Introduction
Lung cancer is the most common cause of cancer
mortality in males and females worldwide (1). The World Health Organization
estimates that worldwide lung cancer mortality should continue to
rise, largely due to the increase in global tobacco smoke, which is
the main risk factor responsible for 80–90% of all lung carcinomas
(2). Non-smokers account for only
10–15% of the incidence of lung cancer, which is often attributed
to a combination of genetic factors, occupational exposure,
including radon gas and asbestos, air pollution and second hand
smoke (3). Clinical therapies of
lung cancer are principally composed of surgery, radiation,
chemotherapy, targeted therapy and palliative care, alone or in
combination, in an attempt to cure or lessen the adverse impact of
malignant neoplasms originating in the lung tissue (4,5).
Surgical resection remains the first choice of therapy for the
majority of patients with lung cancer (6). However, all curative therapies for
lung cancer inevitably result in certain negative effects with
regard to post-operative pulmonary function and quality of life
(QOL) following rehabilitation (7). Breathlessness, alongside coughing,
for instance, is the most common depressing secondary symptom in
lung cancer patients, which may lead to physical disability, loss
of independence and dignity and lowered self-esteem with associated
psychosocial distress, thereby severely affecting the QOL of
patients with lung cancer (8).
Moreover, breathlessness is a poorly controlled symptom against
which traditional pharmacological interventions, including
benzodiazepines, opioids and oxygen, are often ineffective
(9). Therefore, breathing
exercises as a non-pharmacological approach to improve
post-operative pulmonary function and QOL in lung cancer patients
have attracted increasing attention in recent years.
Breathing exercises aim to correct breathing errors,
reestablish a proper breathing pattern, increase diaphragm
activity, elevate the amount of alveolar ventilation, reduce energy
consumption when breathing and relieve the shortness of breath
experienced by patients with lung cancer. Several studies have
shown that a number of patients with lung cancer fear the
possibility of suffocation when they feel breathless during
physical activities such as climbing stairs (10,11).
In order to combat this shortness of breath, breathinxg exercises
are used as an alternative treatment to bolster post-operative
pulmonary function by teaching patients to utilize more of their
lungs (12). In their simplest
form, breathing exercises consist of elongating and slowing down
the inhalation and exhalation, which allow lung cancer patients to
take deeper breaths that increase their intake of oxygen, rather
than taking shallow breaths that only make use of the top half of
their lungs (13). Previously,
studies examining the effect of breathing exercises on improvements
to post-operative pulmonary function and QOL following
rehabilitation showed inconclusive results. However, the majority
of studies came to the conclusion that lung cancer patients
suffering from breathlessness benefited from breathing exercises
with regard to the aspects of post-operative pulmonary function and
QOL (14–16). Certain other studies have not
demonstrated the favorable effects of breathing exercises on
post-operative pulmonary function and QOL in patients with lung
cancer (17). Given these
circumstances, a meta-analysis was performed to evaluate the
clinical value of breathing exercises on post-operative pulmonary
function and QOL in patients with lung cancer.
Materials and methods
Literary search strategy
Relevant manuscripts published prior to October 1st
2012 were identified through a search of Pubmed, Embase, the Web of
Science and CBM databases using the following terms: ‘lung
neoplasms’, ‘pulmonary neoplasms’, ‘pulmonary neoplasm’, ‘lung
cancer’ or ‘bronchial neoplasms’; and ‘breathing exercises’,
‘exercise of breathing’, ‘respiratory muscle training’ or ‘training
of respiratory muscle’. Eligible articles or textbooks were also
reviewed and checked via manual searches to find other potential
studies. Any disagreements were resolved by discussion between the
authors.
Inclusion and exclusion criteria
To be eligible for inclusion in the present
meta-analysis, the following criteria were established: i) The
study must be a clinical study focused on the effect of breathing
exercises on post-operative pulmonary function and QOL in patients
with lung cancer; ii) all patients diagnosed with lung cancer
should have had confirmation from a pathological examination of the
surgical specimen; iii) the patients in the treatment group must
have been assigned to receive breathing exercises, including
inspiratory muscle training, simple relaxation techniques, activity
pacing or psychosocial support, under the guidance of their
physicians and nurse; and iv) sufficient data must be published on
the outcomes of the breathing exercises, including pulmonary
function, QOL, visual analog scales (VAS), hospital anxiety and
depression. Studies were excluded when they were: i) Not clinical
studies that evaluated the clinical value of breathing exercises on
post-operative pulmonary function and QOL in patients with lung
cancer; ii) case reports, letters, reviews, meta-analyses and
editorial articles; iii) studies that were based on incomplete raw
data and those with no usable data reported; and iv) duplicates of
previous publications.
Data extraction
Using a standardized form, data from the published
studies were extracted independently by two reviewers to populate
the necessary information. For each study, the following
characteristics were collected: the first author, year of
publication, country, language, study design, number of cases,
ethnicity, inclusion criteria, pathological type, follow-up period
and outcome index. In cases of conflicting analysis, an agreement
was reached following a discussion between the authors. If
required, a third reviewer confirmed any discrepancies or
uncertainties related to the data abstraction process.
Quality assessment of the included
studies
The methodological quality of the included studies,
including randomization, similarity of groups, co-intervention,
masking, outcome measures, compliance, exercise regime and
follow-up, was evaluated by two independent reviewers using a
modified methodological quality scale (18). A total of eight assessment items
matching with the quality appraisal were used in this meta-analysis
with scores ranging from 0 to 40 (5 scores for each item). Scores
of 0–19, 20–29 and 30–40 were defined as low, moderate and high
quality, respectively. The two reviewers resolved any differences
of opinion by discussion.
