Introduction
In recent years, with increasing public health
knowledge, liability issues and awareness of self-protection,
medical healthcare providers have faced increasing risks.
Delivering safe nursing and identifying and reducing risks have
become the main tasks for nursing staff. Neuroma studies have been
carried out on nursing risks and risk management (1–3),
resulting in a number of risk analysis and management systems,
particularly for important clinical departments and major common
diseases (4–6). These include analyses of the types of
risks and their causes and management. For diabetes, a number of
risk assessment methods are available, including nutritional risk
screening, which was designed to identify diabetic patients through
assessment of their nutritional condition (7–9).
However, little has been reported on an integrated nutritional and
nursing risk assessment from the patient’s and the nursing staff’s
prospective. The present study was conducted to establish and
evaluate a risk assessment method for diabetic inpatients in order
to enable nursing staff and patients to predict risk factors for
nutritional intervention.
Subjects and methods
Subjects
The data of 2,065 participants were selected from
the type II diabetic inpatients in the Departments of Elderly
Endocrinology and Endocrinology at the Provincial People’s hospital
between January 2009 and December 2012, together with data for
their nursing attendants. Subjects with incomplete data were
excluded. The participants consisted of 1,276 males and 786
females, aged between 60 and 98 years old, with an average age of
68±11.32 years old. The participants were grouped randomly into two
groups, A and B, consisting of 1,043 and 1,033 participants,
respectively. The two groups had comparable profiles, including age
and gender. This study was approved by the Sichuan Academy of
Medical Sciences Review Board (Institutional Review Board no.
B4589888).
Questionnaire for risk assessment
The risk assessment questionnaire was designed to
have two parts, one was designed to review the nursing risk for
nursing staff and the other was designed to evaluate the risk for
nutritional intervention. Part one was used to assess the nursing
staff for their knowledge about the disease, physical exercise, the
functions and side-effects of antidiabetic drugs, and the recording
and monitoring of patient’s weight, blood sugar level and diet. The
rationality of the staff’s guidance for balanced patient food
intake and their knowledge of a non-indicative label for
hypoglycemic drugs were also assessed.
The second part was to assess the patient’s personal
and nutritional risk factors, including gender, age, height,
weight, administration of antidiabetic drugs, daily intake of
staple food, intake of vegetables and fruits, diet composition
(such as high fat and low fiber), dining time (fixed or not),
dining habit (whether the patient dined out more than three times
per week) and exercise (whether the patient was sitting down whilst
working, without much movement, and whether the patient exercised
for 3–4 h per week). Other information that was collected in this
section of the questionnaire included any family history of
diabetes (namely, if the patient’s parents or siblings were
diabetic), smoking and drinking histories, a history of high blood
sugar level (whether or not the patient had previously been
diabetic or was a latent diabetic) and a history of any
hypertension, hyperlipidemia and coronary heart disease.
Methods
Prior to conducting this investigation, consent was
obtained from the clinicians, with whom the projects were
discussed, and who provided support. In total, 15 trained nutrition
nurses, six with excellent accuracy in completing questionnaires,
were selected to participate in this investigation. All
participants were asked to sign their informed consent and complete
the questionnaire under the supervision of the trained nurses.
Blood sugar level change was used as a dependent
variable; if it changed, it was assigned a value of 1, and
otherwise a value of 0. All other factors were treated as
independent variables, including age and gender. These variables
were used in an unconditional multivariate logistic regression
analysis to screen for risk factors. A factor (Xi) with P<0.05
was considered to be significant. In the logistic regression
analysis, regression coefficient β indicates the relative degree of
risk increase from increments of the independent variable.
Therefore, values that were 10 times that of the β value were used
to calculate the risk score of the respective variables. An
individual’s predicted nursing risk was, therefore, determined by
the number and score of the risks that they possessed.
