Introduction
Gorham’s disease (Gorham-Stout syndrome) is a rare
disorder characterized by progressive resorption of the whole or
part of a bone (1–5). It is non-hereditary and often occurs
in individuals aged <40 years without gender-related differences
(6). The pathogenetic mechanism of
Gorham’s disease remains unknown. Phase I of this disease
represents increased vascular concentration in the bone-displacing
fibrous tissues. In phase II, only fibrous tissue is observed
(7,8). There is controversy with regard to
the presence or absence of osteoclasts in this condition. In
certain cases, osteoclastic activity is minimal or non-existent,
whereas in other cases, osteoclasts are easily identifiable
(9). During the past 10 years, we
have identified only 2 cases that were diagnosed as Gorham’s
disease. In the current study, we report one of these cases.
Case report
An eight-year-old male in West China was admitted
with shortness of breath for 10 months. The patient was admitted to
Department of Endocrinology and Metabolism, The Military General
Hospital of Beijing PLA, Beijing, on September 13, 2010.
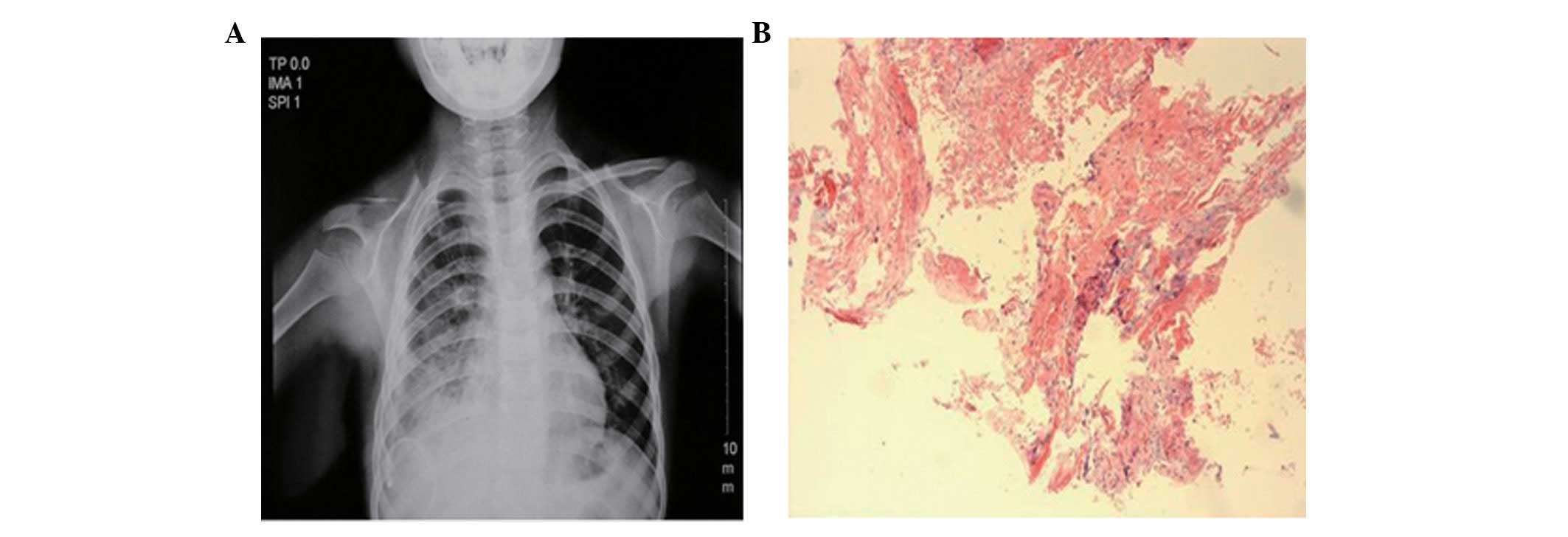
Radiographs revealed the absence of the right clavicle, destruction
of the anterior extremity of the right ribs and pleural effusion of
the right side (Fig. 1A). Bone
scanography indicated that the change in the right clavicle was not
malignant. The biopsy of the right cervical rib revealed
considerable vascular fibrous tissue with certain vessels
distending and shunting together to form sinus construction
(Fig. 1B), in which there was no
endothelial cell proliferation. Masson’s staining revealed the
proliferation of collagen.
Acid-fast bacillia and malignant cells were not
detected in a sample of pleural effusion; however, the Rivalta and
Chyle tests were positive. Other laboratory investigation results
were normal, with the exception of low hemoglobin (93 g/l) and a
slight elevation of the alkaline phosphatase levels (133 U/l). In
the follow-up examination there was no progress of osteolysis of
the skull and the other portion of bone. Prior written and informed
consent were obtained from every patient and the study was approved
by the ethics review board of The Military General Hospital of
Beijing PLA.