Statistical analysis
The differences between the pre-intervention and
post-intervention results of breathing exercises on post-operative
pulmonary function and QOL were measured by standardized mean
differences (SMDs) with 95% confidence intervals (CIs). The
statistical significance of the pooled SMD was examined by Z-test.
Between-study variations and heterogeneities were estimated using
Cochran’s Q statistic and P<0.05 was considered to indicate a
statistically significant heterogeneity (19). The effect of heterogeneity was also
quantified using the I2 test, which ranges from 0–100%
and represents the proportion of inter-study variability that may
be contributed by heterogeneity rather than by chance (20). When the Q-test was significant
(P<0.05) or I2>50% this indicated that
heterogeneity existed among the studies and the random-effects
model (DerSimonian-Laird method) was conducted in the
meta-analysis. Otherwise, the fixed-effects model (Mantel-Haenszel
method) was used. A sensitivity analysis was performed by omitting
each study in turn to assess the stability of the results. Begg’s
funnel plots and Egger’s linear regression tests, which measure
funnel plot asymmetry, were used to detect any publication bias
(21). All the P-values were
two-sided and P<0.05 was considered to indicate a statistically
significant difference. All analyses were calculated using STATA
Version 12.0 software (Stata Corp, College Station, TX, USA).
Results
Characteristics of the included
studies
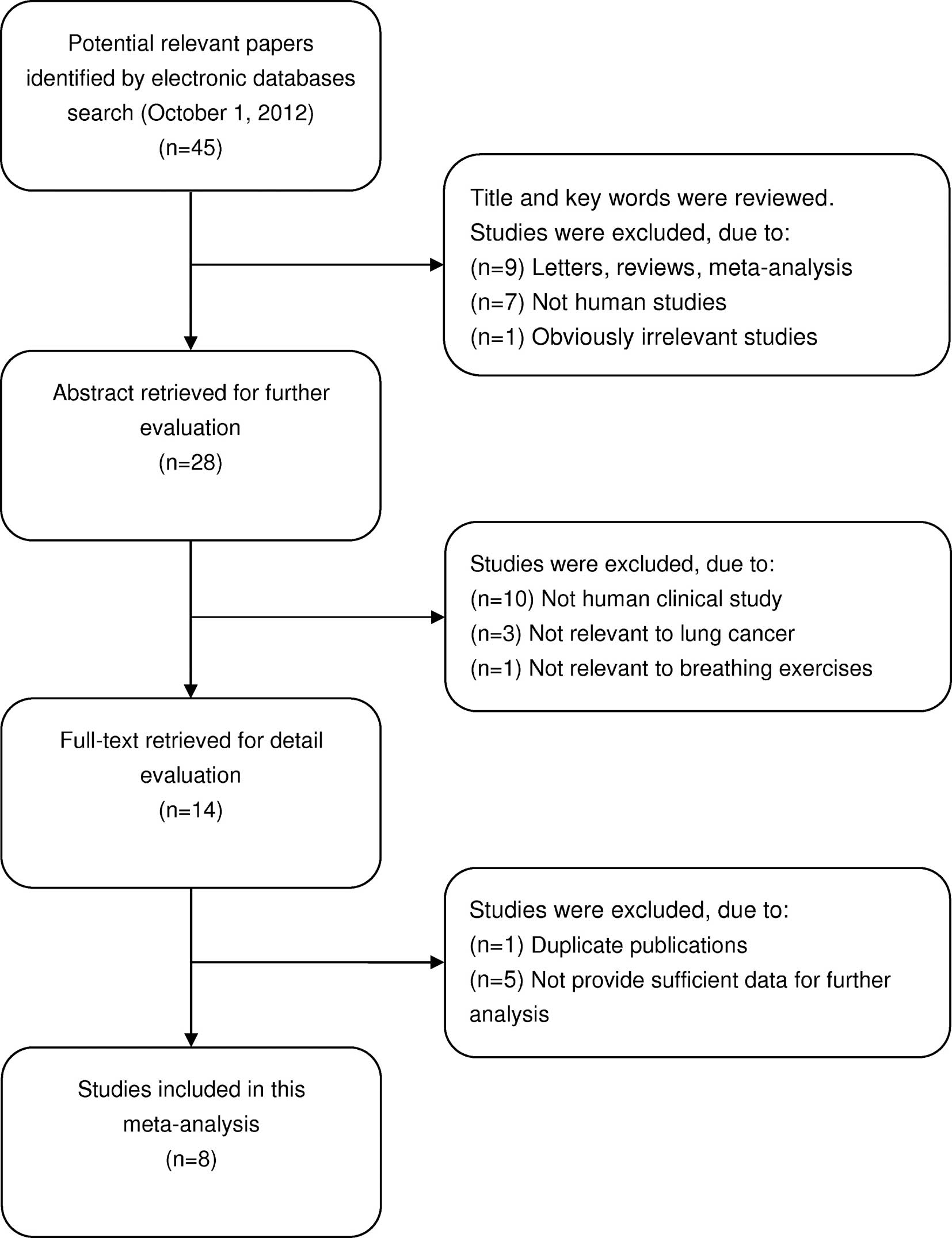
In total, 45 potentially relevant studies were
identified by searching electronic databases. According to the
inclusion criteria, 8 clinical studies (8,15–17,22–25)
were included and 37 articles were excluded in the present
meta-analysis. The details of the selection process are presented
in a flow chart in Fig. 1. The
publication year for the involved studies ranged from 1996 to 2012.
