Introduction
Pathological optic disc cupping (ODC) is frequently
associated with glaucoma and other less common neuro-ophthalmic
conditions (1). Optic atrophy, as
a result of numerous nonglaucomatous diseases, may also lead to
ODC; however, this has received less consideration. Previous
studies have indicated that ~20% of patients were misdiagnosed with
glaucoma (2,3). Nonglaucomatous optic disc cupping
(NGODC) is predominantly attributed to various optic nerve diseases
(4,5); however, may also be a result of
retinal diseases (6). Therefore,
in the present study, patients with NGODC were analyzed based on
data obtained from clinical information and examinations and
certain patients were diagnosed with retinal disorders.
Distinguishing characteristics between glaucomatous optic disc
cupping (GODC) and NGODC are discussed in the present study.
Patients and methods
Patients
Medical records of patients who had been diagnosed
with NGODC at the Chinese General Hospital of PLA (Beijing, China)
between February 2008 and March 2013 were retrospectively reviewed.
Informed consent was obtained from all the patients. In total, 19
eyes from 12 subjects (male, 6; female, 6) were analyzed in this
study. The patient ages ranged between 8 and 63 (mean age, 39
years; Table I). The medical
records of the patients were reviewed and a detailed history of
current and past ophthalmic and systemic illnesses was constructed,
including visual symptoms on presentation and their duration,
medical, family and social histories and any medication previously
prescribed.
 | Table IClinical data of 12 patients with
NGODC. |
Table I
Clinical data of 12 patients with
NGODC.
| Case no. | Gender | Age (years) | Diagnosis | Eye | Duration of
diseasea | Morphology of
cupping | BCVAb | Visual field
defect |
|---|
| 1 | F | 41 | Neuromyelitis
optica | OS | 2 years | Diffuse | OD 0.2, OS
FC/20 cm | Central scotoma |
| 2 | M | 18 | LHON | OU | 2 years | Diffuse | OD 0.1, OS 0.05 | Central scotoma |
| 3 | F | 62 | CLRAO, CRVO | OD | 10 months | Diffuse | OD 0.15, OS 0.25 | Inferior defect |
| 4 | M | 26 | Pituitary
adenoma | OU | 10 months | Bilateral nasal (more
serious OD) | OD 0.8, OS 0.8 | Bitemporal
hemianopsia |
| 5 | F | 31 | Cerebral
hemorrhage | OU | 13 months | Temporal OS, nasal
OD | OD 1.0, OS 1.0 | Bilateral homonymous
hemianopia in the right side |
| 6 | M | 55 | Optic neuritis | OD | 1 year | Diffuse | OD 0.3 | Diffuse defect |
| 7 | M | 47 | Optic neuritis | OU | 10 months | Diffuse | OD 1.0, OS 0.12 | Diffuse defect OS,
more serious superiorly. Superior defect OD |
| 8 | F | 8 | Optic neuritis | OU | 6 months | Diffuse | OD 0.8, OS 0.8 | Diffuse defect, more
serious peripherally |
| 9 | F | 48 | Optic neuritis | OS | 1 year | Diffuse | 0.1 | Unknown |
| 10 | M | 39 | Pituitary
adenoma | OU | 2 years | Diffuse | OD 1.2, OS
HM before eye | Diffuse defect
OS
Nasal hemianopia OD |
| 11 | F | 30 | Optic nerve
injury | OU | 2 years | Diffuse | NLP, OU | Unavailable |
| 12 | M | 63 | CRAO | OD | 3 months | Diffuse | 0.1 | Diffuse defect |
Ophthalmic evaluation
Patients underwent a detailed ophthalmic evaluation
with particular focus on visual acuity, visual fields, relative
afferent pupillary defects, slit-lamp (Topcon Inc., Tokyo, Japan)
examinations of the anterior segment, lens and vitreous,
intraocular pressure (IOP) (Canon Non-Contact Tonometer; Canon
Inc., Tokyo, Japan), ocular movements and fundus evaluation by
indirect and direct ophthalmoscopy (also by contact lens if
required), as well as additional clinical parameters. Color fundus
images (Canon CX-1 fundus camera; Canon Inc., Tokyo, Japan),
fluorescein fundus angiography (Heidelberg Retina Tomograph HRT-3;
Heidelberg Engineering, Inc., Heidelberg, Germany), optical
coherence tomography (Zeiss Cirrus 4000 OCT, Carl Zeiss Meditec,
Inc., Dublin, CA, USA), perimetry (Humphrey 740i Field Analyzer,
Carl Zeiss Meditec, Inc.) and visual electrophysiology (Roland
Electrophysiological diagnostic systems; Roland Consult, Stasche
& Finger GmbH, Brandenburg an der Havel, Germany) were also
performed.
