Introduction
Schwannomas are solitary, encapsulated,
slow-growing, benign tumors arising from Schwann cells of the
peripheral nervous system (1).
Between 25 and 45% of all schwannomas occur in the head and neck
region and are usually located in the parapharyngeal space.
Schwannomas of the larynx are extremely rare, accounting for
0.1–1.5% of all benign laryngeal tumors (2). The current report presents a case of
laryngeal schwannoma located in the aryepiglottic fold.
Case report
A 29-year-old female consulted the Department of
Otolaryngology, Head and Neck Surgery, Shanghai Jiao Tong
University Affiliated Shanghai First People’s Hospital (Shanghai,
China) with symptoms of hoarseness and dyspnea on exertion that had
been present for 3 years. The patient had also experienced
dysphagia for 1 month, which had recently worsened. In a previous
hospital, 2 months prior to consultation, the tumor had been
biopsied and the pathodiagnosis revealed a schwannoma. No other
significant past medical illnesses were present and systemic
examination was normal. No palpable lymph nodes or café au lait
patches were present. Informed consent was obtained from the
patient.
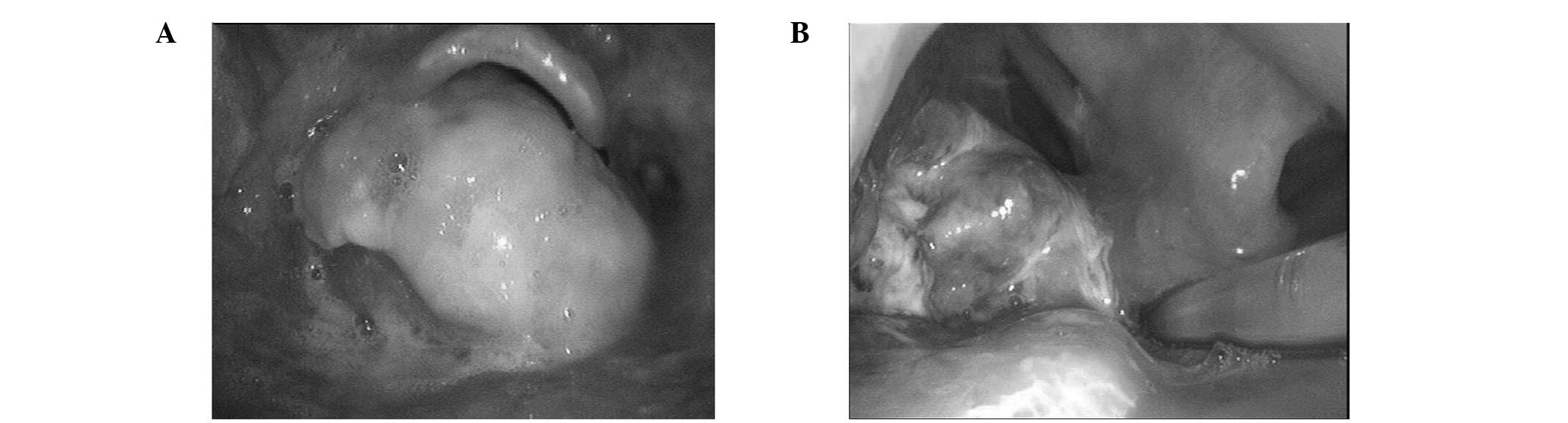
Outpatient laryngoscopy revealed a large mass
located within the left recessus piriformis. In addition, the
glottis was obstructed and the vocal folds were not visible
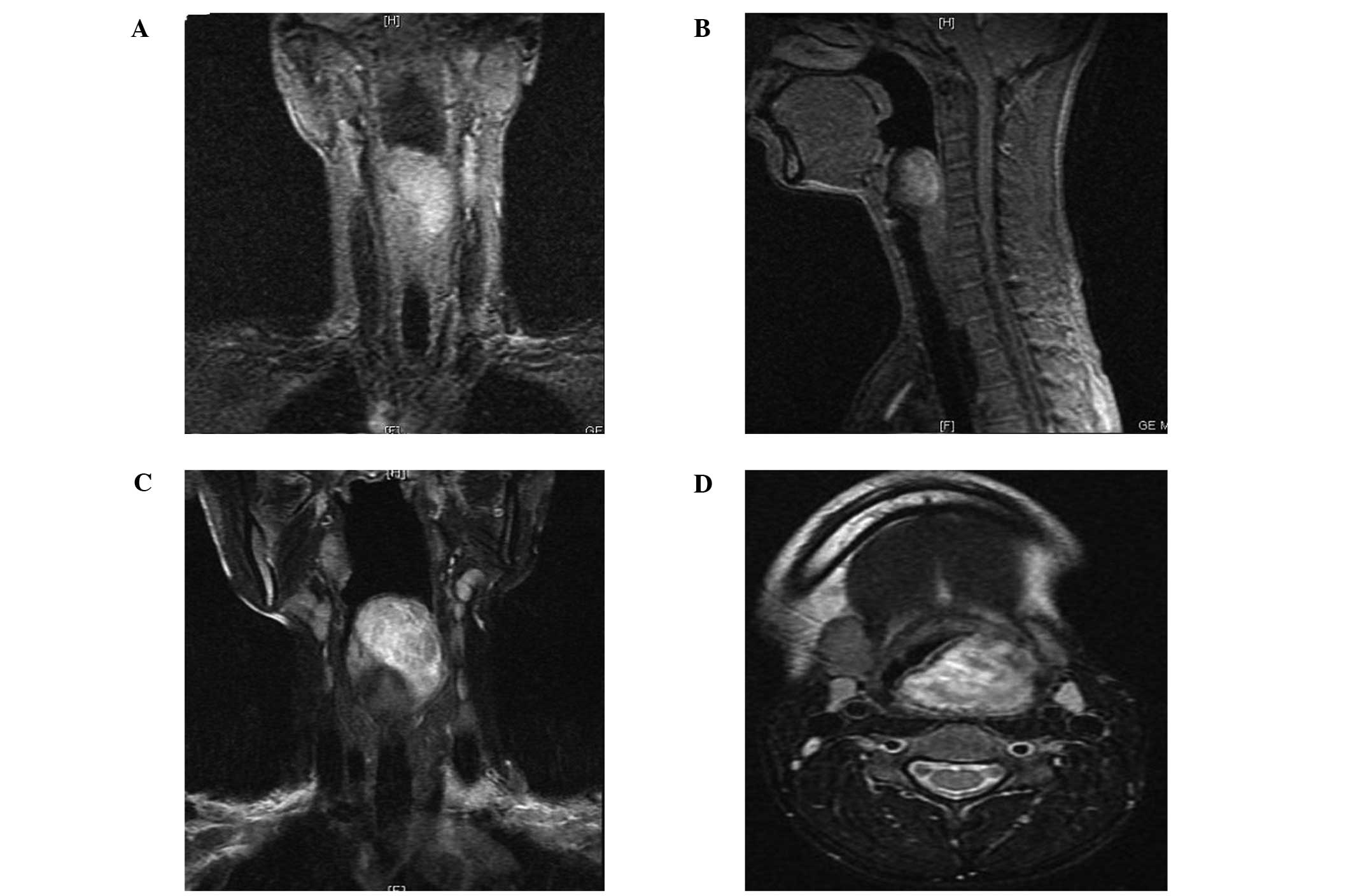
(Fig. 1A). Magnetic resonance
imaging (MRI) of the lesion revealed it to be isodense compared
with muscle in the T1-weighted images that exhibited strong,
inhomogeneous enhancement by gadolinium. In the T2-weighted images,
the lesion was shown to be hyperintense and inhomogeneous. The
lesion was a well-defined, enhanced, inverted conical mass,
measuring 58×29×26 mm in size and centered on the posterior and
lateral wall of the left recessus piriformis. The lesion appeared
to originate from the left aryepiglottic fold. The left recessus
piriformis and vocal cords were effaced (Fig. 2).
