Introduction
Endovascular treatment may be used for relatively
simple, short lesions in peripheral arterial occlusive disease
(PAOD) whereas open surgery is typically used for long segment
lesions. According to the TransAtlantic Society Consensus (TASC) II
guidelines, published in 2007 (1),
relatively short ‘A’ lesions should be treated by endovascular
procedures, whereas relatively long ‘D’ lesions should be treated
with open surgery. For ‘B’ lesions, since endovascular methods
offer sufficiently good results, this approach is preferred, unless
an open revascularization is required for other associated lesions
in the same anatomic area. The treatment of ‘C’ lesions with open
revascularization procedures produces superior long-term results;
therefore, endovascular methods should only be used in patients at
high risk for open revascularization.
Multilevel involvement is typically observed in
PAOD. A staged approach to multilevel occlusive disease was the
standard for numerous years, with balloon angioplasty of the iliac
artery followed at an interval by infrainguinal surgery (2,3).
This approach was a rational strategy at a time when open and
endovascular surgical techniques were only performed in separate
settings.
Multilevel revascularization, using a combination of
endovascular and open (hybrid) surgeries, was first reported in the
early 1990s (4). Hybrid surgery is
ideal for multilevel lesions, as it allows for minimally invasive
treatment on complex anatomy in medically high-risk patients.
Examples of multimodal and multilevel vascular reconstructions are
common femoral endarterectomy combined with open iliac artery
transluminal angioplasty and stent placement (5,6), or
infrainguinal bypass originated distal to an iliac or superficial
femoral artery (SFA), percutaneous transluminal angioplasty and
stent (7). Usually the procedures
are performed simultaneously, although individual patient anatomy
plays a part in the decision of whether to perform the two
procedures simultaneously or not.
The aim of the present study was to report a novel
hybrid surgery for lesions involved in multilevel lower extremity
arteries and to evaluate the clinical outcomes.
Materials and methods
Patients
Consecutive patients from the Kyung Hee University
Hospital at Gangdong (Seoul, Korea) were selected between March
2009 and February 2012. This study was approved by the
Institutional Review Board (the Kyung Hee University Hospital at
Gangdong). Written informed consent for the procedure was obtained
from all the patients or their families. Each patient had disabling
claudication or critical limb ischemia (Rutherford category 3 and
4–6, respectively) and underwent revascularization by open surgery
(open group) or by a combination of open surgery and an
endovascular procedure (hybrid group). The patients were
retrospectively analyzed using a prospectively collected
database.
Demographic and clinical characteristics of the
patients were recorded, including comorbidities (hypertension,
diabetes, smoking, coronary artery disease, cerebrovascular
disease, chronic obstructive pulmonary disease, hyperlipidemia and
chronic renal failure), clinical presentation, imaging studies,
procedural details and condition on last follow-up. Preoperatively,
all patients underwent computed tomography-angiography (CTA) for
the evaluation of lower extremity arterial occlusive lesions.
Treatment modality was determined by the vascular surgeon based on
the CTA images. Endovascular procedures were performed for lesions
of TASC classifications A and B whilst open surgeries were
performed for lesions of TASC classification C and D and at lesions
of joint portion.
Surgical procedures
Procedures were performed by a vascular surgeon in
an operating room. Open surgeries were performed with standard
techniques, whilst hybrid surgeries were performed using the BV
Pulsera system (Philips, Andover, MA, USA) for fluoroscopic
imaging. In hybrid cases with iliac occlusions, crossing the lesion
in a retrograde fashion following common femoral artery (CFA)
exposure was attempted. When retrograde access failed, the iliac
occlusion was crossed in an antegrade fashion and the guidewire was
retrieved through the arteriotomy site during endarterectomy or
bypass surgery. Self-expandable stents were preferentially used in
iliac artery lesions.
In patients who required a femoral endarterectomy
and SFA, the SFA lesion was initially crossed in an antegrade
fashion following the exposure of the CFA. Angioplasty and/or
stenting and femoral endarterectomy followed. Next, the arteriotomy
was closed with standard patch angioplasty using the branch of the
ipsilateral great saphenous vein.