Statistical analysis
SPSS 19.0 software (SPSS, Inc., Chicago, IL, USA)
was used for statistical analysis. The correlation between IOP and
the cup/disc (C/D) ratio was analyzed and compared with analysis of
variance. In addition, the data were analyzed using a curve fitting
model.
Results
Analysis of morphology and clinical
data
Of the 12 cases, none were diagnosed with glaucoma,
four exhibited optic neuritis, one had Devic’s disease, one had
Leber’s hereditary optic neuropathy (LHON), two had a pituitary
adenoma, one had a basal ganglia cerebral hemorrhage, one exhibited
cilioretinal artery occlusion (CLRAO) associated with central
retinal vein occlusion (CRVO), one exhibited central retinal artery
occlusion (CRAO) and the remaining patient exhibited optic nerve
injuries. The clinical data are described in Table I and selected cases are detailed as
follows (the case number refers to the patient number in Table I).
The mean IOP of the affected eyes of the 12 subjects
was 14.5±3.8 mmHg (n=19), as compared with the healthy eyes that
had a mean IOP of 14.4±1.3 mmHg (n=5). There was no statistically
significant difference (F=4.30; P=0.892). The mean C/D ratio in the
affected eyes was 0.83±0.10 and 0.38±0.01 in the healthy eyes
(F=4.30; P<0.01). There was no correlation between IOP and the
C/D ratio (correlation coefficient, 0.184; P>0.05).
Representative cases
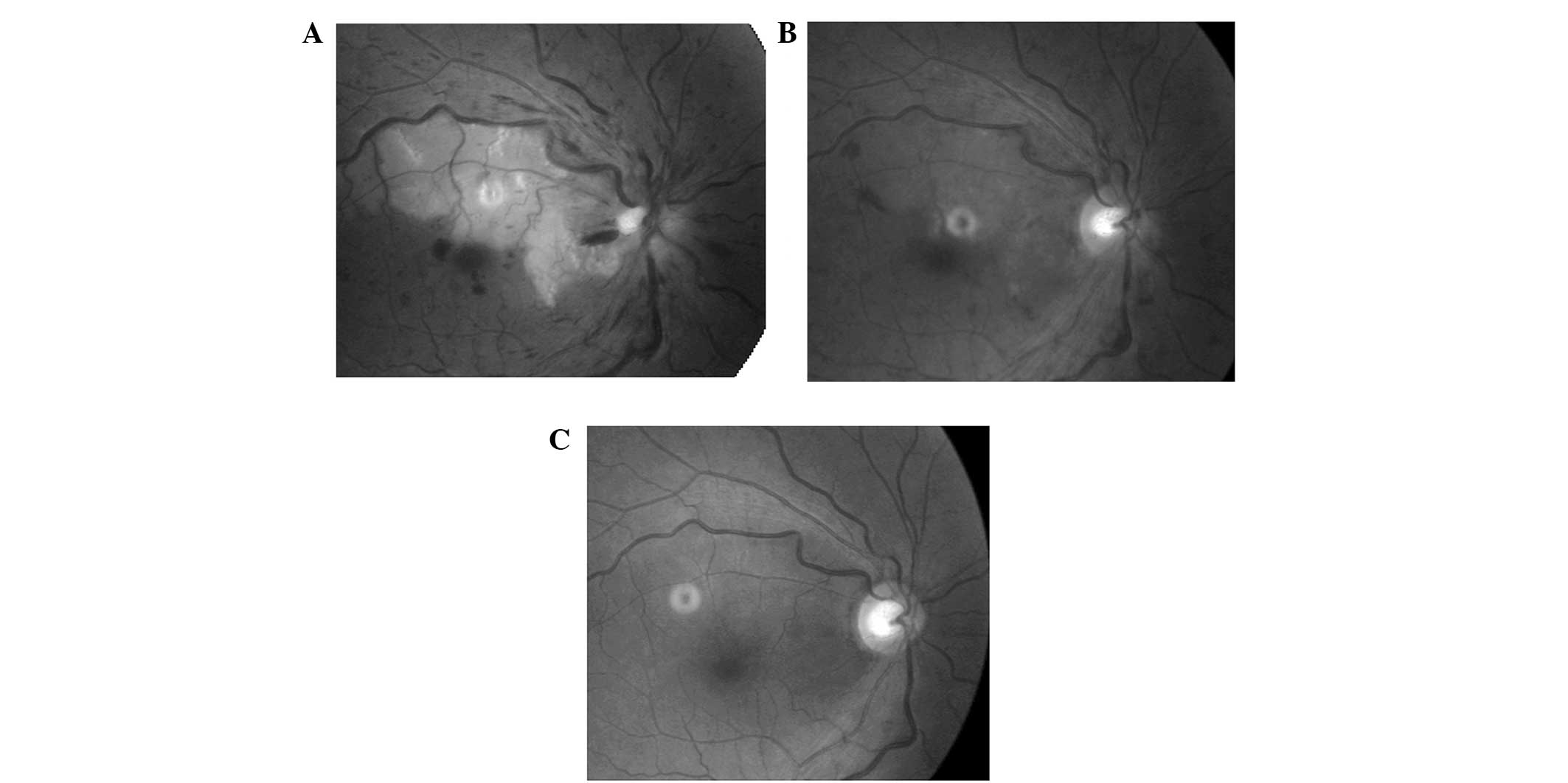
Case 2
An 18-year-old male complained of a sequential
decrease in binocular vision over two years. IOPs were 16 mmHg
oculus dexter (OD) and 14 mmHg oculus sinister (OS).
The patient was diagnosed with LHON that had been caused by a
11778A mtDNA mutation. Bilateral optic disc appearance was
characterized via diffuse excavation of the optic cup and rim
pallor (Fig. 1). A central scotoma
was the predominant visual field defect observed.
Case 3
A 62-year-old female with CLRAO and CRVO of the
right eye exhibited increasing excavation of the cup with superior
and inferior rim loss. Temporal rim pallor was identified in the
follow-up examinations (Fig. 2).
IOP was 15 mmHg OD.