Following consideration of age and symptoms, the
patient selected not to undergo surgery via an incision in the
lateral neck. Therefore, a trans-oral resection using a
microlaryngoscope was performed and postoperative tracheostomy was
avoided. Treatment for the symptoms and nutritional support was
administered, including anti-inflammatory agents, hemostatic
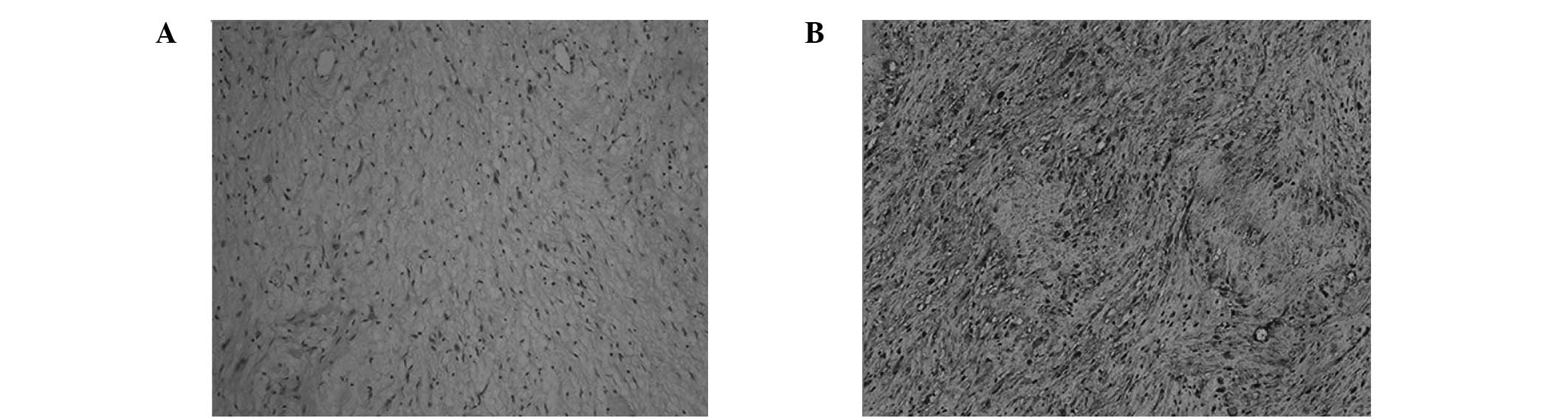
methods and nasogastric nutrition. Microscopic examination showed
compact cellular margins and prominent palisade formation, known as
Antoni A patterns. A less cellular, loosely-textured pattern, known
as the Antoni B pattern, was also observed. Immunochemical staining
evaluation demonstrated the expression of S-100, resulting in a
final diagnosis of a benign schwannoma (Fig. 3).
The patient was discharged on the fifth
postoperative day and the nasal feeding tube was removed.
Postoperative laryngoscopy showed that the left vocal cord was
immobile and that the remaining tumor was present within the left
recessus piriformis (Fig. 1B). It
is unlikely that the immobility of the left vocal fold was the
result of injury. The nerve may have caused the immobility. Close
follow-up of the patient was advised.
Discussion
Schwannomas and neurofibromas are two types of
neurogenic tumor. Neurofibroma is the main differential diagnosis
of laryngeal schwannoma. Other differential diagnoses include
chondroma, adenoma, laryngeal cyst and laryngocele (3). Schwannomas account for 0.1–1.5% of
all benign laryngeal tumors. Schwannomas are encapsulated, benign,
solitary tumors that grow slowly and were first reported by Verocay
in 1908 (4,5). Schwannomas deriving from perineural
Schwann cells grow extrinsically to their parent nerve fascicles
and may develop along any somatic or sympathetic nerve in the body
(with the exception of the olfactory and optic nerves due to the
lack of Schwann cell sheaths) (6).
By contrast, neurofibromas originate from perineural fibrocytes,
involving nerve fibers and sheath cells. These tumors exhibit
diffuse proliferation and are usually intertwined with the nerve
trunk (2).
Schwannomas most commonly occur in females between
the ages of their 4th and 5th decades. In total, 80% of laryngeal
schwannomas are found in the aryepiglottic folds, while the
remaining 20% are found in the false and true cords (7). In the majority of cases, the nerve of
origin is likely to be the internal branch of the superior
laryngeal nerve (8).
Clinical symptoms are related to the size and
location of the tumor (1). The
patient may complain of a number of symptoms, including dysphagia,
dyspnea, dysphonia, hoarseness and a foreign body sensation in the
throat (3). However, these
clinical features are meaningless to the definite diagnosis
(1).
Laryngoscopic evaluation reveals a round submucosal
mass originating from the aryepiglottic fold and/or true and/or
false vocal cords.
With CT scans, a small schwannoma is regarded as a
homogenous, enhanced mass (9).
When the size is large (>3 cm), tumors are often heterogeneous,
with randomly distributed areas of low attenuation, surrounded by a
peripheral ring of enhancement. Generally, cystic components may be
observed (10).
When examined by MRI, T1-weighted images of
schwannomas have a low signal intensity ranging between those of
the brain and muscles, with a homogeneous or heterogeneous
appearance (11). With T2-weighted
images, the schwannomas have a brighter signal than cerebrospinal
fluid and may be heterogeneous or homogeneous (11). The images are usually well-enhanced
following gadolinium injection (9).
