Introduction
Gastric cancer is one of the most common causes of
mortality due to cancer in China (1). Surgery is the standard treatment
procedure for localized and resectable gastric cancer. However, the
survival rate of patients with advanced gastric cancer after
surgery remains low. Decreasing the recurrence rates and extending
the life span of patients suffering from gastric cancer has been
the focus of a number of clinical investigations, with one study
showing that chemotherapy may improve the survival rates of
patients with gastric cancer postoperatively; however, the
effectiveness was limited (2).
Therefore, considerable efforts are required to improve the current
therapeutic modalities and to explore novel therapies. In recent
years, adoptive immunotherapy has been generally used in clinical
practice. A number of adoptive immuno-therapies with killer cells
have been developed, including tumor infiltrating lymphocyte (TIL),
dendritic cell (DC) and cytokine-induced killer (CIK) cell
therapies. At present, CIK cells are a novel type of antitumor
effector cell that have been demonstrated to proliferate rapidly
in vitro, with a stronger antitumor activity and a broader
target tumor spectrum than the alternative antitumor effector cells
that have been investigated (3,4).
Moreover, CIK cells are able to regulate and enhance immune
function (5).
In the present study, the potential benefits of the
combination of autologous CIK cells with FOLFOX4 were investigated
in patients suffering from gastric cancer and were compared with
the effects of chemotherapy alone.
Subjects and methods
Clinical data
A total of 98 patients with gastric cancer who were
treated surgically in The First Affiliated Hospital of Zhengzhou
University (Zhengzhou, China) from June 2010 to June 2012 were
enrolled in this study. The patients received a gastroscopy and a
barium meal examination prior to the surgery. The 98 patients with
gastric cancer were divided into two groups following the surgery:
The control group (47 patients) were treated with FOLFOX4 alone,
while the observation group (51 patients) were treated with FOLFOX4
in combination with CIK cell immunotherapy. The characteristics of
the patients, such as gender, age, pathological grade, tumor site,
histological type, invasion depth, lymph node metastasis and tumor
stage, were collected and evaluated. The control group comprised 31
males and 16 females, aged from 35 to 76 years with a median age of
55.2±12.7 years. The cancer characteristics of the patients in the
control group were as follows: pathological grade, 12 prophase and
35 aggressive phase; tumor site, 9 gastric fundus cardia, 20
gastric corpus and 18 gastric antrum; histological type, 21
moderately well-differentiated adenocarcinoma and 26 poorly
differentiated adenocarcinoma; invasion depth, 24 with serosa
infiltration and 23 without serosa infiltration; lymph node
metastasis, 25 lymphaden transfer; and tumor stage, 6 stage I, 19
stage II, 18 stage III and 4 stage IV. The observation group
comprised 34 males and 17 females, aged from 33 to 78 years with a
median age of 56.1±11.9 years. The cancer characteristics of the
patients in the observation group were as follows: pathological
grade, 14 prophase and 37 aggressive phase; tumor site, 8 gastric
fundus cardia, 23 gastric corpus and 20 gastric antrum;
histological type, 21 moderately well-differentiated adenocarcinoma
and 30 poorly differentiated adenocarcinoma; invasion depth, 23
with serosa infiltration and 28 without serosa infiltration; lymph
node metastasis, 30 lymphaden transfer; tumor stage, 8 stage I, 20
stage II, 16 stage III and 7 stage IV. No statistical differences
were identified between the two groups with regard to the gender
and age of the patients, or the pathological grade, tumor site,
histological type, invasion depth, lymph node metastasis or tumor
stage (P>0.05). The study was conducted in accordance with the
Declaration of Helsinki and with approval from the Ethics Committee
of the First Affiliated Hospital of Zhengzhou University. Written
informed consent was obtained from all participants.
Treatments
Patients in the control group underwent two cycles
of chemotherapy with the protocol of FOLFOX4 [oxaliplatin (L-OHP)
85 mg/m2, 3 h on day 1; calcium folinate (CF) 200
mg/m2, 2 h on days 1 and 2; and 5-fluorouracil (5-Fu)
400 mg/m2, 22 h on days 1 and 2]. One cycle comprised 14
days. All the patients in the two groups were treated with a 5-HT
receptor blocker and vitamin B6 prior to therapy.
Appropriate treatments were administered if the numbers of
peripheral blood leucocytes or platelets, or the hemoglobin levels
of the patients appeared to descend.
