient was admitted to West
China Hospital of Sichuan University on August 15, 2012 with a
history of a bladder tumor and microscopic hematuria. The lesion
was found 2 years before by abdominal ultrasonography (USG) and the
size of the tumor was stable from then until 4 months prior to
admission, when the tumor began to enlarge. Physical examination of
the patient did not reveal any unusual findings; the blood pressure
of the patient was 93/63 mmHg on admission and results of the
urinalysis were normal. An abdominal CT examination was performed
using a Philips Brilliance 64-slice CT scanner (Philips Medical
Systems, Eindhoven, The Netherlands) with a slice thickness of 6
mm. This revealed a 26×22×25 mm nodular lesion originating from the
right bladder trigone region, protruding into the bladder cavity.
The tumor showed homogeneous soft-tissue attenuation [mean CT
value, 40 Hounsfield units (HU)] on a plain CT scan, the density of
which was slightly lower than that of the internal obturator
muscles. The lesion exhibited intense enhancement (mean CT value,
129 HU) in the arterial phase, which was significantly higher than
that of the bladder wall and only slightly lower than that of the
right femoral artery. Thickening of the bladder wall near the tumor
was not observed (Fig. 1). The
primary radiological and clinical diagnosis was bladder carcinoma
with no suspicion of extra-adrenal paraganglioma.
Following the preoperative examinations, an elective
cystoscopic tumor resection was performed on August 17, 2012.
During the surgery, the tumor was found in the trigone region of
the bladder. The tumor had a pedicle, smooth surface, edema mucosa
and varicose veins. On attempted surgical removal of a small part
of the tumor, the blood pressure of the patient suddenly increased
to 210/120 mmHg and the heart rate reached 145 bpm. The operative
procedure was immediately terminated, and the blood pressure and
heart rate gradually returned to normal over 10 min. Subsequently,
an intraoperative biopsy using frozen sections indicated the
presence of paraganglioma.