Patients typically received 3,000–5,000 units
heparin following the placement of a sheath, which was not reversed
at the end of the procedure. Following surgery, all patients were
administered 75 mg clopidogrel for a minimum of 90 days and 100 mg
enteric coated acetyl salicylic acid for the rest of their
lives.
Postoperative surveillance
Technical success for an endovascular procedure was
defined as a patent vessel with <30% residual stenosis,
following postdilatation with restoration of rapid antegrade
perfusion. Postoperative surveillance was performed in outpatient
clinics at 3 and 6 months and every 6 months thereafter. Clinical
assessments of the femoral and distal pulses, ankle-brachial index
(ABI) measurements and duplex scanning or CTA were performed when
clinically indicated. Loss of patency was defined as a reduction in
the ABI of >0.15 or significant stenosis on duplex scanning or
CTA.
Statistical analysis
Data were analyzed using SPSS 19.0 software (SPSS,
Inc., Chicago, IL, USA). Kaplan-Meier analysis was used to compare
the primary and secondary patency rates of the groups on an
intent-to-treat basis. Continuous variables are presented as mean ±
SD. Demographic comparisons were performed using Fisher’s exact
test for categorical variables and by Mann-Whitney U test for
continuous variables. P<0.05 was considered to indicate a
statistically significant difference.
Results
Patient demographics
A total of 76 patients were included in the study.
Demographic and preoperative characteristics of the patients are
shown in Table I. The mean age was
67.1±11.3 years (range, 42–94 years) and the male-to-female ratio
was 67:9. The most common indication for revascularization was
Rutherford category IV (resting pain) and hypertension was the most
common comorbidity. Table II
shows demographic and preoperative characteristics of the open and
hybrid groups. Age, indication for revascularization and
comorbidities were similar between the open and hybrid groups. The
follow-up period was significantly longer in the open group
compared with that in the hybrid group.
 | Table IPatient demographics (n=76). |
Table I
Patient demographics (n=76).
| Characteristics | Patients |
|---|
| Age, years
(range) | 67.1±11.3
(42–94) |
| Gender,
male:female | 67:9 |
| Follow-up, months
(range) | 10.4±9.4 (0–32) |
| Clinical severity, n
(%) |
| Disabling
claudication | 17 (22.4) |
| Resting pain | 45 (59.2) |
| Tissue loss | 14 (18.4) |
| Risk factors, n
(%) |
| Hypertension | 52 (68.4) |
| Diabetes | 39 (51.3) |
| Smoking | 27 (35.5) |
| Coronary artery
disease | 12 (15.8) |
| Cerebrovascular
disease | 11 (14.5) |
| COPD | 6 (7.9) |
| Hyperlipidemia | 4 (5.3) |
| Chronic renal
failure | 4 (5.3) |
 | Table IIPatient demographics (n=76). |
Table II
Patient demographics (n=76).