Patients in the observation group received CIK cell
immunotherapy following two cycles of chemotherapy. All the
patients underwent a routine blood examination after blood
collection. A total of 50 ml blood was drawn from each patient
using sodium citrate as an anticoagulant. Peripheral blood
mononuclear cells (PBMCs) were isolated using hydroxypropylmethyl
cellulose and were subsequently cultured in Medium I containing
RPMI-1640 in the presence of human interferon-γ (IFN-γ,
1.0×106 U/l), recombinant human interleukin-1α (IL-1α,
100 U/ml) and human IL-2 (5.0×105 U/l). A monoclonal
antibody (MAb) against CD3 (50 ng/ml) was added following 24 h of
culture. The supernatant was aspirated and the cells were cultured
in Medium II in the absence of INF-γ following a further 48 h
culture. The cells were then cultured for 15 days and the medium
was changed every 2 days. CIK cells (1.0×109) were
transfused into the patients for 1 h every second day. The curative
efficacy was evaluated subsequent to each treatment. The cells were
identified and sorted by flow cytometry using a
fluorescence-activated cell sorter (FACS; Beckman-Coulter, Miami,
FL, USA) on days 1, 5, 10, 15, and 20. In addition, the whole blood
cells of the patients were separated and sorted by FACS prior to
and following treatment.
Evaluation
The patients were followed up from June 2010 to June
2012, and were assessed every 3 months for the first year, then
every 6 months for the second and third years. The immune functions
[CD3, CD4, CD8, CD4/CD8 and natural killer (NK) cells], cumulative
recurrence rates, cumulative survival rates and the survival times
of the two groups were analyzed prior to and following
treatment.
Statistical analysis
Statistical analysis was performed using SPSS
version 3.0 statistical software (SPSS, Inc., Chicago, IL, USA).
All values are expressed as the mean ± standard deviation.
Comparisons were made using the Student’s t-test or the
χ2 test. The cumulative recurrence and survival curves
were estimated using the Kaplan-Meier method and the differences in
the distributions were compared with the log-rank test. P<0.05
was considered to indicate a statistically significant
difference.
Results
Analysis of CIK cell phenotype
CD3+ CD56+ CIK cells were
induced from the PBMCs of the patients following stimulation by
INF-γ, IL-1α, IL-2 and anti-CD3 MAb. The number of CIK cells
gradually increased the during cell culture, peaking on day 15 and
then decreasing slightly with further culture (Fig 1).
Comparison of the immune function of the
patients prior to and following treatment
No statistical differences were observed in the
levels of CD3+, CD4+, CD8+,
CD4+/CD8+ and NK cells between the two groups
prior to treatment (P>0.05). Moreover, there were no
statistically significant differences between the levels of
CD3+, CD4+, CD8+,
CD4+/CD8+ and NK cells in the control group
prior to and following treatment (P>0.05). However, the levels
of CD3+, CD4+, CD8+,
CD4+/CD8+ and NK cells in the observation
group following treatment were markedly higher than those prior to
treatment and were also significantly enhanced compared with the
levels in the control group following treatment, and the level of
CD8+ in the observation group following treatment was markedly
lower than those prior to treatment (P<0.05; Table I).
 | Table I.Phenotypic analysis of
cytokine-induced killer cells of the control and observation groups
pretherapy and 10 days post-therapy. |
Table I.
Phenotypic analysis of
cytokine-induced killer cells of the control and observation groups
pretherapy and 10 days post-therapy.
| Group | n | CD3+
(%) | CD4+
(%) | CD8+
(%) |
CD4+/CD8+ (%) | NK cells (%) |
|---|
| Control | | | | | | |
| Pretherapy | 47 | 57.04±10.23 | 28.99±8.14 | 25.79±6.41 | 0.96±0.31 | 17.89±5.89 |
| Post-therapy | 47 | 55.39±8.90 | 18.16±8.54 | 26.39±7.01 | 1.02±0.26 | 18.14±6.01 |
| Observation | | | | | | |
| Pretherapy | 51 | 57.21±9.44 | 29.54±7.82 | 26.32±6.48 | 1.06±0.25 | 18.23±6.12 |
| Post-therapy | 51 |
66.75±9.81ab |
38.12±8.02ab |
19.62±5.92ab |
1.37±0.29ab |
26.11±6.48ab |
Comparison of the recurrence rates of the
two groups
There were 23 postoperative recurrences in the
control group, and 12 in the observation group. The log-rank test
demonstrated that the gastric cancer recurrence rates of the
patients in the observation group were significantly lower than
those of the patients in the control group (5.9 versus 25.5, 17.6
versus 36.2 and 23.5 versus 48.9% for the observation and control
groups following 1, 2 and 3 years, respectively; P<0.05;
Fig. 2).