A total of 398 lung cancer patients were included in these eight
studies, which all evaluated the effect of breathing exercises on
post-operative pulmonary function and QOL in patients with lung
cancer. All patients fulfilled the diagnostic criteria of lung
cancer, as confirmed by pathological examination of surgical
specimens. Five studies had been carried out in China and three
studies in the UK. According to the modified methodological quality
scale, the scores of all the included studies were moderately high
(>20 points) and varied from 20 to 31 (median, 24). The main
characteristics and methodological quality of all the eligible
studies are listed in Table I. A
summary of the differences between the pre-intervention and
post-intervention results for post-operative pulmonary function and
QOL is provided in Table II.
 | Table ICharacteristics of studies included in
the present meta-analysis. |
Table I
Characteristics of studies included in
the present meta-analysis.
| First author
(ref.) | Year | Country | Ethnicity | Study design | Case number | Duration of
intervention | Frequency of
sessions | Main outcome
measures | Quality scores |
|---|
| Corner et al
(22) | 1996 | UK | Caucasian | RCT | 11 | 3–6 weeks | Weekly | Visual analog scales,
hospital anxiety and depression scale | 30 |
| Bredin et al
(23) | 1999 | UK | Caucasian | RCT | 51 | 3–8 weeks | Weekly | Visual analog scales,
hospital anxiety and depression scale | 26 |
| Hately et al
(8) | 2003 | UK | Caucasian | Cohort study | 30 | 4–6 weeks | Weekly | Visual analog
scales | 25 |
| Li (24) | 2003 | China | Asian | Cohort study | 38 | 6 months | 6 months | Pulmonary function,
quality of life | 21 |
| Ye et al