| Characteristics | Open group
(n=55) | Hybrid group
(n=21) | P-value |
|---|
| Age, years | 65.7±11.8 | 71.1±8.8 | 0.076 |
| Gender, male:
female | 50:5 | 17:4 | |
| Follow-up,
months | 13.5±10.1 | 4.1±4.3 | <0.0001 |
| Clinical severity, n
(%) | | | 0.479 |
| Disabling
claudication | 12 (21.8) | 5 (23.8) | |
| Resting pain | 35 (63.6) | 10 (47.6) | |
| Tissue loss | 8 (14.6) | 6 (28.6) | |
| Risk factors, n
(%) |
| Hypertension | 33 (60.0) | 19 (90.5) | 0.432 |
| Diabetes | 25 (45.5) | 14 (66.7) | 0.534 |
| Smoking | 20 (36.4) | 7 (33.3) | 0.158 |
| Coronary artery
disease | 6 (10.9) | 6 (28.6) | 0.613 |
| Cerebrovascular
disease | 5 (9.1) | 6 (28.6) | 0.629 |
| COPD | 2 (3.6) | 4 (19.0) | 0.521 |
| Hyperlipidemia | 2 (3.6) | 2 (9.5) | 0.305 |
| Chronic renal
failure | 2 (3.6) | 2 (9.5) | 0.305 |
Hybrid and endovascular surgeries
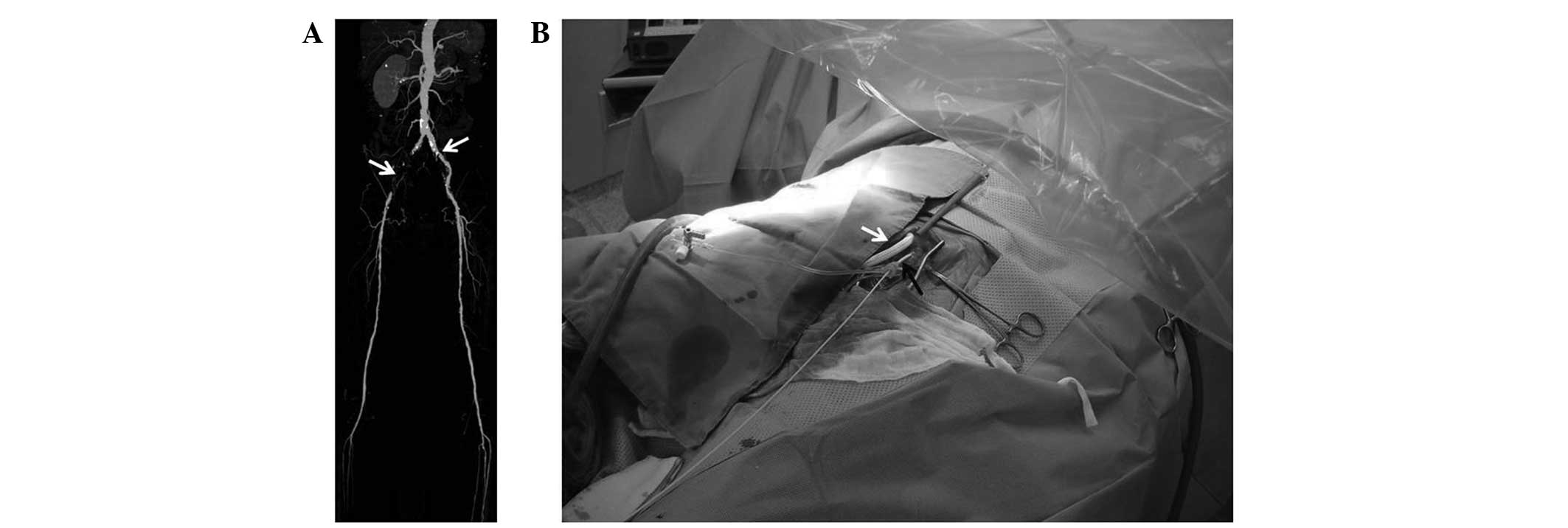
The most common hybrid procedure was a combination
of femoral endarterectomy and iliac stenting (Fig. 1). In the case shown, preoperative
CTA showed tight, calcified stenosis of the right CFA, as well as
bilateral common iliac stenosis (Fig.
1A). Iliac stenting was followed by exposure of the femoral
artery. After the endovascular procedure, routine endarterectomy
and patch closure was performed (Fig.
1B). Postoperative CTA showed a widely opened right CFA and
patent iliac stent (Fig. 1C).
