Introduction
The occurrence of an accessory spleen is relatively
common and observed in 10–30% of autopsy patients (1,2).
Accessory spleens are congenital foci of healthy splenic tissues
that are separate from the main body of the spleen (3). They often originate from a failed
fusion of the splenic anlage located in the dorsal mesogastrium
during the 5th week of fetal development (4). Although they have been found at sites
from the diaphragm to the scrotum, the vast majority are located in
the spleen region, usually in the splenic hilum or along the
splenic vessels or associated ligaments. The majority of accessory
spleens appear as small nodules arising from adjacent organs, such
as the kidney, adrenal gland and pancreas (5–10).
Cases arising from the stomach are relatively rare. In the present
case, the accessory spleen was unusual, presenting as a
gastrointestinal stromal tumor (GIST) of the stomach at
endoscopy.
This study was approved by the ethics committee of
Su Bei People’s Hospital of Jiangsu Province (Yangzhou, China). The
patient consented to the publication of this study.
Case report
A 61-year-old male was admitted to the Department of
Gastroenterology of Su Bei People’s Hospital of Jiangsu Province
(Yangzhou, China) presenting with an upper abdominal discomfort of
3 months in duration. Past and family histories were
non-contributory and the patient did not smoke or consume alcohol
and had undergone a splenectomy 20 years earlier. Upon admission,
physical examination and laboratory data, including peripheral
blood counts, were all unremarkable. The platelet count was
1.48×1011/l. The tumor markers showed no abnormalities
and were as follows: Carbohydrate antigen (CA)50, 3.75 KU/l (normal
range, <35.00); CA19-9, 2.09 KU/l (normal range, <35.00);
α-fetoprotein, 4.58 ng/ml (<20.00); and carcinoembryonic
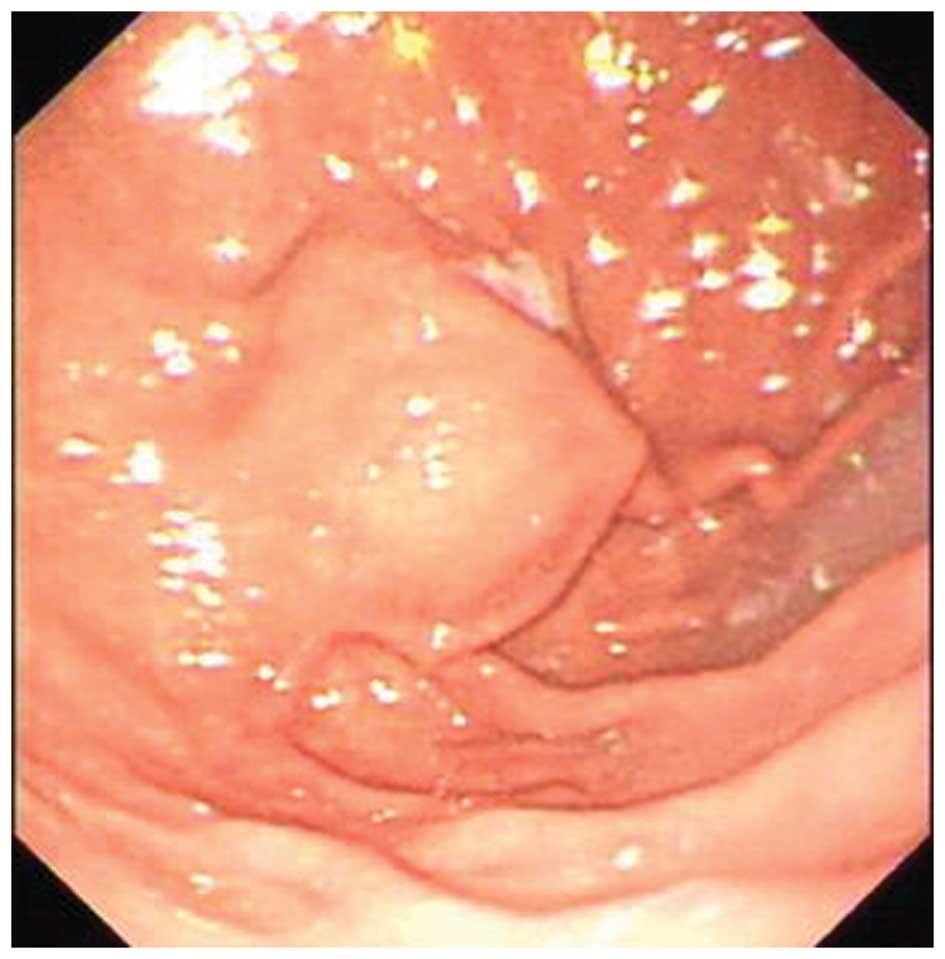
antigen, 0.95 ng/ml (normal range, <5.00). Gastrointestinal
endoscopy identified a fusiform mass at the posterior wall of the
upper gastric fundus (Fig. 1).