(17) | 2004 | China | Asian | Cohort study | 52 | 6 months | 3 months | Pulmonary function,
quality of life | 22 |
| Pan et al
(15) | 2005 | China | Asian | Cohort study | 82 | 1–6 months | 6 months | Pulmonary function,
quality of life | 20 |
| Shi (16) | 2006 | China | Asian | Cohort study | 48 | 6 months | 3 months | Pulmonary function,
quality of life | 23 |
| Zhou et al
(25) | 2012 | China | Asian | Cohort study | 86 | 1 week | 1 week | Pulmonary
function | 22 |
 | Table IISummary of the effect of breathing
exercises on post-operative pulmonary function and quality of
life. |
Table II
Summary of the effect of breathing
exercises on post-operative pulmonary function and quality of
life.
| Parameters | SMD | 95% CI | P-value | Ph | I2
(%) |
|---|
| Pulmonary
function | | | | | |
| FEV1 | 3.369 | 1.968, 4.770 | <0.001a | <0.001 | 98.40 |
| FVC | 0.192 | −0.199, 0.582 | 0.336a | <0.001 | 83.50 |
| FEV1/FVC | 1.77 | 0.148, 3.392 | 0.032a | <0.001 | 98.50 |
| Quality of
life | | | | | |
| The ability of
self-care in daily life | −0.992 | −1.467, −0.517 | <0.001a | <0.001 | 85.00 |
| Social
activities | −0.936 | −1.725, −0.148 | 0.02a | <0.001 | 94.50 |
| Symptoms of
depression | −0.911 | −1.249, −0.572 | <0.001a | 0.007 | 71.40 |
| Symptoms of
anxiety | −0.914 | −1.201, −0.628 | <0.001a | 0.04 | 60.10 |
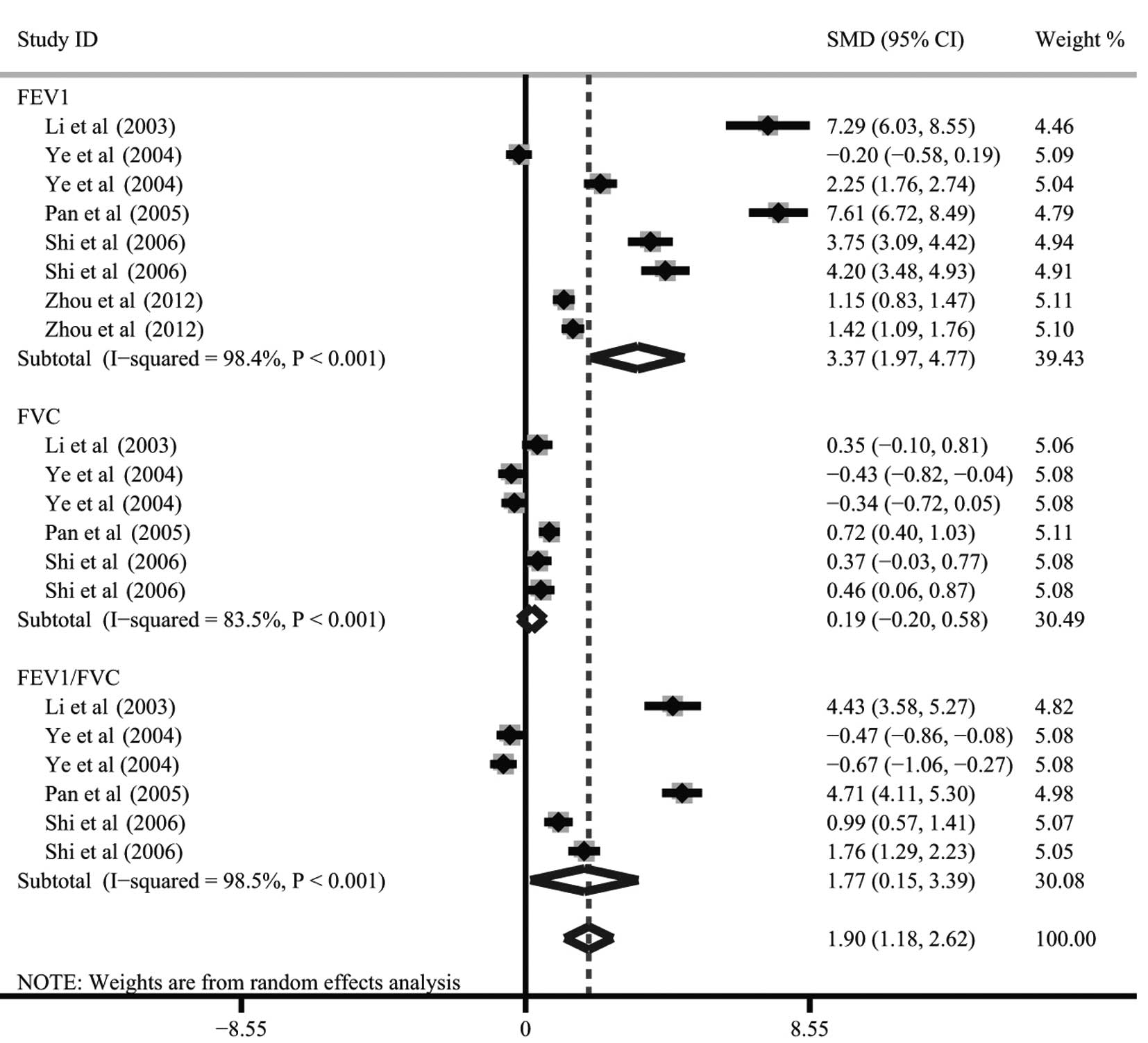
Pulmonary function
The difference between the pre-intervention and
post-intervention results of breathing exercises on pulmonary
function was investigated in five studies. There were three main
outcome indices, including the forced vital capacity (FVC), the
forced expiratory volume in 1 sec (FEV1) and the the ratio of
FEV1/FVC. The heterogeneity was significant (all P<0.05) so the