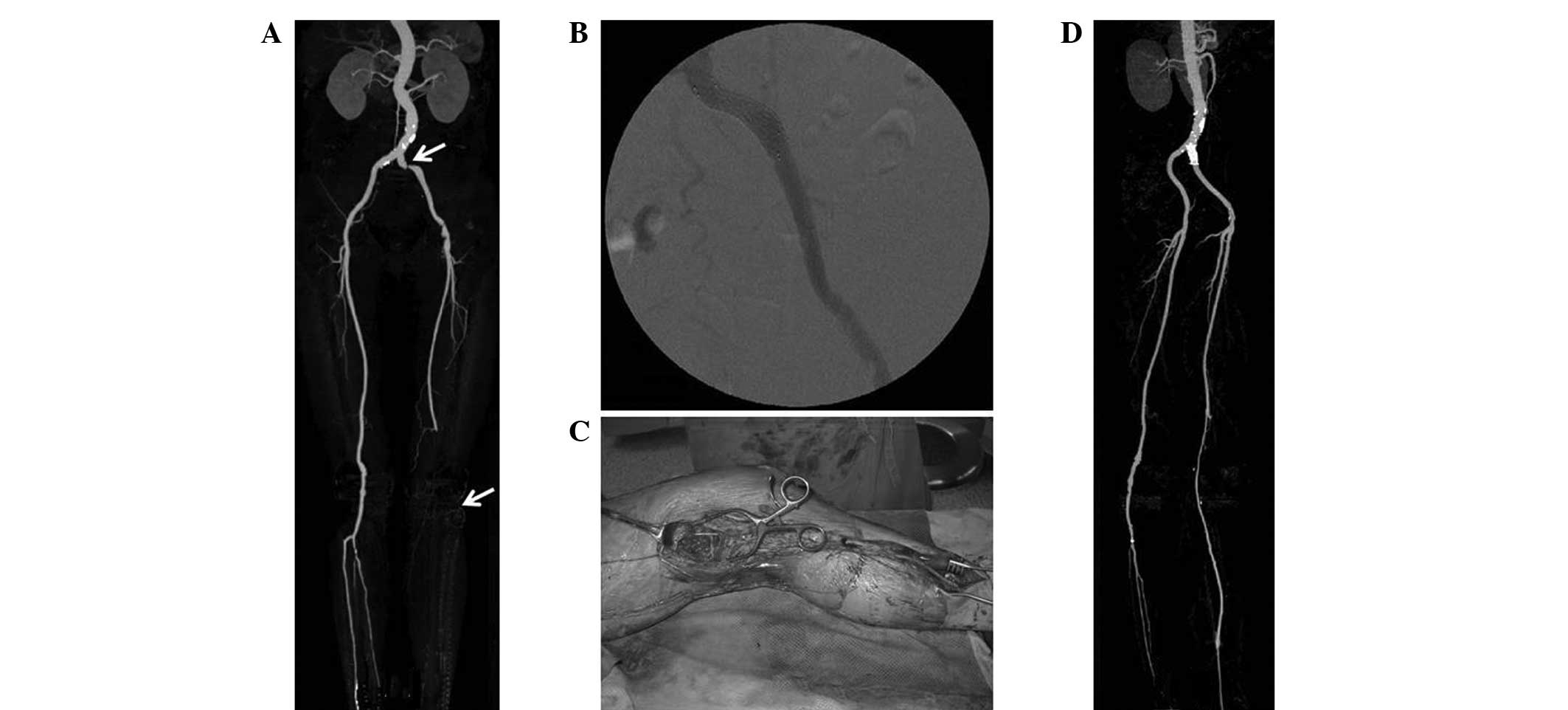
Another frequently performed hybrid surgery is shown
in Fig. 2. Unilateral iliac
stenting and crossover femorofemoral bypass was performed in
patients with TASC classification A unilateral iliac artery
stenosis and TASC classification C or D contralateral iliac
occlusion. A typical CTA image is shown in Fig. 2A. For these patients, the bilateral
femoral artery was first exposed and tunneling was conducted using
a conventional tunneler. Next, the artificial graft was placed in
the tunneled portion and intravenous heparin was injected to
minimize bleeding. The endovascular procedure followed and finally,
bypass surgery was performed. The artificial graft for crossover
femorofemoral bypass and the introducer sheath for endovascular
procedure is shown in Fig. 2B.
Fig. 3 shows an example of the
iliac stenting and distally originated bypass used in patients with
combined lesions comprising a TASC classification A iliac lesion
and C or D lesions below the knee arteries. Fig. 4 shows an example of endarterectomy
of the proximal femoral artery and endovascular procedure for TASC
classification A or B lesions of the SFA.