Endoscopic ultrasonography (EUS) revealed a tumor with low
homogenous echogenicity originating in the gastric muscular layer
(Fig. 2). Abdominal
contrast-enhanced computed tomography (CT) showed a well-marginated
ovoid mass ~2.6×1.9 cm in size located close to the gastric fundus
(Fig. 3). A diagnosis of gastric
GIST was made. Initially, endoscopic submucosal dissection was
considered, however, the perforation involved rendered the problem
difficult to repair by this method. Instead, gastroscopy was
combined with laparoscopy. Under a laparoscope, the tumor was
located at the posterior wall of the upper gastric fundus and was
~2.5×3.0 cm in size. Due to abdominal adhesions in the gastric
fundus, separation and exposure was difficult. Open surgery was
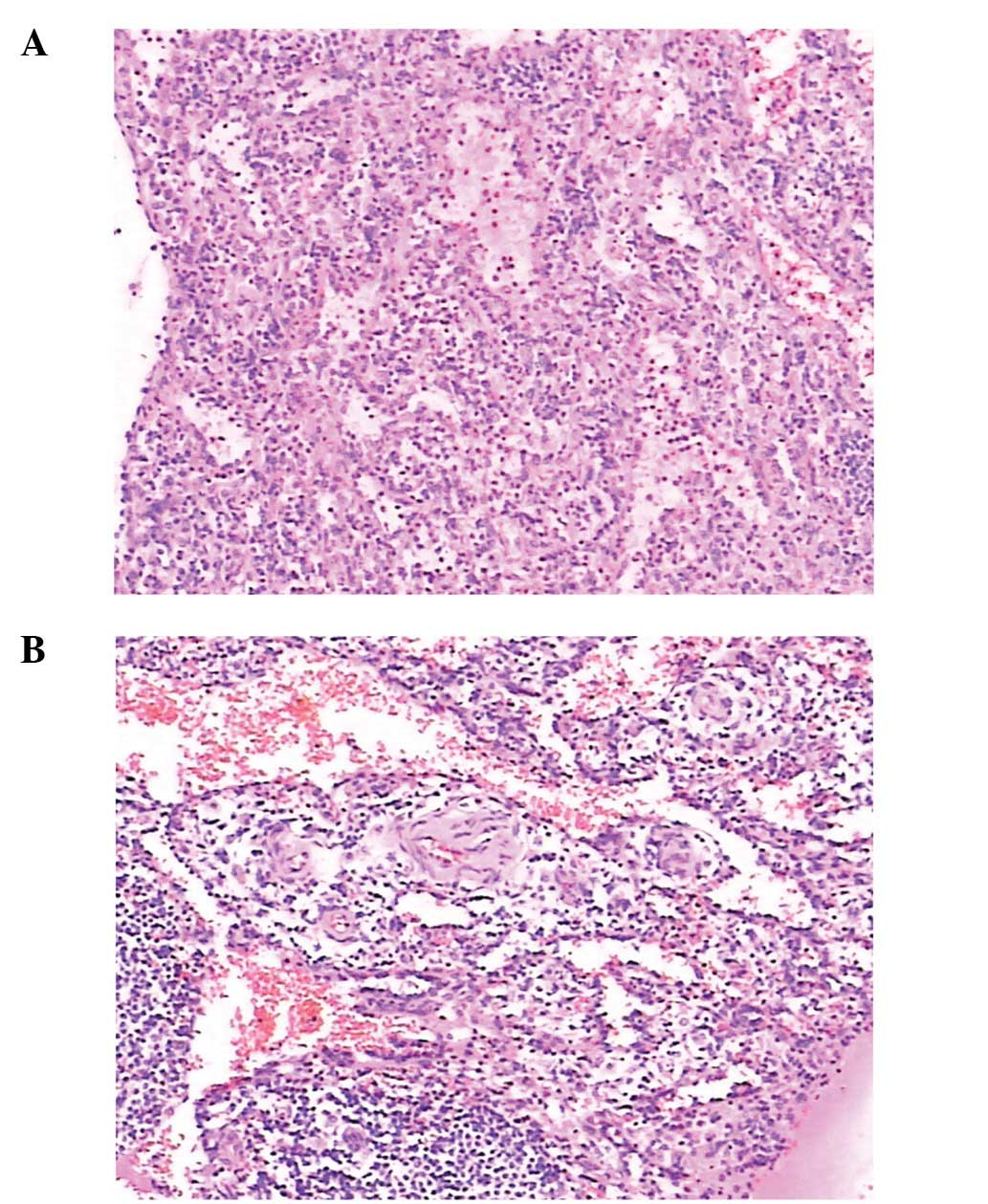
performed with enterolysis and partial gastrectomy. Histological
examination identified specific representative structures in the
red pulp and perifollicular zone of the human spleen. The tissue
was largely composed of monocytes and lymphocytes and numerous
sinusoidal spaces containing red blood cells were interspersed
among these cells. The terminal end of the capillary branches of
the arteriole sheaths were also identified, and were intermixed
with lymphocytes and plasmocytes (Fig.