random-effects model was used. When all five studies were pooled
into the meta-analysis, there was a significant difference between
the pre-intervention and post-intervention results of breathing
exercises on FEV1 and FEV1/FVC (FEV1: SMD, 3.37; 95% CI, 1.97–4.77;
P<0.001; FEV1/FVC: SMD, 1.77; 95% CI, 0.15–3.39; P=0.032), but
no difference was identified for FVC (SMD, 0.19; 95% CI,
−0.20–0.58; P=0.336; Fig. 2).
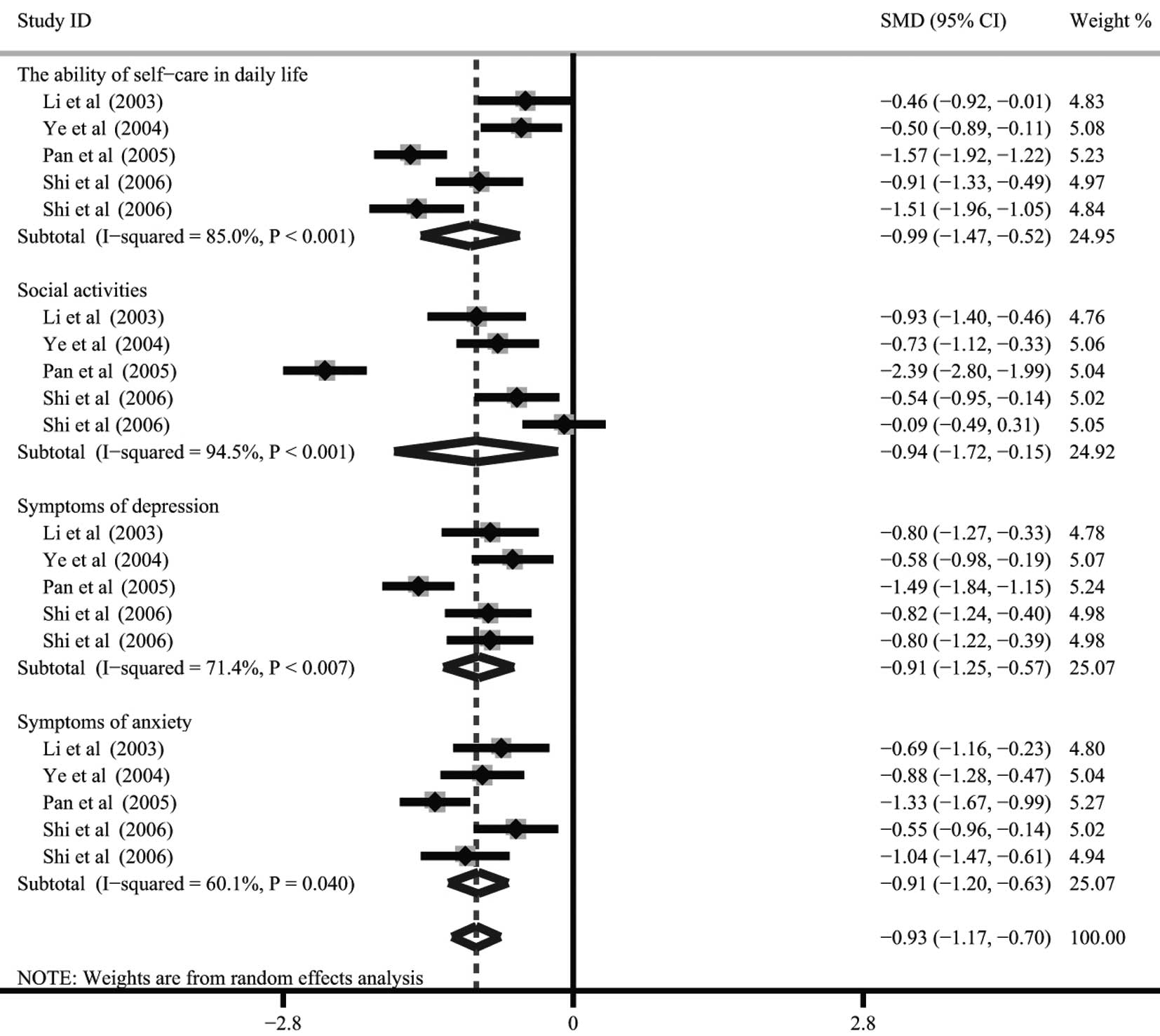
QOL
There were four studies [Li (24), Ye et al (17), Pan et al (15) and Shi (16)] that referred to the differences
between the pre-intervention and post-intervention results of
breathing exercises on QOL. The four main outcome indices that were
addressed were the ability of self-care in daily life, engagement
in social activities, the symptoms of depression and the symptoms
of anxiety. Since heterogeneity existed (all P<0.05), the
random-effects model was conducted to pool the results. The
meta-analysis results indicated that the QOL in patients with lung
cancer was significantly improved following the intervention with
breathing exercises. There were significant differences between the
pre-intervention and post-intervention results of breathing
exercises on the ability of self-care in daily life (SMD, −0.99;
95% CI, −1.47 to −0.52; P<0.001), engagement in social
activities (SMD, −0.936; 95% CI, −1.725 to −0.148; P=0.02), the
symptoms of depression (SMD, −0.91; 95% CI, −1.25 to −0.57;
P<0.001) and the symptoms of anxiety (SMD, −0.91; 95% CI, −1.20
to −0.63; P<0.001; Fig. 3).
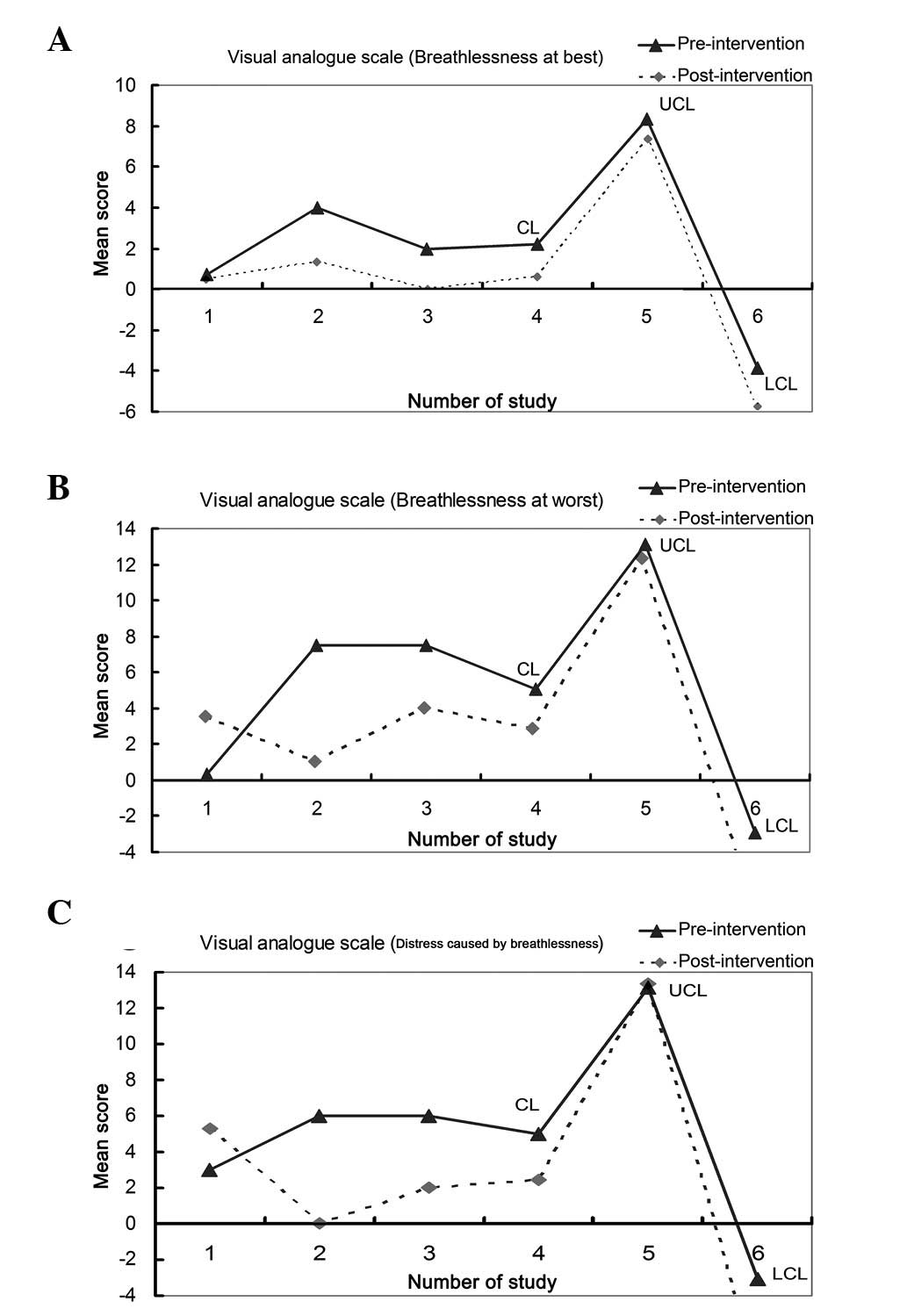
VAS
Only three studies referred to the differences
between the pre-intervention and post-intervention results of
breathing exercises in the VAS (8,22,23).