Procedural details for hybrid surgery are shown in
Table III. The most common open
surgery was femoral endarterectomy and patch closure, whilst for
endovascular surgery, ipsilateral or bilateral iliac stenting was
the most common.
 | Table IIIOpen and endovascular procedures in
hybrid surgery (n=21). |
Table III
Open and endovascular procedures in
hybrid surgery (n=21).
| Type of
procedure | Number |
|---|
| Open procedure |
| Femoral
endarterectomy with patch angioplasty | 7* |
| Femoropopliteal
bypass | 6 |
| Crossover
femorofemoral bypass | 5 |
| Femorotibial
bypass | 3 |
| Popliteo-tibial
bypass | 1 |
| External-to-internal
iliac artery bypass | 1 |
| Endovascular
procedure |
| Ipsilateral iliac
stent | 15 |
| Bilateral iliac
stent | 2 |
| Infrainguinal
PTA | 2 |
| SFA subintimal
angioplasty and stent | 1 |
| Aneurysm repair
using stent-graft | 1 |
Success rates
The immediate technical success rate of hybrid
surgery was 90.5%. There were two technical failures in the hybrid
group. It was not possible to cross over the severely calcified
bilateral iliac arteries in one patient, which necessitated
unilateral iliac stenting and a crossover femorofemoral bypass. The
second patient had a flow-limiting dissection of the SFA during
balloon angioplasty, which required bail-out stenting. The
ipsilateral ABI increased from 0.53±0.21 to 0.75±0.16 in the hybrid
group (P=0.024). This difference was identified to be statistically
significant.
The mean follow-up duration was 10.4±9.4 months
(range, 0–32 months) in the two groups and the mortality rate was
6.6%. Three patients succumbed to myocardial infarction, one to
overwhelming sepsis and one to intracranial hemorrhage. The overall
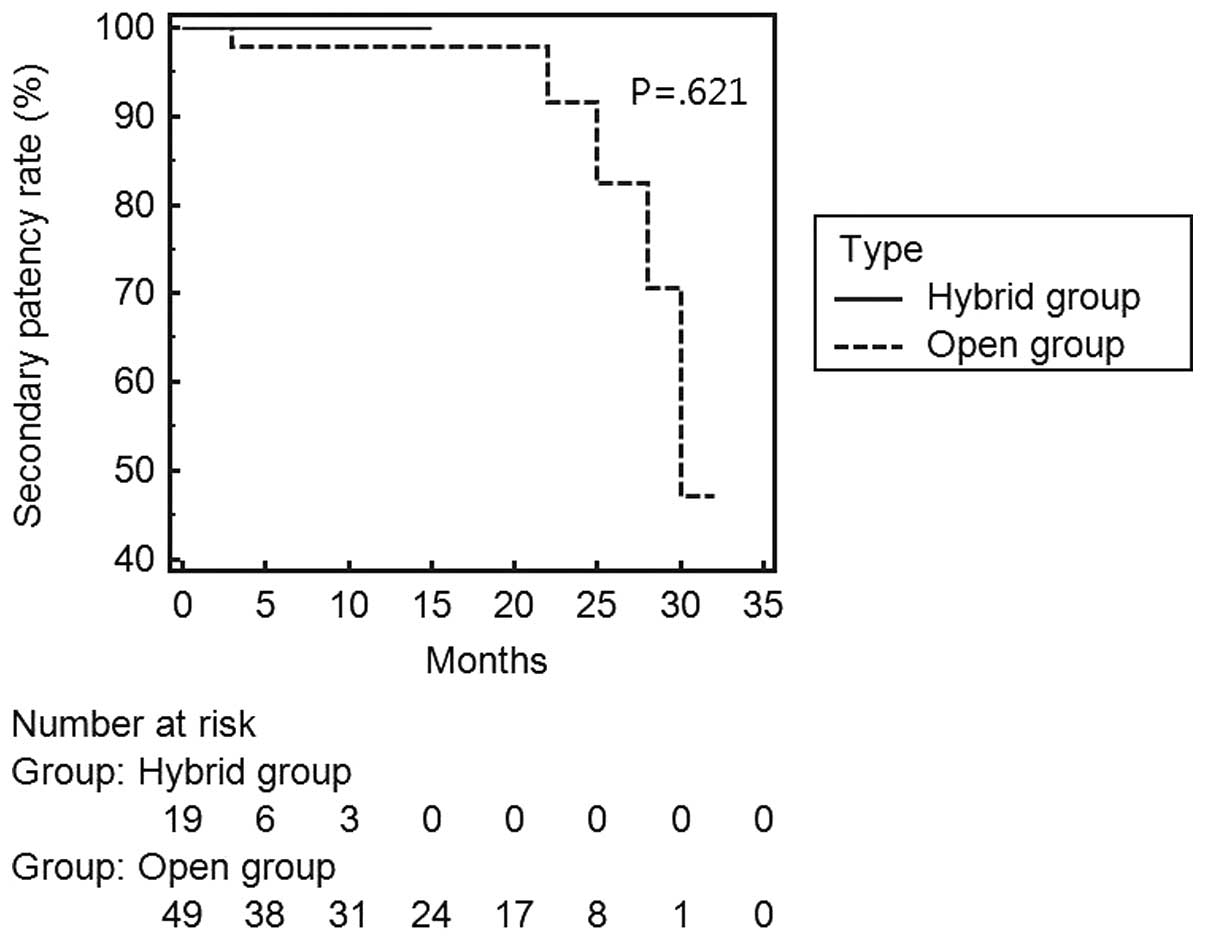
limb salvage rate was 97.4%. The primary patency rates of the
hybrid and open groups are shown in Fig. 5. In the hybrid group, all
revascularized arteries were patent during the follow-up period. In
the open group, 50/55 (90.9%) were patent at the mean follow-up of
10.4 months; however, the difference between the groups was not
statistically significant (P=0.441). Secondary patency rates showed
a similar result (Fig. 6).
Discussion
Combined open and endovascular revascularization may
be performed with a staged or simultaneous approach. Endovascular
surgery has been enthusiastically embraced by a number of vascular