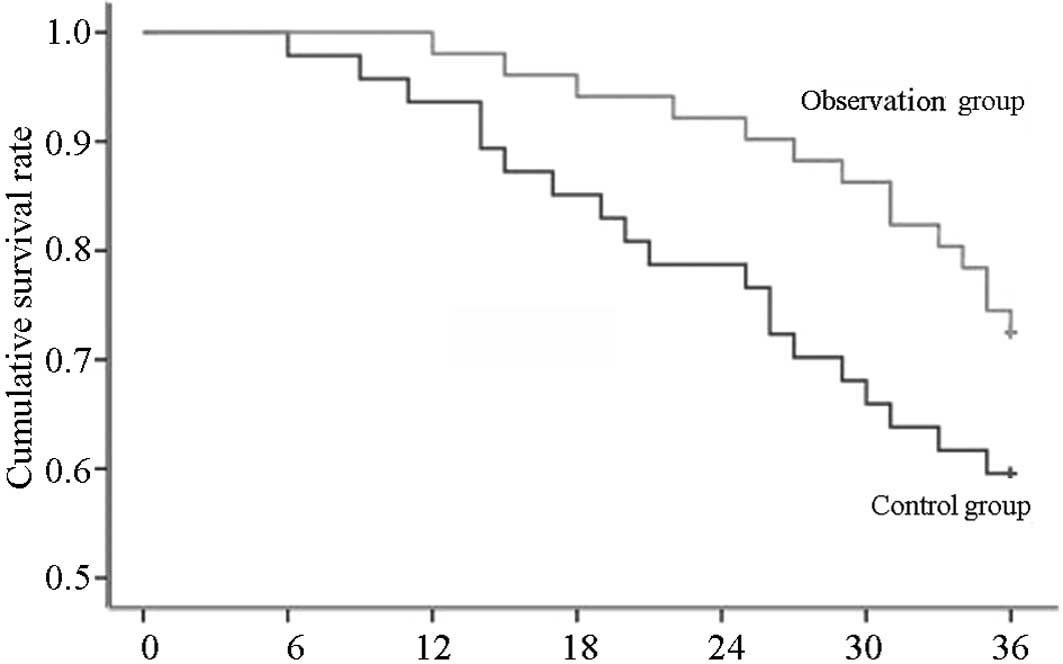
Comparison of the survival rates of the
two groups
In the observation group, there were 19 fatalities
and the average survival time was 21 months, while in the control
group, there were 11 fatalities and the average survival time was
29 months. The survival rates of the patients with gastric cancer
in the observation group were demonstrated to be significantly
enhanced in comparison with those in the control group following
analysis with a log-rank test (98.0 versus 93.6, 92.2 versus 78.7
and 72.5 versus 59.6% after 1, 2 and 3 years, respectively;
P<0.05; Fig. 3).
Discussion
Despite the standardization of surgery and
multimodal therapies, the postoperative survival of patients with
advanced gastric cancer remains poor. Previous studies have shown
that the recurrence rates are 2–14% in early gastric cancer, more
than 50% in advanced gastric carcinoma and ∼30% in the patients
with a 5-year survival (6,7). It has been demonstrated that adjuvant
chemotherapy for gastric cancer following curative resection may
improve the disease-free and overall survival times of patients
with gastric cancer. However, numerous cycles of chemotherapy may
lead to a reduction in the immune functions of the patients with
gastric cancer, with decreased ratios of CD4+ and
CD4+/CD8+ cells, reduced NK cell activities
and an increased proportion of CD8+ cells (8). These observations are consistent with
those of the present study. Therefore, novel therapies that
significantly improve the immune functions of patients with cancer
are required.
In recent years, immunotherapy has become the fourth
most important treatment modality for malignant tumors (9). It has been shown that cellular
immunotherapy is able to promote host anticancer immunity, thus
prolonging the survival time of patients with gastric cancer. The
treatment of gastric cancer with autologous CIK cells is one such
promising cellular immunotherapy (9–12).
It has been demonstrated that CIK cells proliferate abundantly
in vitro and kill tumor cells directly. Moreover, CIK cells
are able to regulate and increase the host cellular immune function
in vivo (13–16). The results of the present study
suggest that CIK cell immunotherapy is able to significantly
improve the immune functions of patients with cancer, showing that
the proportions of the CD3+ and CD4+ T-cell
subgroups were significantly increased, the activities of the NK
cells were enhanced, the proportion of CD8+ cells was
markedly decreased and the ratio of CD4+/CD8+
cells was normal following CIK cell immunotherapy.
The current study also investigated the effects of
CIK cell treatment combined with FOLFOX4 on the recurrence and
survival rates of the patients with gastric cancer. The results
showed that in years 1, 2 and 3, for the control group, the
cumulative recurrence rates were 25.5, 36.2 and 48.9%, respectively
and the survival rates were 93.6, 78.7 and 59.6% respectively,
while for the observation group, the recurrence rates were 5.9,
17.6 and 23.5%, respectively and the survival rates were 98.0, 92.2
and 72.5%, respectively. It was observed that the recurrence rates
of the observation group were lower compared with those of the
control group, whereas the survival rates of the observation group
were higher than those of the control group. The results suggested
that CIK cell immunotherapy combined with chemotherapy may have a
synergistic effect.