The three main outcome indices addressed were breathlessness at
worst, breathlessness at best and distress caused by
breathlessness. Due to limited data, the analysis of this was only
qualitative. No significant differences were observed between the
pre-intervention and post-intervention results of breathing
exercises for the VAS in the three broken-line graphs (Fig. 4).
Hospital anxiety and depression
There were also only two studies (22,23)
that referred to the differences between the pre-intervention and
post-intervention results of breathing exercises on hospital
anxiety and depression. Qualitative data analysis showed that there
were no significant differences between these results (Fig. 5).
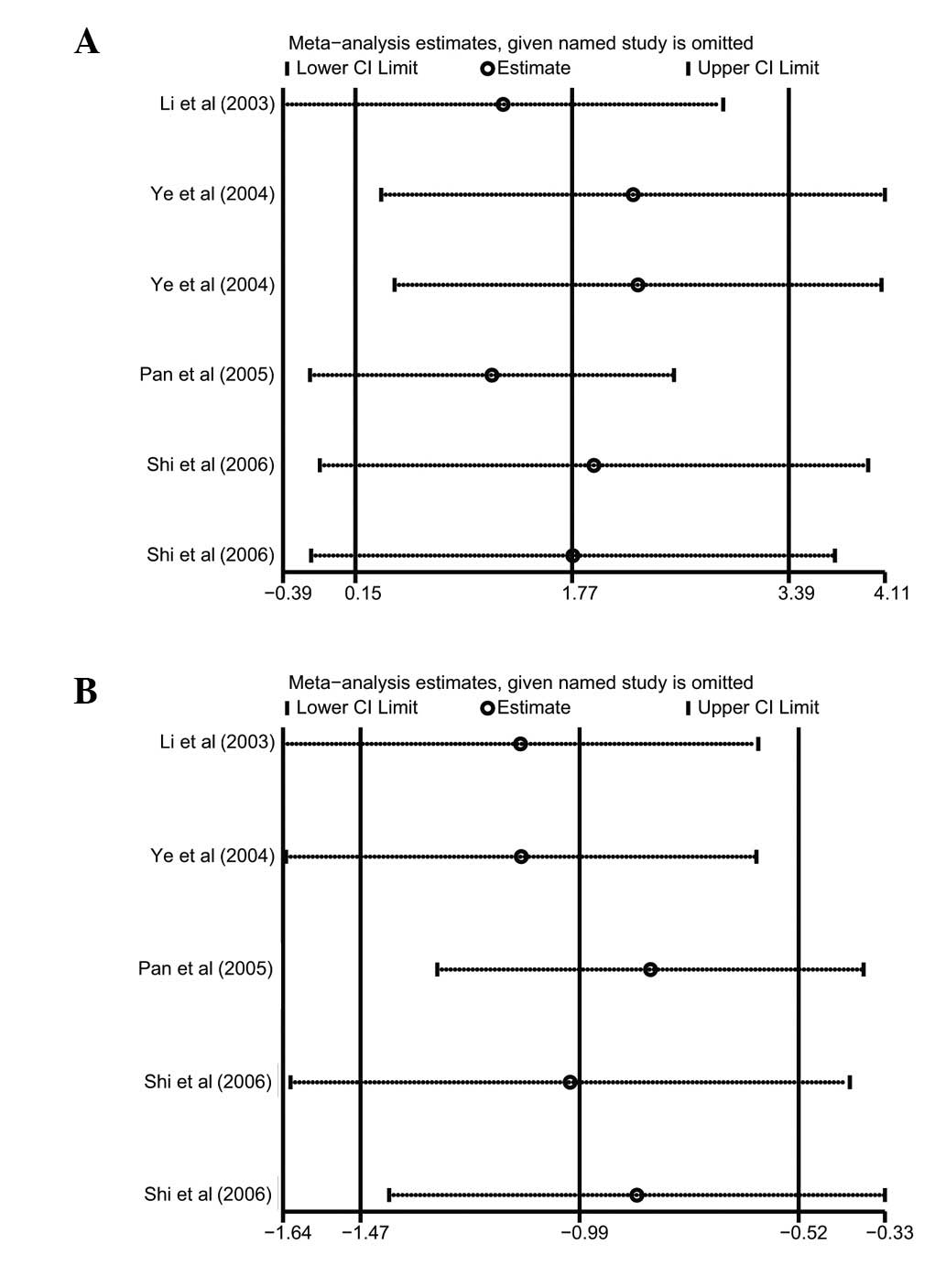
Sensitivity analysis and publication
bias
A sensitivity analysis was performed to assess the
effect of each individual study on the pooled SMD of pulmonary
function and QOL analysis by omission of individual studies. The
analysis results suggested that no individual study significantly
affected the pooled values of the clinical events (Fig. 6), indicating that the results of
the present study are statistically robust.