surgeons, leading to increased experience with endovascular
interventions. In numerous hospitals, hybrid operating rooms have
been constructed where open and endovascular surgery may be
performed. It is easy and comfortable to perform simultaneous
hybrid surgery in this environment. The hybrid approach has several
advantages (8). Firstly, there is
no delay in providing complete revascularization to the ischemic
limb. Secondly, the length of stay in hospital is reduced and
finally, puncture-site complications are eliminated since the
target artery is accessed through the surgical field and the access
site becomes the location of proximal anastomosis. In the present
study, all endovascular procedures were performed through the
surgically exposed artery and there were no puncture-site
complications in the hybrid group.
When performing a combined femoral endarterectomy
and iliac angioplasty/stenting, the procedure sequence may be
crucial. Previously, Dosluoglu et al (9) recommended pre-arteriotomy guidewire
access, where the distal external iliac artery (EIA), CFA, SFA and
deep femoral artery are exposed. The puncture site is selected by
manually palpating the CFA and EIA. If the CFA is not amenable to
puncture due to occlusion or heavy calcification, the distal EIA is
punctured. The same technique was employed in the current study. In
the conventional percutaneous approach, it may be dangerous to
puncture the EIA due to the high risk of retroperitoneal bleeding.
However, it is avoided in hybrid surgery since the puncture site
may be repaired using an open surgical technique.
In the present study, one patient underwent combined
distal origin bypass graft and iliac artery stenting. Distal origin
bypass grafts have been shown to have a relatively high limb
salvage rate with reasonable morbidity and mortality rates
(10,11). The technique of simultaneous SFA
endovascular intervention and popliteal to distal bypass was first
reviewed by Schneider et al (12). In this previous study, 12 patients
were treated with SFA angioplasty and distal bypass graft
originating from the popliteal artery. There were no perioperative
graft failures or amputations and the 2-year primary patency rate
was 76%. In the current study, simultaneous common iliac artery
(CIA) endovascular intervention and popliteal to distal bypass was
performed. This approach may be ideal for this type of combined
lesion.
