Introduction
Ischemic colitis is primarily caused by arterial
obstruction secondary to arteriosclerosis, thrombosis or embolism
in the left-sided colon (1).
Mesenteric venous abnormalities may also result in ischemic
colitis, and lead to progressive fibrosis, calcification and
obstruction of the colonic and mesenteric veins (1). Subsequently, the affected colon wall
becomes thickened, which interferes with motility and may lead to
subserosal calcifications and luminal stenosis (1). Ischemic colitis infrequently affects
the right colon and the superior mesenteric vein (SMV).
Phlebosclerotic colitis (PC), also known as
mesenteric phlebosclerosis, is a unique form of ischemic colitis
with <80 reported cases in the literature (2,3).
Calcifications along the wall of colon are the only unique
radiographic feature, and delayed diagnosis may lead to intestinal
gangrene (2,3). The present report describes a case of
PC in a 56-year-old male.
Case report
A 56-year-old male presented with a one-day history
of diffuse abdominal pain, and an absence of stool passage and
occasional nausea and vomiting for one week. The patient’s medical
history was significant for hypertension, which had been controlled
with medication for two years. In addition, the patient had used a
Chinese herbal syrup and alcohol for the relief of intermittent
abdominal pain for >30 years. A similar episode of diffuse
abdominal pain three years previously had resulted in the patient
consulting a doctor; the patient was discharged following imaging
studies and conservative treatment. The study was approved by the
Ethics Committee of the Institutional Review Board of Shin Kong Wu
Ho-Su Memorial Hospital (Taipei, Taiwan). Written informed consent
was obtained from the patient.
Physical examination revealed stable vital signs and
rebound tenderness over the right upper abdomen. Laboratory data,
including biochemistry, electrolytes and a complete blood count,
were all within normal limits, except for mild leukocytosis [white
blood cells (WBCs), 12,600/μl; segmented neutrophils, 70.1%]. An
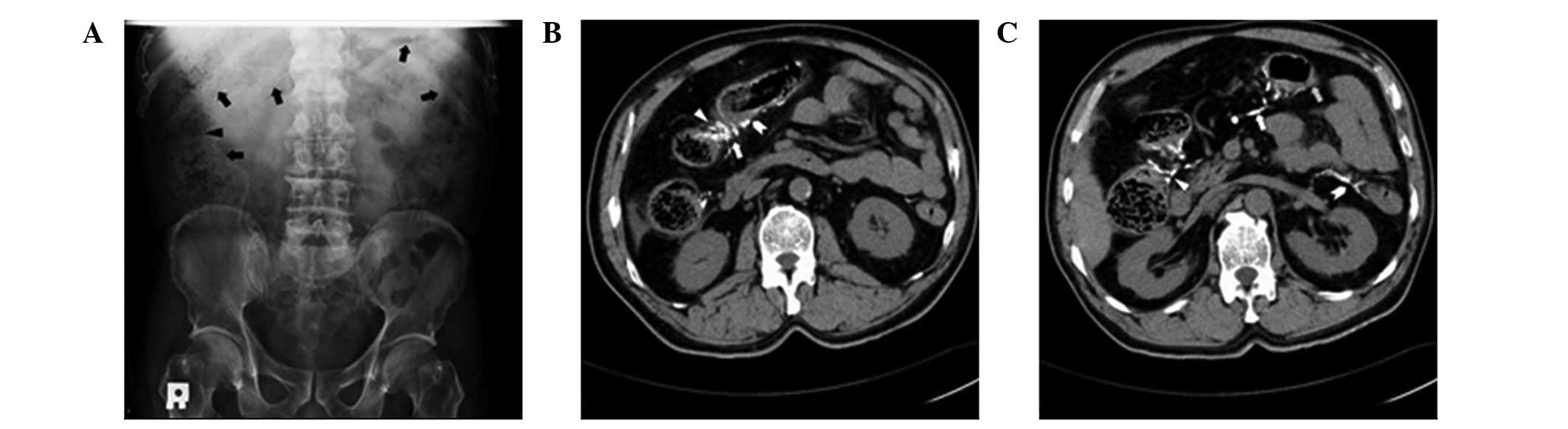
abdominal radiograph revealed thread-like radiopaque densities in
the right upper quadrant (Fig.