Publication bias exists to the extent that available
research results are unrepresentative of all research results. A
Begg’s funnel plot and Egger’s linear regression test were
performed to assess the publication bias of the included studies.
The shapes of the funnel plots for pulmonary function and QOL
analysis did not reveal any evidence of marked asymmetry (Fig. 7). Egger’s test also showed that
there was no statistically significant evidence of a publication
bias (pulmonary function: t=2.47, P=0.062; QOL: t=0.70,
P=0.534).
Discussion
Currently, surgical therapy for lung cancer is aimed
not only at prolonging survival periods, but additionally at
improving post-operative QOL, which is also the ultimate goal of
effective cancer treatment (5).
However, due to the impact of multiple factors subsequent to
surgery, including anesthesia, wound pain, pleural reaction and
pleural adhesions, there is an inevitable decline in respiratory
function, breathing difficulty, abnormal lung capacity ventilation,
reduced effective diffusion area and an imbalanced
ventilation/perfusion ratio, to various degrees (6). In order to correct these aberrant
pulmonary functions, the body spontaneously over-utilizes auxiliary
respiratory muscles and thereby forms an improper breathing
pattern. The formation of an incorrect pattern of breathing not
only fails to relieve irregular post-operative symptoms, but also
makes patients with lung cancer more susceptible to respiratory
muscle fatigue, hypoxia and carbon dioxide retention, which may
eventually cause chronic obstructive pulmonary disease and
respiratory failure, including breathlessness (13). The occurrence of breathlessness may
seriously affect the length of survival, self-care ability, labor
and interpersonal skills of patients with lung cancer and
accordingly decrease QOL and lead to psychological depression and
anxiety (9).
Breathing exercises have long been recognized as an
effective method to reduce the post-operative complications of lung
cancer, including breathlessness, and thus improve pulmonary
function and QOL by strengthening the respiratory muscles (16). Breathing exercises may be
categorized into specific and non-specific respiratory muscle
training. Specific breathing exercises, including lip reduction and
deep abdominal breathing exercises, are conducted primarily in a
pressurized respiratory manner. Generally, lip reduction breathing
exercises refer to the nasal inspiratory and lip reduction
expiratory breathing patterns caused by shrinking the lips, as if
whistling, to slowly exhale the gas and then maintaining this for
>10 sec (14). Deep abdominal
breathing exercises allow patients to train in a sitting, supine or
lateral position, and requires concentration, natural postures,
relaxation of the muscles and a gradual deepening of breathing to
reach a maximum lung capacity. The air is then excluded for 10 sec
and the patient should exhale slowly (14). In addition, non-specific breathing
exercises are often identified as whole body exercises, including
stair climbing, qigong, breathing gymnastics and balloon blowing
(26). The applications of proper
breathing exercises, together with symptomatic care and a
comprehensive and timely assessment of the physical and
psychological state of patients with lung cancer, show promise in
relieving the symptoms of breathlessness and in improving the
post-operative pulmonary function and QOL following rehabilitation
(27).
However, studies investigating the improvements to
post-operative pulmonary function and QOL caused by breathing
exercises have suggested conflicting results. Therefore, the
present meta-analysis of all eligible studies was performed to
evaluate the exact effects of breathing exercises on post-operative
pulmonary function and QOL in patients with lung cancer. A
significant enhancement in pulmonary function was observed in FEV1
and FEV1/FVC following the use of breathing exercises, but no
significant differences were identified in FVC between the
pre-intervention and post-intervention results of breathing
exercises. These results were inconsistent with those of several
previous studies (14–16). This may have been due to the
deviation of the instruments measuring the pulmonary function
parameters, the baseline characteristics (such as histological
type, differentiation and disease stage) of the patients or the
duration of the follow-up. Additionally, the present study
demonstrated a significant reduction in the symptoms of depression
and anxiety caused by breathlessness and a decrease in the
promotion of the ability to perform self-care for daily living and
to engage in social activities, indicating an improvement in the
post-operative QOL of the patients with lung cancer. The outcomes
of the VAS, which are usually utilized to measure the degree of
breathlessness, were also analyzed and no significant differences
were observed in the degree of breathlessness between the
pre-intervention and post-intervention results of the breathing
exercises.
In interpreting the results of the current
meta-analysis, specific issues pertinent to this study need to be
addressed. Firstly, the sample size included in the present study
is relatively small and may have overestimated the clinical values
of breathing exercises on post-operative pulmonary function and QOL
in patients with lung cancer. In addition, the origins of
heterogeneity may include a number of factors, including criteria,
characteristics of the patients and the follow-up period. A
selection bias may exist due to the differences in the mean age of
the subjects, the duration of the intervention, the inclusion
criteria or the study design. Finally, although all the
participants in each study were well defined with similar inclusion
criteria, there may be potential factors that have not been taken
into account that may have affected the results and they should
therefore be interpreted with caution owing to the potential
heterogeneity among trials.