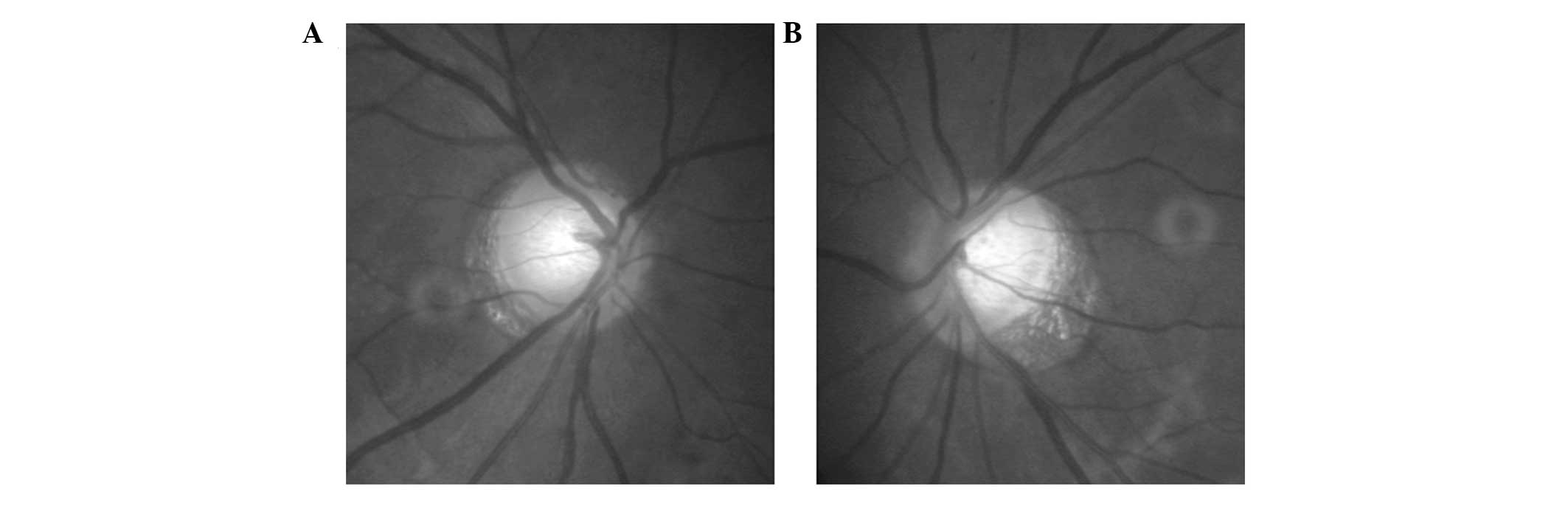
Case 5
A 31-year-old female complained of a visual field
defect of the right eye over a six-month period. IOPs were 14 mmHg
OD and 14 mmHg OS. A magnetic resonance imaging scan revealed a
hemorrhage in the left basal ganglia, which also involved the left
cerebral peduncle and basal ganglia. Left temporal and right nasal
disc pallor and rim loss were observed with the corresponding
visual field defect of right homonymous hemianopia (Fig. 3).
Case 7
A 47-year-old male experienced decreased vision in
both eyes for ten months. The patient had been diabetic for three
years. IOPs were 17 mmHg OD and 16 mmHg OS. Optic disc excavation
and disc pallor were identified in both eyes, but was more serious
in the left eye (Fig. 4). The
patient exhibited congenital physiological ODC with disc pallor as
a result of optic atrophy following optic neuritis.
Discussion
A strong association was observed between
neuro-ophthalmic diseases and pathological ODC in the present
study. In addition to glaucoma, other retinal diseases contribute
to NGODC (6). Retinal and optic
nerve head diseases are often associated with NGODC, including
arteritic anterior ischemic optic neuropathy (AION; 7–10), which is
the most common cause despite being rarely observed in China. In
the present study, one patient with CLRAO and CRVO also exhibited
NGODC, which to the best of our knowledge, is the first such case
to be reported in literature. Furthermore, optic neuropathies may
lead to NGODC, including LHON, autosomal dominant hereditary optic
atrophy, optic neuritis, toxic optic neuropathy (e.g. methanol
poisoning) and traumatic neuropathy. In addition, chiasmatic
diseases and other diseases, including anterior segmental optic
nerve compression, cerebrovascular diseases, radiation optic
neuropathy and carotid artery stenosis, occasionally lead to NGODC
(6). Previous studies have focused
on other causes, such as retrograde transsynaptic degeneration of
retinogeniculate axons following periventricular leukomalacia
(11), physiological cupping and
nonglaucomatous optic atrophy, which are additional manifestations
of NGODC.