1A). Computed tomography (CT) revealed numerous serpentine
calcifications alongside the colonic veins, which extended from the
terminal ileum to the proximal descending colon, ascites, and wall
thickening and luminal stenosis over the hepatic flexure (Fig. 1B and C). Compared with the previous
imaging studies, the extent of the calcifications had become more
severe. Angiography showed a patent superior mesenteric artery
trunk; however, there was decreased arterial perfusion and absent
venous return at the tributary of the ascending colon and hepatic
flexure (Fig. 2).
The patient was admitted and reported increased
abdominal pain and tenderness later that day, and progressive
leukocytosis was observed (WBCs, 18,800/μl; segmented neutrophils,
88.0%). The patient subsequently underwent emergent surgical
intervention with suspected PC and impending ischemia or gangrene
of the colon.
Intraoperatively, ischemic and gangrenous changes
involving almost the entire colon, as well as turbid ascites, were
observed, and a subtotal colectomy was performed. Pathological
examination revealed necrotic changes, erosion and ulceration of
the colonic mucosa, in addition to hemorrhagic and edematous
submucosa with inflammatory cell infiltration in the colon wall. No
obvious perforation was apparent. There were numerous sclerotic
veins or venules with hyalinization, calcification and areas of
ossification in the intramural and extramural aspect of the colon,
and a focal area of near-total occlusion of the venous lumen with
ossification and thrombosis (Fig.
3).
The patient recovered well, and was discharged two
weeks later. He returned to work, and has had no recurrent symptoms
during the subsequent three-year follow-up.
Discussion
The signs and symptoms of PC are nonspecific and may
include abdominal pain, ileus, diarrhea and bloody stools (2). Features of PC may include mesenteric
venous fibrosis, hyalinization, sclerosis and/or calcifications,
ulceration of the colonic mucosa, wall thickening and luminal
stricture (4,5). PC occurs primarily in individuals of
Asian descent. A summary of the patient and disease characteristics
is shown in Table I.
 | Table IDemographics and characteristics of
patients with phlebosclerotic colitis reported from 1991 to
2011. |
Table I
Demographics and characteristics of
patients with phlebosclerotic colitis reported from 1991 to
2011.
|
Demographic/characteristic | Value | % |
|---|
| Country or area
(n=69) |
| Japan | 52 | 75.4 |
| Taiwan | 12 | 17.4 |
| Hong Kong | 2 | 2.9 |
| Korea | 3 | 4.3 |
| Gender (n=63) |
| Male | 34 | 54.0 |
| Female | 29 | 46.0 |
| Age, years
(n=63) |
| Median (range) | 59 (33–77) | NA |
| Symptoms and signs
(n=60) |
| Pain | 45 | 75.0 |
| Diarrhea | 26 | 43.3 |
| Ileus | 17 | 28.3 |
| Nausea/vomiting | 17 | 28.3 |
| Positive stool
occult blood | 12 | 20.0 |
| Constipation | 8 | 13.3 |
| Palpable mass | 3 | 5.0 |
| Fever | 3 | 5.0 |
| Body weight
loss | 3 | 5.0 |
| Fatigue | 1 | 1.7 |
| Location of lesions
(n=62)a |
| Limited to right
colon (cecum and ascending colon) | 4 | 6.5 |
| Continuously
extended to transverse colon | 29 | 46.8 |
| Continuously
extended to left colon (descending and sigmoid colon) | 27 | 43.5 |
| Continuously
extended to rectum | 2 | 3.2 |
| Management
(n=64) |
| Surgical
intervention | 33 | 51.6 |
| Conservative
treatment and subsequent surgery | 5 | 7.8 |
| Conservative
treatment only | 26 | 40.6 |
| Procedure
(n=38)b |
| Right
hemicolectomy | 12 | 31.6 |
| Subtotal
colectomy | 26 | 68.4 |
The condition is mostly neglected during the early
stage of the disease, and the characteristic radiographic feature
is multiple fine tortuous thread-like or serpentine mesenteric
venous calcifications involving the marginal veins, vena recti and
intramural tributaries (3,6). The calcifications are primarily
located perpendicular to the long axis of the colon (3,6), and
may extend to the vicinity of the SMV trunk (2). CT may reveal edematous wall mural
thickening and luminal stricture of the colon, and angiography may
show decreased venous phase perfusion. PC chiefly involves the
right hemicolon, and in certain cases the lesions gradually
progress in a caudal direction (3,6). In
the patient described in the present report, the SMV distribution
of the ascending and proximal transverse colon was affected in
2006, and three years later the lesions had extended to the
proximal descending colon, suggesting a slow disease
progression.