In conclusion, adjuvant immunotherapy with CIK cells
significantly reduced the recurrence rate and prolonged the
survival time of patients with gastric cancer. Furthermore, the
treatment with CIK cells combined with FOLFOX4 demonstrated notable
efficacy in improving the immune function of the patients.
References
|
1.
|
Dong S, Li FQ, Zhang Q, Lv KZ, Yang HL,
Gao Y and Yu JR: Expression and clinical significance of SHP2 in
gastric cancer. J Int Med Res. 40:2083–2089. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Martella B, Cardin F, Lorenzetti R,
Terranova C, Amato B and Militello C: Local recurrence of gastric
cancer after total gastrectomy: an unusual presentation. BMC Surg.
12(Suppl 1): S282012. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Shi SB, Ma TH, Li CH and Tang XY: Effect
of maintenance therapy with dendritic cells: cytokine-induced
killer cells in patients with advanced non-small cell lung cancer.
Tumori. 98:314–319. 2012.PubMed/NCBI
|
|
4.
|
Yang XJ, Huang JA, Lei W, Zhu YB and Zhang
XG: Antitumor effects of cocultured dendritic cells and
cytokine-induced killer cells on lung cancer in vitro and in vivo.
Ai Zheng. 25:1329–1333. 2006.(In Chinese).
|
|
5.
|
Ma Y, Xu YC, Tang L, Zhang Z, Wang J and
Wang HX: Cytokine-induced killer (CIK) cell therapy for patients
with hepatocellular carcinoma: efficacy and safety. Exp Hematol
Oncol. 1:112012. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Basili G, Nesi G, Barchielli A, Manetti A
and Biliotti G: Pathologic features and long-term results in early
gastric cancer: report of 116 cases 8–13 years after surgery. World
J Surg. 27:149–152. 2003.PubMed/NCBI
|
|
7.
|
Marrelli D, Roviello F, De Stefano A,
Fotia G, Giliberto C, Garosi L and Pinto E: Risk factors for liver
metastases after curative surgical procedures for gastric cancer: a
prospective study of 208 patients treated with surgical resection.
J Am Coll Surg. 198:51–58. 2004.
|
|
8.
|
Zhou QM, Wu PH, Zhao M, et al: Short-term
curative efficacy of cytokine-induced killer cells combined
micro-invasive treatments on hepatocellular carcinoma. Ai Zheng.
25:1414–1418. 2006.(In Chinese).
|
|
9.
|
Blattman JN and Greenberg PD: Cancer
immunotherapy: a treatment for the masses. Science. 305:200–205.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Shi L, Zhou Q, Wu J, Ji M, Li G, Jiang J
and Wu C: Efficacy of adjuvant immunotherapy with cytokine-induced
killer cells in patients with locally advanced gastric cancer.
Cancer Immunol Immunother. 61:2251–2259. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Rutella S and Locatelli F: Is there a role
for cytokine-induced killer cells in cancer immunotherapy?
Immunotherapy. 4:867–869. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Sangiolo D: Cytokine induced killer cells
as promising immuno-therapy for solid tumors. J Cancer. 2:363–368.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Jäkel CE, Hauser S, Rogenhofer S, Müller
SC, Brossart P and Schmidt-Wolf IG: Clinical studies applying
cytokine-induced killer cells for the treatment of renal cell
carcinoma. Clin Dev Immunol. 2012:4732452012.PubMed/NCBI
|
|
14.
|
Sangiolo D, Mesiano G, Carnevale-Schianca
F, Piacibello W, Aglietta M and Cignetti A: Cytokine induced killer
cells as adoptive immunotherapy strategy to augment graft versus
tumor after hematopoietic cell transplantation. Expert Opin Biol
Ther. 9:831–840. 2009. View Article : Google Scholar
|
|
15.
|
Zhang J, Zhu L, Wei J, Liu L, Yin Y, Gu Y
and Shu Y: The effects of cytokine-induced killer cells for the
treatment of patients with solid tumors: a clinical retrospective
study. J Cancer Res Clin Oncol. 138:1057–1062. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Schlimper C, Hombach AA, Abken H and
Schmidt-Wolf IG: Improved activation toward primary colorectal
cancer cells by antigen-specific targeting autologous
cytokine-induced killer cells. Clin Dev Immunol. 2012:2389242012.
View Article : Google Scholar
|