Cotroneo et al reported 2-year results of
hybrid revascularization (13).
The technical success rate was 100% whilst the primary patency rate
was 86.2% at 6 months and 79.1% at 24 months. Dosluoglu et
al stratified hybrid surgery as simple (sHYBRID group) when the
endovascular-treated segment was TASC classification A/B and
complex (cHYBRID group), when it was C/D (14). The immediate technical success rate
was 96% for cHYBRID and 100% for sHYBRID procedures. At the mean
follow-up of 30.3 months, the 12- and 36-month primary patency
rates in patients who had aortoiliac level interventions in the
sHYBRID were 80 and 75%, respectively, and were similar to those in
the cHYBRID group, which were 87 and 81%, respectively (P=0.863).
Limb salvage rates at 12 and 36 months in patients with critical
limb ischemia were similar in the endovascular, sHYBRID and open
groups (86 and 80; 94 and 80; and 80 and 74%, respectively);
however, these rates were improved in the cHYBRID group (100%;
P=0.014). In the present study, the initial technical success rate
of hybrid surgery was 90.5%. At the mean follow-up of 10.4 months,
the primary patency rates of hybrid and open surgery were 100 and
90.9%, respectively. Hybrid surgery has a theoretical advantage
compared with open or endovascular revascularization performed
separately, in terms of patency rate. With hybrid surgery, inflow
or outflow arteries may be revascularized, which may affect the
patency rate. However, as the follow-up period was only 10 months
in the current study, a longer-term follow-up is required to
confirm this hypothesis.
The annual number of hybrid procedures is
increasing. Aho and Venermo (15)
reported that this number ranged between 4 in 2004 and 73 in 2011.
Of these hybrid procedures, the proportion of endovascular
surgeries performed by vascular surgeons increased from 0% in 2004
to 86.3% in 2011. Relatively young vascular surgeons have adopted
endovascular surgery and become familiar with it. According to a
survey conducted by the Society for Vascular Surgery (16), younger vascular surgeons (those
aged <50 years) more frequently reported >50% of their
workload being endovascular, compared with older vascular surgeons
(aged ≥50 years) (P<0.001). The endovascular skills of vascular
surgeons have improved through education and simulator-based
endovascular skills training (17–20).
Performing hybrid surgery may greatly reduce
hospital charges and the length of stay (LOS). Ebaugh et al
evaluated the costs of staged versus simultaneous lower extremity
arterial hybrid procedures (21).
Notably, the unadjusted results showed that hospital charges and
LOS more than doubled if staged rather than simultaneous hybrid
procedures were performed.
Limitations of the present study include its
retrospective nature, and the small number of patients from a
single center. The groups were heterogeneous and were not directly
comparable. In addition, the follow-up period was too short to
fully evaluate the patency rate following hybrid
revascularization.
In conclusion, hybrid procedures are a feasible
option for multilevel peripheral arterial occlusive disease, with
favorable patency and limb salvage rates. The observations of the
current study indicate that femoral endarterectomy plays an
important role in hybrid surgery.
Acknowledgements
This work was supported by a grant from Kyung Hee
University (KHU-20100752).
References
|
1
|
Norgren L, Hiatt WR, Dormandy JA, et al:
Inter-society consensus for the management of peripheral arterial
disease (TASC II). J Vasc Surg. 45(Suppl S): S5–S67. 2007.