The pathogenesis of PC has not been fully elucidated
(2,5). There have been seven cases of PC
associated with the prolonged use of herbal medications (7,8). In
addition, alcohol and chemicals, such as aristolochic acid or
rolipram, have been associated with blood vessel injuries that lead
to ischemic changes (7,8). The history of the patient in the
present case was significant for the use of a herbal syrup for
>30 years. Of note, there are numerous herbal-infused seasonings
and microorganisms used in the fermenting process of foods commonly
consumed in Asian countries.
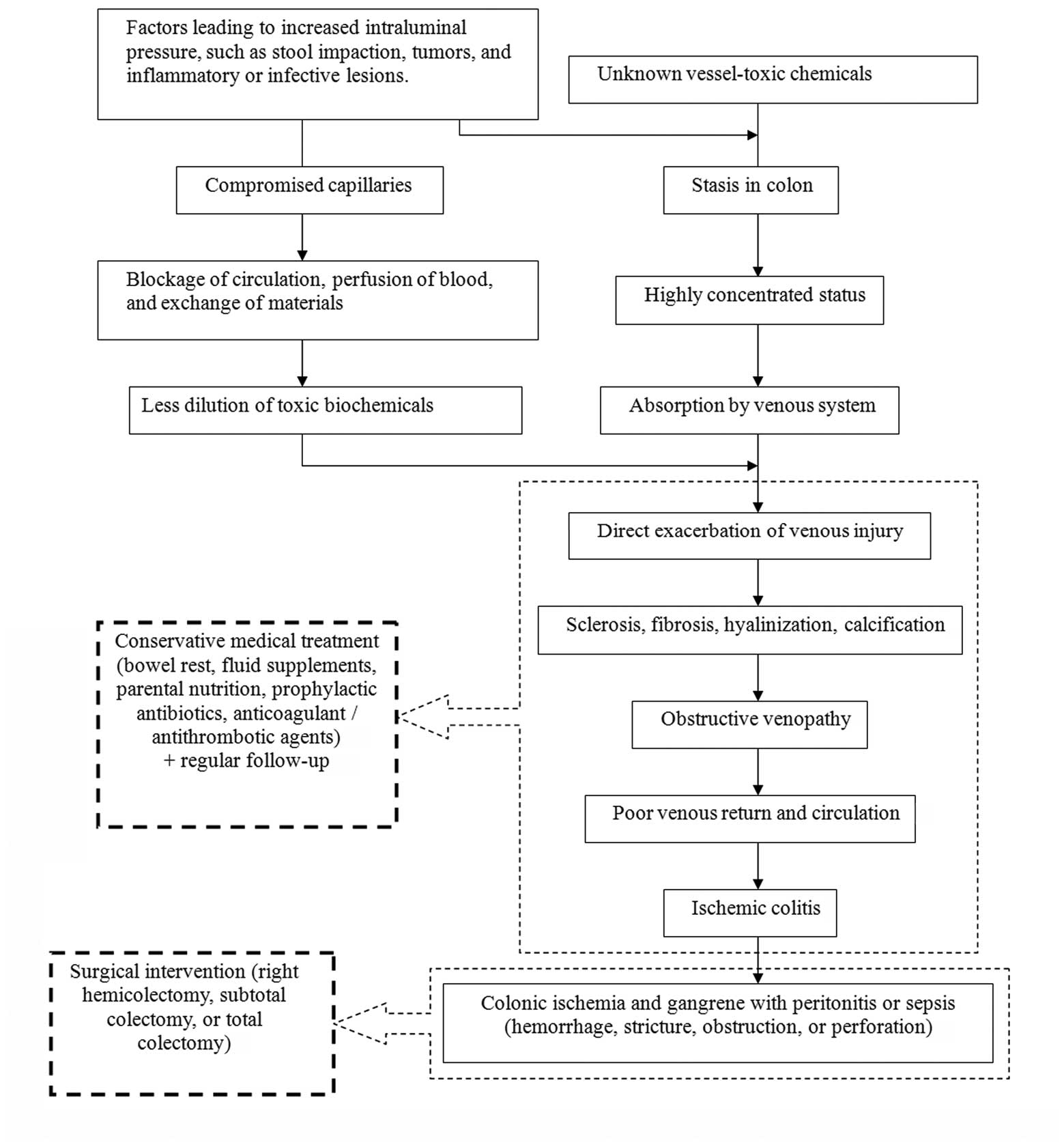
It is unclear why PC primarily affects the
right-sided colon; however, it has been suggested that certain
toxic biochemical agents or water-soluble irritants absorbed from
the ascending colon cause chronic venous damage (7,9).