Following surgery, the history of the patient was
reviewed and it was noted that the patient had a history of
post-micturition syncope. One day after the surgery, the erect and
supine aldosterone levels of the patient were 15.51 ng/dl (normal,
9.8–27.5 ng/dl) and 17.57 ng/dl (normal, 4.5–17.5 ng/dl),
respectively), and the plasma renin levels were 1.59 ng/ml/h
(normal, 0.56–2.79 ng/ml/h) and 1.65 ng/ml/h (normal, 0.05–0.8
ng/ml/h), respectively. Four days after the surgery, the plasma
norepinephrine and epinephrine levels were 345 ng/l (normal,
272–559 ng/l) and 91 ng/l (normal, 54–122 ng/l), respectively. A
partial cystectomy with complete extirpation was performed on
August 28, 2012. During the second surgery, no episodes of
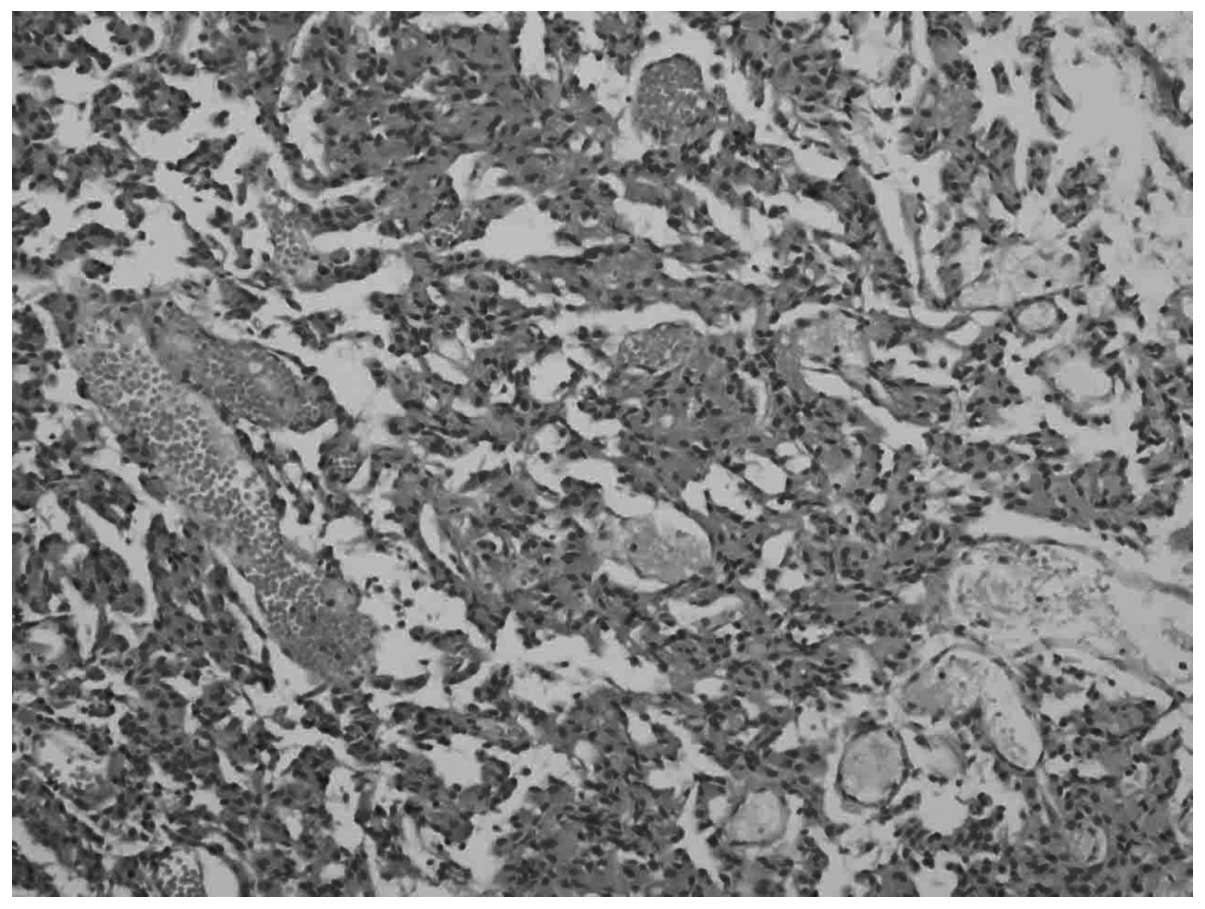
hypertension occurred. Convalescence was uneventful. Histological
examination confirmed bladder paraganglioma (Fig. 2).
Discussion
Bladder paragangliomas may occur in patients of any
age, but typically occur between the ages of thirty and fifty
(6). They are usually submucosal
or intramural with intact vesical epithelium and, consistent with
the present case, are commonly detected in the trigone region
(7).
The most common feature of bladder paraganglioma is
a characteristic clinical picture resulting from a hypertensive
crisis that may be accompanied by headache, palpitations, hot
flushes and sweating. These crises are typically provoked by
micturition or overdistention of the bladder. The classical triad
of episodic hypertension, persistent hematuria and post-micturition
syncope is almost diagnostic, but is extremely rare (8). In the present case, painless
hematuria was the primary clinical symptom. This is common in
bladder disease and therefore does not specifically indicate the
presence of bladder paraganglioma. Symptoms resulting from
hypertensive crises did not present in this case, with the
exception of a history of post-micturition syncope. Although this
is a virtually diagnostic symptom, it is often missed when the
history of the patient is initially taken, as occurred in this
case.