4). These results indicated that the mass contained splenic
tissue, which confirmed it to be an accessory spleen.
Discussion
The current case report presents the diagnosis and
treatment of an accessory spleen adjoining the stomach fundus,
which appeared as a GIST at endoscopy in a patient who had
undergone a splenectomy 20 years earlier. It has been reported that
accessory spleens can have compensatory hypertrophy of residual
splenic tissue following splenectomy and occasionally reach 3–5 cm
in size (2). The accessory spleen
observed in the present case appeared to be a GIST, considering
that the patient had a history of splenectomy.
The following diagnostic approach can be considered
effective when the diagnosis is unclear. CT is an important imaging
technique used to evaluate the abdomen. It can identify the shape
of accessory spleens (oval or round) and whether attenuation is
identical to that of a proper splenic parenchyma prior to and
following administration of contrast medium (1). Familiarity with the CT features of
accessory spleens is useful to determine a diagnosis (6). Typically, accessory spleens are round
or oval and the attenuation is identical to that of the proper
splenic parenchyma prior to and following administration of
contrast medium (6). Vascular
branches arising from the splenic artery can be observed on dynamic
CT (1). Endoscopic ultrasonography
is able to show whether a mass with the homogenous parenchymal
texture has originated from extragastric tissue, such as splenic
parenchyma. The patient in the present case study had previously
undergone a splenectomy, therefore it was impossible to compare the
accessory spleen to proper splenic parenchyma. EUS-guided fine
needle aspiration is beneficial for diagnosis of accessory spleen,
which mimics a gastric subepithelial mass observed in histological
examination (11). However,
certain accessory spleens mimic an enlarged lymph node or tumor
arising from adjacent organs, such as the kidney, adrenal gland or
pancreas (12–15). Similarly, accessory spleens may be
differentiated from metastatic lesions or lymphadenopathy when they
are enhanced to the same degree as the spleen (1). In such cases, technetium 99m sulfur
colloid scintigraphy provides an easy method of establishing the
identity of ectopic splenic tissues (5,6). The
mass mimicking GIST was readily identified by radionuclide imaging
in the present case, resulting in the definite diagnosis of
accessory spleens. An accessory spleen should be suspected in this
type of case. In addition, ectopic splenic tissue may be caused by
autotransplantation of splenic cells within the peritoneal cavity
resulting from traumatic disruption of the splenic capsule
(16,17).
Although an accessory spleen is usually found
incidentally with no clinical significance in the majority of
patients (1,6), it may occasionally be relevant to
detection and characterization in clinical situations (18–20).
Accessory spleens may become symptomatic due to spontaneous
rupture, hemorrhage, embolism or torsion. The clinical significance
of a residual accessory spleen post-splenectomy varies according to
the individual conditions. Surgeons must be aware of their presence
when the intention is to remove functional splenic tissues. The
return of splenic function caused by compensatory enlargement of
ectopic splenic tissues has been implicated in the recurrence of
hematological disorders, such as thrombocytopenic purpura (18–20).
During follow-up, the platelet count of the present
patient increased to 3.92×1011/l on the second day
following surgery and a high level of 4.10×1011/l was
observed on day 9. The patient peripheral blood count returned to
normal after 2 weeks, and there was no evidence of recurrence.
Platelet count usually increases within 2–3 days of splenectomy,
peaks between 7 and 14 days and then gradually decreases and
returns to normal after 1–2 months (21). This condition may cause venous
thrombosis if the platelet count increases abnormally. Once
thrombosis has extended to the superior mesenteric vein, it may
cause extensive necrosis of its convolutions. Similarly, high
postoperative platelet counts can easily lead to deep venous
thrombosis of the lower limbs, resulting in pulmonary embolism and
even mortality. For this reason, changes in platelet count should
be observed carefully following a splenectomy. Appropriate
treatment based on the platelet count and liver function may
provide good therapeutic effects.