A normal optic disc usually forms a vertical oval
shape with a vertical diameter that is 7–10% greater than the
horizontal diameter. The optic cup is horizontally oval, thus, the
horizontal C/D ratio is larger than the vertical C/D ratio. In
healthy individuals, the median C/D ratio value is <0.3 and the
difference in the C/D ratios between the fellow eye is <0.2.
Therefore, a ratio greater than 0.6 is indicative of ODC. The color
of a normal rim is orange due to the presence of capillaries. In
the majority of cases, a normal width follows the inferior,
superior, nasal, temporal (ISNT) rule, thus, the neuroretinal rim
is broadest in the inferior disc region, followed by the superior
disc region, the nasal disc area and finally the temporal disc
portion. However, violation of the ISNT rule also occurs in large
optic disc cups of nonglaucomatous origin, with a greater frequency
in the pediatric population (12).
Changes in the optic disc as a result of glaucoma
include focal or concentric enlargement, where the vertical
diameter change is disproportionate to the horizontal change.
Additional traits include deepened excavation, increased exposure
of the lamina cribrosa, diffuse rim loss, wedge-shaped nerve fiber
layer defects, flame-shaped disc hemorrhages and beta zones of
parapapillary atrophy in accordance with nerve fiber layer defects
(13).
Several key differences were observed between NGODC
and GODC (14–16). Firstly, the color of the rim is the
most important. The rim of NGODC often exhibits pallor, while the
rim in GODC is pink. However, differentiating between NGODC and
GODC according to rim color is very difficult in end-stage glaucoma
when the C/D ratio is ~1.0. Secondly, the presence of focal or
diffuse rim loss is important. Focal rim loss is predominantly
associated with glaucoma, while eyes with nonglaucomatous diseases
are often characterized by diffuse rim loss. Although focal rim
loss may occasionally be present in NGODC, total loss of the disc
rim is never observed. Thirdly, there is a high correlation between
visual field defects and disc changes in GODC, but a marginal
correlation between these parameters in NGODC (4,14,15).
Fourthly, IOP may or may not be within the normal range. Fifthly,
ODC is apparent prior to visual field defects in GODC. Visual
acuity decreases markedly in NGODC with apparent visual field
losses, but with marginal associated changes in the optic cup.
Finally, peripapillary atrophy is an increasingly common
observation in GODC as compared with NGODC.
Physiological cupping is a congenital disorder of
optic cupping, which is caused by the scleral optic canal and
pronounced glial atrophy of Bergmeister’s papilla. GODC is a type
of ascending optic nerve atrophy that is associated with the loss
of retinal ganglion cell axons. These changes extend anterogradely
(upwards) along the pathological axons, which is followed by
neuroretinal rim loss and increased exposure of the lamina
cribrosa. In eyes exhibiting glaucomatous damage, rim loss is
predominantly identified in the inferior and superior disc regions,
thus, cupping is prone to vertical expansion. Focal or diffuse rim
loss is associated with the distribution of nerve fibers and the
impaired area. NGODC, resulting from optic nerve diseases, is an
abnormality of retrograde (descending) optic atrophy, the
mechanisms of which include prelaminar tissue atrophy, postlaminar
tissue fibrosis, the shrinkage of fiber longitudinales, glial
hyperplasia, bowing back of the lamina cribrosa following loss of
support and damage to the laminar neurological and connective
tissue caused by ischemia (7).
Eyes with non-arteritic AION (NA-AION) do not
develop ODC. Patients with NA-AION usually exhibit a small or no
optic cup, which may contribute to the pathology (7). However, the damage and atrophy of
retinal ganglion cell axons in NA-AION is not as serious as that
observed in arteritic AION, in which occlusion of the posterior
ciliary arteries is a key event in pathogenesis and results in
greater diffuse damage (7).
In conclusion, the key differentiating features
between NGODC and GODC are the optic disc rim color and the
correlation between visual field defects and the disc appearance.
Focal rim loss also aids with distinguishing between the two
diseases. However, methods of distinguishing NGODC from GODC should
rely on patient history, visual field assessment and clinical data.