These substances may remain static longer in the right-sided colon,
and often migrate cephalad (4).
Increased intraluminal pressure in the right-sided colon may be
another possible factor. Genetic susceptibility to PC has also been
proposed, since almost all reported cases of PC are in individuals
of Asian ancestry (4). Based on
our review of the literature, an algorithm of the possible
pathogenic mechanism is shown in Fig.
4.
The management of PC should be based on the severity
of the disease. In addition, the extent and duration of blood
supply deprivation, as well as the degree of the intestinal injury,
should be considered when selecting between surgical and
conservative treatment. Previously, the majority of patients
underwent surgical intervention; however, at present, conservative
management with close follow-up is preferred if there are no signs
of bowel compromise (10).
Hemicolectomy or subtotal or total colectomy is considered curative
therapy with a relatively good prognosis (10).
PC is a rare and potentially life-threatening
condition that is most frequently observed in Asia, and diagnosis
is made by the presence of serpentine calcifications on imaging
studies. Management depends on the severity of disease, ranging
from close follow-up to prompt surgical intervention.
References
|
1
|
Feuerstadt P and Brandt LJ: Colon
ischemia: recent insights and advances. Curr Gastroenterol Rep.
12:383–390. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Iwashita A, Yao T, Schlemper RJ, et al:
Mesenteric phlebosclerosis: a new disease entity causing ischemic
colitis. Dis Colon Rectum. 46:209–220. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kwok KY, Lo SSM, Fung HS, Fan TW and Wong
WK: Mesenteric phlebosclerosis - features on plain radiograph and
computed tomography scan. J HK Coll Radiol. 12:136–138. 2010.
|
|
4
|
Nishimura G, Nagai N, Ninomiya I, et al:
Chronic ischemic lesions of the colon caused by phlebosclerosis of
ileocolic mesenteric vein. Dig Endosc. 16:169–171. 2004. View Article : Google Scholar
|
|
5
|
Mikami T, Hatate K, Kokuba Y, Nemoto Y,
Tanigawa H and Okayasu I: A case of phlebosclerotic colitis:
vasculitis as a possible origin. Kitasato Med J. 35:75–79.
2005.
|
|
6
|
Markos V, Kelly S, Yee WC, Davis JE,
Cheifetz RE and Alsheikh A: Phlebosclerotic colitis: imaging
findings of a rare entity. AJR Am J Roentgenol. 184:1584–1586.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Miyazaki M, Nakamura S and Matsumoto T:
Idiopathic mesenteric phlebosclerosis occurring in a wife and her
husband. Clin Gastroenterol Hepatol. 7:e32–e33. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ho TJ, Cheung CW, Wong WM and Chan FL:
Phlebosclerotic colitis: an unusual cause of ischaemic colitis in a
65-year-old man. J HK Coll Radiol. 8:53–58. 2005.
|
|
9
|
Chang KM: New histologic findings in
idiopathic mesenteric phlebosclerosis: clues to its pathogenesis
and etiology - probably ingested toxic agent-related. J Chin Med
Assoc. 70:227–235. 2007. View Article : Google Scholar
|
|
10
|
Yu CJ, Wang HH, Chou JW, et al:
Phlebosclerotic colitis with nonsurgical treatment. Int J
Colorectal Dis. 24:1241–1242. 2009. View Article : Google Scholar : PubMed/NCBI
|