In conclusion, patients who present with accessory
spleen arising from gastric fundus following splenectomy should
undergo careful follow-up by imaging examination, including CT. If
the clinical course is uneventful and the patient remains
asymptomatic without any abnormalities in physical and laboratory
examinations, then splenectomy should not be performed. Changes in
postoperative platelet count should be taken into account. If
splenectomy is necessary, platelet count should be used as a
routine monitoring indicator.
References
|
1
|
Halpert B and Gyorkey F: Lesions observed
in accessory spleens of 311 patients. Am J Clin Pathol. 32:165–168.
1959.PubMed/NCBI
|
|
2
|
Beahrs JR and Stephens DH: Enlarged
accessory spleens: CT appearance in postsplenectomy patients. AJR
Am J Roentgenol. 135:483–486. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Freeman JL, Jafri SZ, Roberts JL, Mezwa DG
and Shirkhoda A: CT of congenital and acquired abnormalities of the
spleen. Radiographics. 13:597–610. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Dodds WJ, Taylor AJ, Erickson SJ, Stewart
ET and Lawson TL: Radiologic imaging of splenic anomalies. AJR Am J
Roentgenol. 155:805–810. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mortelé KJ, Mortelé B and Silverman SG: CT
features of the accessory spleen. AJR Am J Roentgenol.
183:1653–1657. 2004.PubMed/NCBI
|
|
6
|
Gayer G, Zissin R, Apter S, et al: CT
findings in congenital anomalies of the spleen. Br J Radiol.
74:767–772. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hayward I, Mindelzun RE and Jeffrey RB:
Intrapancreatic accessory spleen mimicking pancreatic mass on CT. J
Comput Assist Tomogr. 16:984–985. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Harris GN, Kase DJ, Bradnock H and
Mckinley MJ: Accessory spleen causing a mass in the tail of the
pancreas: MR imaging findings. AJR Am J Roentgenol. 163:1120–1121.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Stiris MG: Accessory spleen versus left
adrenal tumor: computed tomographic and abdominal angiographic
evaluation. J Comput Assist Tomogr. 4:543–544. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tsuchiya N, Sato K, Shimoda N, et al: An
accessory spleen mimicking a nonfunctional adrenal tumor: a
potential pitfall in the diagnosis of a left adrenal tumor. Urol
Int. 65:226–228. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ahn JY, Jung HY, Kim do H, et al:
Diagnosis of an accessory spleen mimicking a gastric submucosal
tumor using endoscopic ultrasonography-guided fine-needle
aspiration. Korean J Gastroenterol. 59:433–436. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Seo T, Ito T, Watanabe Y and Umeda T:
Torsion of an accessory spleen presenting as an acute abdomen with
an inflammatory mass. US, CT, and MRI findings. Pediatr Radiol.
24:532–534. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Valls C, Monés L, Gumà A and López-Calonge
E: Torsion of a wandering accessory spleen: CT findings. Abdom
Imaging. 23:194–195. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Coote JM, Eyers PS, Walker A and Wells IP:
Intra-abdominal bleeding caused by spontaneous rupture of an
accessory spleen: the CT findings. Clin Radiol. 54:689–691. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Pérez Fontán FJ, Soler R, Santos M and
Facio I: Accessory spleen torsion: US, CT and MR findings. Eur
Radiol. 11:509–512. 2001.PubMed/NCBI
|
|
16
|
Brewster DC: Splenosis. Report of two
cases and review of the literature. Am J Surg. 126:14–19.
1973.PubMed/NCBI
|
|
17
|
Fleming CR, Dickson ER and Harrison EG Jr:
Splenosis: autotransplantation of splenic tissue. Am J Med.
61:414–419. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Facon T, Caulier MT, Fenaux P, et al:
Accessory spleen in recurrent chronic immune thrombocytopenic
purpura. Am J Hematol. 41:184–189. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Antevil J, Thoman D, Taller J and Biondi
M: Laparoscopic accessory splenectomy with intraoperative gamma
probe localization for recurrent idiopathic thrombocytopenic
purpura. Surg Laparosc Endosc Percutan Tech. 12:371–374. 2002.
View Article : Google Scholar
|
|
20
|
Budzynski A, Bobrzyński A, Sacha T and
Skotnicki A: Laparoscopic removal of retroperitoneal accessory
spleen in patient with relapsing idiopathic thrombocytopenic
purpura 30 years after classical splenectomy. Surg Endosc.
16:16362002.
|
|
21
|
Koyanagi N, Iso Y, Higashi H, Kitano S and
Sugimachi K: Increased platelet count as a screening test for
distal splenorenal shunt patency. Am J Surg. 156:29–33. 1988.
View Article : Google Scholar : PubMed/NCBI
|