Although CT and MRI scans reveal a well-defined
submucosal mass without surrounding tissue destruction (12), the methods are not able to
differentiate a schwannoma from other laryngeal neoplasms (13). Histopathological examination is the
gold standard. The diagnosis of schwannoma may be made with the
presence of three features: i) a clear capsule; ii) the presence of
Antoni A and/or B areas; and iii) a positive reaction for S-100
protein (14). Antoni A regions
are described by densely packed spindle cells with nuclei aligned
in parallel rows in a palisade pattern. Antoni B regions consist of
loosely arranged spindle cells, with vacuoles and spindle-shaped
nuclei prone to degeneration (2).
Laryngeal schwannoma is a rare benign tumor and the
curative method is surgical resection (13). However, this method may not be
suitable for every patient due to anatomical constraints and the
requests of patients (15). There
are a number of surgical methods that may be used, including
trans-oral microlaryngoscopic excision, median thyrotomy and
lateral pharyngotomy. Generally, the treatment of laryngeal
schwannomas depends on the location and size of the tumor (16). Trans-oral microlaryngoscopic
excision is suitable for small lesions and successful resections
have been reported (3). In 2011,
Kayhan et al (12)
demonstrated the first case of transoral robotic surgery-assisted
excision of a schwannoma in the supraglottic larynx. An open
approach may be wise for larger lesions (13). The complete excision of the tumor
is desirable, and recurrence is very rare, even if a portion of the
capsule is left behind (4). For
these reasons, the method of trans-oral microlaryngoscopic excision
was used for the patient in the current case. Since schwannomas are
slow-growing, we are able to excise the tumor under a
microlaryngoscope without tracheotomy to maintain the patient’s
quality of life.
References
|
1
|
Xu J, Zheng Y, Li G and Su X: A rare
finding of multiple schwannomas in the epiglottis. Otolaryngol Head
Neck Surg. 147:1160–1161. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zbären P and Markwalder R: Schwannoma of
the true vocal cord. Otolaryngol Head Neck Surg. 121:837–839.
1999.
|
|
3
|
Ebmeyer J, Reineke U, Gehl HB, et al:
Schwannoma of the larynx. Head Neck Oncol. 1:242009. View Article : Google Scholar
|
|
4
|
Vijayendra H, Nanjundappa and Sangeetha R:
Laryngeal schwannomas-case reports with rare presentations. Indian
J Otolaryngol Head Neck Surg. 60:185–187. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Verocay J: Multiple Geschwülste als
Systemerkrankung am nervösen. Festschrift F. Chiari Wien and
Leipzig: W. Braunmiller; pp. 378–415. 1908
|
|
6
|
Rognone E, Rossi A, Conte M, et al:
Laryngeal schwannoma in an 8-year-old boy with inspiratory dyspnea.
Head Neck. 29:972–975. 2007.PubMed/NCBI
|
|
7
|
Fini-Storchi I and Frosini P: Laryngeal
neurinoma. A case report and review. ORL J Otorhinolaryngol Relat
Spec. 59:182–185. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Phang WK, Raman R and Jayalaksmi E:
Neurogenous tumour of the larynx (a case report). J Laryngol Otol.
101:1209–1210. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Plantet MM, Hagay C, De Maulmont C, et al:
Laryngeal schwannomas. Eur J Radiol. 21:61–66. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yamamoto S, Masuda S, Okazaki T, Izumi H
and Dambara T: A case report of neurinoma originating from the
recurrent nerve. Nihon Kyobu Geka Gakkai Zasshi. 39:2203–2207.
1991.(In Japanese).
|
|
11
|
Friedman DP, Tartaglino LM and Flanders
AE: Intradural schwannomas of the spine: MR findings with emphasis
on contrast-enhancement characteristics. AJR Am J Roentgenol.
158:1347–1350. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kayhan FT, Kaya KH and Yilmazbayhan ED:
Transoral robotic approach for schwannoma of the larynx. J
Craniofac Surg. 22:1000–1002. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lo S and Ho WK: Schwannoma of the larynx -
an uncommon cause of vocal cord immobility. Hong Kong Med J.
10:131–133. 2004.PubMed/NCBI
|
|
14
|
Rosen FS, Pou AM and Quinn FB Jr:
Obstructive supraglottic schwannoma: a case report and review of
the literature. Laryngoscope. 112:997–1002. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Meriç F, Arslan A, Cüreoğlu S and
Nazaroğlu H: Schwannoma of the larynx: case report. Eur Arch
Otorhinolaryngol. 257:555–557. 2000.
|
|
16
|
Vital I, Fliss DM and Cohen JT: Laryngeal
schwannoma excised under direct laryngoscopy: case report. Ear Nose
Throat J. 91:204–205. 2012.PubMed/NCBI
|