View Article : Google Scholar
|
|
2
|
Wilson SE, White GH, Wolf G and Cross AP:
Proximal percutaneous balloon angioplasty and distal bypass for
multilevel arterial occlusion. Veterans administration cooperative
study no 199. Ann Vasc Surg. 4:351–355. 1990. View Article : Google Scholar
|
|
3
|
Brewster DC, Cambria RP, Darling RC, et
al: Long-term results of combined iliac balloon angioplasty and
distal surgical revascularization. Ann Surg. 210:324–331. 1989.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Queral LA, Criado FJ and Patten P:
Retrograde iliofemoral endarterectomy facilitated by balloon
angioplasty. J Vasc Surg. 22:742–748. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nelson PR, Powell RJ, Schermerhorn ML, et
al: Early results of external iliac artery stenting combined with
common femoral artery endarterectomy. J Vasc Surg. 35:1107–1113.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Timaran CH, Prault TL, Stevens SL, et al:
Iliac artery stenting versus surgical reconstruction for TASC
(TransAtlantic Inter-Society Consensus) type B and type C iliac
lesions. J Vasc Surg. 38:272–278. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Schanzer A, Owens CD, Conte MS and Belkin
M: Superficial femoral artery percutaneous intervention is an
effective strategy to optimize inflow for distal origin bypass
grafts. J Vasc Surg. 45:740–743. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Schneider PA: Iliac angioplasty and
stenting in association with infrainguinal bypasses: timing and
techniques. Semin Vasc Surg. 16:291–299. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Dosluoglu HH and Cherr GS: Pre-arteriotomy
guidewire access (PAGA): a crucial maneuver for securing inflow
and/or outflow in patients with bulky iliofemoral occlusive disease
undergoing combined (open/endovascular) procedures. Eur J Vasc
Endovasc Surg. 32:97–100. 2006. View Article : Google Scholar
|
|
10
|
Galaria II, Surowiec SM, Tanski WJ, et al:
Popliteal-to-distal bypass: identifying risk factors associated
with limb loss and graft failure. Vasc Endovasc Surg. 39:393–400.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Grego F, Antonello M, Stramana R, et al:
Popliteal-to-distal bypass for limb salvage. Ann Vasc Surg.
18:321–328. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Schneider PA, Caps MT, Ogawa DY and Hayman
ES: Intraoperative superficial femoral artery balloon angioplasty
and popliteal to distal bypass graft: an option for combined open
and endovascular treatment of diabetic gangrene. J Vasc Surg.
33:955–962. 2001. View Article : Google Scholar
|
|
13
|
Cotroneo AR, Iezzi R, Marano G, et al:
Hybrid therapy in patients with complex peripheral multifocal
steno-obstructive vascular disease: two-year results. Cardiovasc
Intervent Radiol. 30:355–361. 2007.PubMed/NCBI
|
|
14
|
Dosluoglu HH, Lall P, Cherr GS, et al:
Role of simple and complex hybrid revascularization procedures for
symptomatic lower extremity occlusive disease. J Vasc Surg.
51:1425–1435. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Aho PS and Venermo M: Hybrid procedures as
a novel technique in the treatment of critical limb ischemia. Scand
J Surg. 101:107–113. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Matthews MA, Satiani B and Lohr JM: Trends
in a changing vascular practice environment for members of the
Society for Vascular Surgery. J Vasc Surg. 57:586–592. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tedesco MM, Pak JJ, Harris EJ Jr, et al:
Simulation-based endovascular skills assessment: the future of
credentialing? J Vasc Surg. 47:1008–1014. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lee JT, Qiu M, Teshome M, et al: The
utility of endovascular simulation to improve technical performance
and stimulate continued interest of preclinical medical students in
vascular surgery. J Surg Educ. 66:367–373. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Aparajita R, Zayed MA, Casey K, et al:
Development and implementation of an introductory endovascular
training course for medical students. Ann Vasc Surg. 25:1104–1112.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Markovic J, Peyser C, Cavoores T, et al:
Impact of endovascular simulator training on vascular surgery as a
career choice in medical students. J Vasc Surg. 55:1515–1521. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ebaugh JL, Gagnon D, Owens CD, et al:
Comparison of costs of staged versus simultaneous lower extremity
arterial hybrid procedures. Am J Surg. 196:634–640. 2008.
View Article : Google Scholar : PubMed/NCBI
|