The imaging modalities for the diagnosis of bladder
paraganglioma include USG, CT, MRI and meta-iodobenzylguanidine
(MIBG) scintigraphy (3,4). The characteristic signs of bladder
paragangliomas in CT and MRI images are as follows: i) The tumor is
nodular or a mass with homogeneous or heterogeneous density/signal;
ii) the lesion often originates from the bladder trigone and seldom
from the anterior or lateral wall, with well-defined borders; and
iii) the lesion appears mostly as soft-tissue attenuation on a
plain CT scan (2,3) with a slightly higher signal intensity
than that of the gluteal muscle on pre-enhanced T1-weighted imaging
(T1WI), and hyperintensity is observed compared with the gluteal
muscle on T2WI. Unlike adrenal paraganglioma, bladder paraganglioma
does not exhibit the characteristic ‘light bulb bright signal’ in
T2WI (2,4). Studies using CT and MRI report
significant enhancement of tumors following contrast injection
(2–4). Epithelial tumor is the main disease
for differential diagnosis of the bladder paraganglioma, and has
been described to have a similar or reduced density compared with
that of the bladder wall on enhanced scans (9). Epithelial tumors also tend to be more
infiltrative and are associated with thickening of the adjacent
bladder wall contiguous with the mass. By contrast, paragangliomas
are extremely vascular and consequently exhibit greater enhancement
than that of the urinary bladder wall. They also tend to be more
localized (10). Although these
characteristic signs of bladder paraganglioma were exhibited in the
present case, clinical misdiagnosis occurred prior to the
operation, leading to an intraoperative hypertensive crisis. Two
explanations may account for this clinical misdiagnosis. Firstly,
typical clinical signs, with the exception of microscopic
hematuria, were not observed in this patient. The history of
post-micturition syncope was not revealed at the initial visit.
Secondly, the radiologist did not raise the possibility of bladder
paraganglioma. The localized tumor with significant enhancement on
contrast enhanced CT images should prompt the radiologist to
consider bladder paraganglioma and subsequently warn surgeons to
prepare for an intraoperative hypertensive crisis. Therefore, the
current case highlights important points to be considered upon
diagnosis. Firstly, it is important to record a thorough history of
patients with bladder tumors, and in particular, to screen for a
history of hypertensive episodes. Secondly, in the case of
localized bladder tumors with significantly higher enhancement than
that of the bladder wall on the CT image, the possible diagnosis of
bladder paraganglioma should be raised in order to ensure that
surgeons and anesthesiologists are prepared for an intraoperative
hypertensive crisis.
References
|
1.
|
Dahm P and Gschwend JE: Malignant
non-urothelial neoplasms of the urinary bladder: a review. Eur
Urol. 44:672–681. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Vahidi K, Joe BN, Meng M, Coakley FV and
Yeh BM: Review of atypical pelvic masses on CT and MRI: expanding
the differential diagnosis. Clin Imaging. 31:406–413. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Vyas S, Kalra N, Singh SK, Agarwal MM,
Mandal AK and Khandelwal N: Pheochromocytoma of urinary bladder.
Indian J Nephrol. 21:198–200. 2011. View Article : Google Scholar
|
|
4.
|
Wang H, Ye H, Guo A, et al: Bladder
paraganglioma in adults: MR appearance in four patients. Eur J
Radiol. 80:e217–e220. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Pahwa HS, Kumar A, Srivastava R and Rai A:
Unsuspected pheochromocytoma of the urinary bladder: reminder of an
important clinical lesson. BMJ Case Rep. Aug 8–2012. View Article : Google Scholar
|
|
6.
|
Sharma PK, Sharma P and Saraswat B: Extra
adrenal pheochromocytoma of urinary bladder. Indian J Surg.
70:188–191. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Ansari MS, Goel A, Goel S, Durairajan LN
and Seth A: Malignant paraganglioma of the urinary bladder. A case
report. Int Urol Nephrol. 33:343–345. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Goyal S, Puri T, Gunabushanam G, Das AK
and Julka PK: Skeletal metastases from recurrent paraganglioma of
the urinary bladder. Indian J Urol. 21:122–124. 2005. View Article : Google Scholar
|
|
9.
|
Husband J: Staging of bladder and prostate
cancer. Computed Tomography of the Pelvis. Walsh JW: Churchill
Livingstone; New York: pp. 135–162. 1985
|
|
10.
|
Athyal RP, Al-Khawari H, Arun N, Abul F
and Patrick J: Urinary bladder paraganglioma in a case of von
Hippel-Lindau disease. Australas Radiol. 51:B67–B70. 2007.
View Article : Google Scholar : PubMed/NCBI
|