Discussion
One case of Gorham’s disease was diagnosed according
to the clinical manifestations, radiological images and the changes
of histopathology. There was no family history of bone disease or
trauma. The portions of bone loss were on the rib cage and
maxillary bone.
The treatment options utilized previously consist of
surgical resection and radiotherapy and mainly target the patient’s
symptoms (6,10–14).
The disparity of the radio-sensitivity of Gorham’s disease-specific
cells has resulted in mixed results following treatment (12–14).
In patients with active osteoclasts, anti-resorptive therapy,
including bisphosphonates or calcitonin, may improve the
progressive osteolytic changes (15–17).
In the current study, radiotherapy was administered
to the patient who was identified to have no osteoclasts when
examined histologically. Despite the report that >15% of
patients succumb due to this disease, the patient was well with no
worsening of the condition. The prognosis depends on complications,
including neurological deficits and pleural effusion (11,18).
Life expectancy is not affected if the extremities are
involved.
References
|
1
|
Gorham LW and Stout AP: Massive osteolysis
(acute spontaneous absorption of bone, phantom bone, disappearing
bone): its relation to hemangiomatosis. J Bone Joint Surg Am.
37:985–1044. 1955.PubMed/NCBI
|
|
2
|
Choma ND, Biscotti CV, Bauer TW, et al:
Gorham’s syndrome: a case report and review of the literature. Am J
Med. 83:1151–1155. 1987.
|
|
3
|
Jackson J: A boneless arm. Boston Med Surg
J. 18:368–369. 1838.
|
|
4
|
Zheng MW, Yang M, Qiu JX, et al:
Gorham-Stout syndrome presenting in a 5-year-old girl with a
successful bisphosphonate therapeutic effect. Exp Ther Med.
4:449–451. 2012.PubMed/NCBI
|
|
5
|
Al-Jamali J, Glaum R, Kassem A, Voss PJ,
Schmelzeisen R and Schön R: Gorham-Stout syndrome of the facial
bones: a review of pathogenesis and treatment modalities and report
of a case with a rare cutaneous manifestations. Oral Surg Oral Med
Oral Pathol Oral Radiol. 114:e23–e29. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hardegger F, Simpson LA and Segmueller G:
The syndrome of idiopathic osteolysis. Classification, review and
case report. J Bone Joint Surg Br. 67:88–93. 1985.PubMed/NCBI
|
|
7
|
Bruch-Gerharz D, Gerharz CD, Stege H, et
al: Cutaneous lymphatic malformations in disappearing bone
(Gorham-Stout) disease: A novel clue to the pathogenesis to a rare
syndrome. J Am Acad Dermatol. 56:S21–S25. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Heffez L, Doku HC, Carter BL, et al:
Perspectives of massive osteolysis: report of a case and review of
the literature. Oral Surg Oral Med Oral Pathol. 55:331–343. 1983.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Dickson GR, Mollan RAB and Carr KE:
Cytochemical localization of alkaline and acid phosphatase in human
vanishing bone disease. Histochemistry. 87:569–572. 1987.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Picault C, Comtet JJ, Imbert JC, et al:
Surgical repair of extensive idiopathic osteolysis of the pelvic
girdle (Jackson-Gorham disease). J Bone Jt Surg Br. 66:148–149.
1984.
|
|
11
|
Hejgaard N and Olsen PR: Massive Gorham
osteolysis of the right hemipelvis complicated by chylothorax:
report of a case in a 9-year-old boy successfully treated by
pleurodesis. J Pediatr Orthop. 7:96–99. 1987.
|
|
12
|
Fontanesi J: Radiation therapy in the
treatment of Gorham disease. J Pediatr Hematol Oncol. 25:816–817.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Dunbar SF, Rosenberg A, Mankin H, et al:
Gorham’s massive osteolysis: the role of radiation therapy and a
review of the literature. Int J Radiat Oncol Biol Phys. 26:491–497.
1993.
|
|
14
|
Hanly JG, Walsh NM and Bresnihan B:
Massive osteolysis in the hand and response to radiotherapy. J
Rheumatol. 12:580–582. 1985.PubMed/NCBI
|
|
15
|
Hagberg H, Lamberg K and Astrom G:
Alpha-2b interferon and oral clodronate for Gorham’s disease.
Lancet. 350:1822–1823. 1997.PubMed/NCBI
|
|
16
|
Hammer F, Kenn W, Wesselmann U, et al:
Gorham-Stout disease - stabilization during bisphosphonate
treatment. J Bone Miner Res. 20:350–353. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Silva S: Gorham-Stout disease affecting
both hands: stabilization during biphosphonate treatment. Hand
(NY). 6:85–89. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bode-Lesniewska B, von Hochstetter A,
Exner GU, et al: Gorham-Stout disease of the shoulder girdle and
cervico-thoracic spine: fatal course in a 65-year-old woman.
Skeletal Radio. 31:724–729. 2002.PubMed/NCBI
|