Physicians and ophthalmologists are required to be vigilant to
uncommon and potentially threatening forms of NGODC.
Acknowledgements
The study was supported by a grant from the
12th five-year National Sci-Tech Support Plan for the
Clinical Research of Optic Neuritis, China (no. 2012BAI08B06).
Abbreviations:
|
ODC
|
optic disc cupping
|
|
GODC
|
glaucomatous optic disc cupping
|
|
NGODC
|
nonglaucomatous optic disc cupping
|
|
IOP
|
intraocular pressure
|
|
C/D
|
cup/disc ratio
|
|
LHON
|
Leber’s hereditary optic
neuropathy
|
|
CLRAO
|
cilioretinal artery occlusion
|
|
CRVO
|
central retinal vein occlusion
|
|
CRAO
|
central retinal artery occlusion
|
|
OD
|
oculo dextro
|
|
OS
|
oculus sinister
|
|
AION
|
anterior ischemic optic neuropathy
|
|
ISNT
|
inferior, superior, nasal,
temporal
|
|
NA-AION
|
non-arteritic anterior ischemic optic
neuropathy
|
References
|
1
|
Ambati BK and Rizzo JF III:
Nonglaucomatous cupping of the optic disc. Int Ophthalmol Clin.
41:139–149. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Piette SD and Sergott RC: Pathological
optic-disc cupping. Curr Opin Ophthalmol. 17:1–6. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Trobe JD, Glaser JS, Cassady J, Herschler
J and Anderson DR: Nonglaucomatous excavation of the optic disc.
Arch Ophthalmol. 98:1046–1050. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Golnik K: Nonglaucomatous optic atrophy.
Neurol Clin. 28:631–640. 2010. View Article : Google Scholar
|
|
5
|
Bianchi-Marzoli S, Rizzo JF III, Brancato
R and Lessell S: Quantitative analysis of optic disc cupping in
compressive optic neuropathy. Ophthalmology. 102:436–440. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Roodhooft JM: Nonglaucomatous optic disk
atrophy and excavation in the elderly. Bull Soc Belge Ophtalmol.
287:45–49. 2003.PubMed/NCBI
|
|
7
|
Hayreh SS and Jonas JB: Optic disc
morphology after arteritic anterior ischemic optic neuropathy.
Ophthalmology. 108:1586–1594. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Girkin CA, De Leon-Ortega J and Graf CM:
Optic disc morphology after AAION. Ophthalmology. 109:1198–1201.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Danesh-Meyer HV, Savino PJ and Sergott RC:
The prevalence of cupping in end-stage arteritic and nonarteritic
anterior ischemic optic neuropathy. Ophthalmology. 108:593–598.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
McLeod D: Optic disc morphology after
AAION. Ophthalmology. 109:1201–1204. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Brodsky MC: Periventricular leukomalacia:
an intracranial cause of pseudoglaucomatous cupping. Arch
Ophthalmol. 119:626–627. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pogrebniak AE, Wehrung B, Pogrebniak KL,
Shetty RK and Crawford P: Violation of the ISNT rule in
nonglaucomatous pediatric optic disc cupping. Invest Ophthalmol Vis
Sci. 51:890–895. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jonas JB and Budde WM: Diagnosis and
pathogenesis of glaucomatous optic neuropathy: morphological
aspects. Prog Retin Eye Res. 19:1–40. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lee AG: Differentiating glaucomatous from
nonglaucomatous optic atrophy. Ophthalmology. 106:8551999.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Greenfield DS: Glaucomatous versus
nonglaucomatous optic disc cupping: clinical differentiation. Semin
Ophthalmol. 14:95–108. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Greenfield DS, Siatkowski RM, Glaser JS,
Schatz NJ and Parrish RK II: The cupped disc. Who needs
neuroimaging? Ophthalmology. 105:1866–1874. 1998. View Article : Google Scholar : PubMed/NCBI
|