In conclusion, this meta-analysis provides strong
evidence that breathing exercises may significantly improve
post-operative pulmonary function and QOL in patients with lung
cancer. Based on the limitations mentioned, larger clinical trials
are required to confirm these findings. Further studies
investigating the role of breathing exercises following surgical
therapy are also required.
References
|
1
|
Ferlay J, Shin HR, Bray F, et al:
Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int
J Cancer. 127:2893–2917. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pesch B, Kendzia B, Gustavsson P, et al:
Cigarette smoking and lung cancer - relative risk estimates for the
major histological types from a pooled analysis of case-control
studies. Int J Cancer. 131:1210–1219. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Stolz A, Pafko P, Harustiak T, et al: Risk
factor analysis for early mortality and morbidity following
pneumonectomy for non-small cell lung cancer. Bratisl Lek Listy.
112:165–169. 2011.PubMed/NCBI
|
|
4
|
Kim AW, Boffa DJ, Wang Z and Detterbeck
FC: An analysis, systematic review, and meta-analysis of the
perioperative mortality after neoadjuvant therapy and pneumonectomy
for non-small cell lung cancer. J Thorac Cardiovasc Surg.
143:55–63. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bongers ML, Coupé VM, Jansma EP, et al:
Cost effectiveness of treatment with new agents in advanced
non-small-cell lung cancer: a systematic review. Pharmacoeconomics.
30:17–34. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Goldstein SD and Yang SC: Role of surgery
in small cell lung cancer. Surg Oncol Clin N Am. 20:769–777. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cella D: Quality of life considerations in
patients with advanced lung cancer. Semin Oncol. 31(6 Suppl 11):
16–20. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hately J, Laurence V, Scott A, et al:
Breathlessness clinics within specialist palliative care settings
can improve the quality of life and functional capacity of patients
with lung cancer. Palliat Med. 17:410–417. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Dorman S, Jolley C, Abernethy A, et al:
Researching breathlessness in palliative care: consensus statement
of the National Cancer Research Institute Palliative Care
Breathlessness Subgroup. Palliat Med. 23:213–227. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bobbio A, Chetta A, Ampollini L, et al:
Preoperative pulmonary rehabilitation in patients undergoing lung
resection for non-small cell lung cancer. Eur J Cardiothorac Surg.
33:95–98. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Benzo R, Wigle D, Novotny P, et al:
Preoperative pulmonary rehabilitation before lung cancer resection:
results from two randomized studies. Lung Cancer. 74:441–445. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nici L: Preoperative and postoperative
pulmonary rehabilitation in lung cancer patients. Thorac Surg Clin.
18:39–43. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ozalevli S, Ilgin D, Kul Karaali H, et al:
The effect of in-patient chest physiotherapy in lung cancer
patients. Support Care Cancer. 18:351–358. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhou YR, Xiong J, Luo LC, Dong CP and Lu
M: Effect of respiration training of postoperative lung function in
patients with lung cancer. Journal of Nursing Science. 21:36–37.
2006.(In Chinese).
|
|
15
|
Pan YM, Pan TC, Zhang LH, et al: A
clinical study of respiration training in lung cancer patients
improving the postoperative lung function and quality of life.
Zhonghua Wu Li Yi Xue Yu Kang Fu Za Zhi. 548–550. 2005.(In
Chinese).
|
|
16
|
Shi A: The effect of breathing exercises
on postoperative lung function and quality of life of patients with
lung cancer. Chin J Misdiagn. 4764–4765. 2006.(In Chinese).
|
|
17
|
Ye YJ, Chen SD, Yu HC, et al: Effect of
breathing exercise on lung function and quality of life in patients
with lung cancer after radiotherapy. Zhongguo Lin Chuang Kang Fu.
7390–7392. 2004.(In Chinese).
|
|
18
|
Smith K, Cook D, Guyatt GH, et al:
Respiratory muscle training in chronic airflow limitation: a
meta-analysis. Am Rev Respir Dis. 145:533–539. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Higgins JP and Thompson SG: Quantifying
heterogeneity in a meta-analysis. Stat Med. 21:1539–1558. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zintzaras E and Ioannidis JP:
Heterogeneity testing in meta-analysis of genome searches. Genet
Epidemiol. 28:123–137. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Peters JL, Sutton AJ, Jones DR, et al:
Comparison of two methods to detect publication bias in
meta-analysis. JAMA. 295:676–680. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Corner J, Plant H, A’Hern R and Bailey C:
Non-pharmacological intervention for breathlessness in lung cancer.
Palliat Med. 10:299–305. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Bredin M, Corner J, Krishnasamy M, et al:
Multicentre randomised controlled trial of nursing intervention for
breathlessness in patients with lung cancer. BMJ. 318:901–904.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Li FY: Respiratory training to improve
lung cancer patients postoperative pulmonary function and quality
of life. Zhongguo Lin Chuang Kang Fu. 7:41542003.(In Chinese).
|
|
25
|
Zhou ZY, Liu LG, Meng AF and Xia HM: Two
kinds of respiratory training method to improve lung function of
patients with lung cancer influence. Nursing Practice and Research.
9:31–32. 2012.(In Chinese).
|
|
26
|
Fiore JF Jr: Use of breathing exercises
and enforced mobilization after colorectal surgery. Surgery.
151:632–633. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Esbensen BA, Osterlind K, Roer O and
Hallberg IR: Quality of life of elderly persons with newly
diagnosed cancer. Eur J Cancer Care (Engl). 13:443–453. 2004.
View Article : Google Scholar : PubMed/NCBI
|