The risks and their scores that were determined
using the data from group A were used to evaluate group B in order
to validate the method. The accumulated score [∑(Xi × Score)] of
individuals in group B was calculated. The cutoff value for a
high-risk patient was determined and the diagnostic accuracy of the
method was tested by Youden’s index (10). The 2006 World Health Organization
diagnostic criteria of diabetes was used to measure the level of
blood sugar (11). The blood sugar
levels were considered changed if there was either a ≥7.0 mmol/l
difference in fasting plasma glucose or an 11.1 mmol/l difference
in post-challenge 2-h plasma glucose.
Statistical analysis
Unconditional multivariate logistic regression
analysis was used to analyze the correlation between the variables
and blood sugar level change. Percentage values were tested for any
differences using the χ2 test. The area under the
receiver operating characteristic (ROC) curve (AUC) was used to
calculate the risk of developing diabetes. The data were processed
using SPSS software (version 16.0; SPSS, Inc., Chicago, IL, USA),
and the statistical significance was indicated by P<0.05.
Results
Identification of risk factors
To identify the risk factors, data from group A were
analyzed using unconditional multivariate logistic regression
analysis, with blood sugar level change used as a dependent
variable.
Among the 20 variables analyzed, eight were found to
be significantly associated with the blood sugar level change
(P<0.05; Table I), including
age, body mass index, waist to hip ratio, diet and histories of
smoking, alcohol consumption, diabetes and high blood pressure. The
coefficient β of the variables was multiplied 10 times and used as
the risk score (Table I).
 | Table ILogistic regression analysis of risk
factors. |
Table I
Logistic regression analysis of risk
factors.
| Variable | β | OR | 95% CI | P-value |
|---|
| Age | 1.826 | 6.379 | 2.911–14.480 | <0.05 |
| BMI | 1.858 | 7.394 | 3.384–16.190 | <0.05 |
| WHR | 1.011 | 2.844 | 1.295–4.468 | <0.05 |
| Diet | 2.004 | 2.931 | 1.499–4.321 | <0.05 |
| Smoking history | 2.938 | 3.542 | 1.639–5.707 | <0.05 |
| Alcohol
consumption | 2.036 | 2.212 | 1.162–3.933 | <0.05 |
| History of family
diabetes | 1.868 | 5.740 | 3.814–8.933 | <0.05 |
| History of high blood
pressure | 2.048 | 15.616 | 8.991–29.340 | <0.05 |
Risk scores of nutritional and nursing
variables
To evaluate the level of risk, the accumulated
scores of the identified significant variables, as well as the
blood sugar level change over the accumulated scores were
calculated for individual patients (Table II). As shown in Table II, the change in the blood sugar
level increased with the accumulated scores, with a significant
association between them (P<0.001). Therefore, the score can be
used to differentiate between patients with different levels of
risk. Such differentiation would aid further screening of high-risk
patients and the implementation of proper preventive measures.
 | Table IINutritional and nursing risks for
diabetic patients measured by the accumulated scores. |
Table II
Nutritional and nursing risks for
diabetic patients measured by the accumulated scores.
| Accumulated
score | No. of patients | No. of patients with
blood sugar changea | Patients with blood
sugar change, % | OR |
|---|
| 0–25 | 173 | 1 | 0.58 | 1.00 |
| 26–50 | 484 | 11 | 2.27 | 4.18 |
| 51–75 | 317 | 29 | 9.15 | 15.70 |
| 76–100 | 43 | 15 | 34.88 | 92.28 |
| 101–125 | 5 | 4 | 80.00 | 738.94 |
Evolution of the nutritional and nursing
risk assessment
The patients in group B were evaluated at different
accumulated scores, used as cutoff values, and the results are
shown in Table II. It was found
that Youden’s index was at the maximum when the score was 50.
Therefore, the score was used as the cutoff value. At this point,
the sensitivity and specificity were 88.3 and 66.5%, respectively.
This means that if 34% of the high-risk inpatients are screened,
3/5 of the nursing risks can be identified by this method in the
same inpatient population, which has predictive positive and
negative rates of 12.83 and 98.52%, respectively.
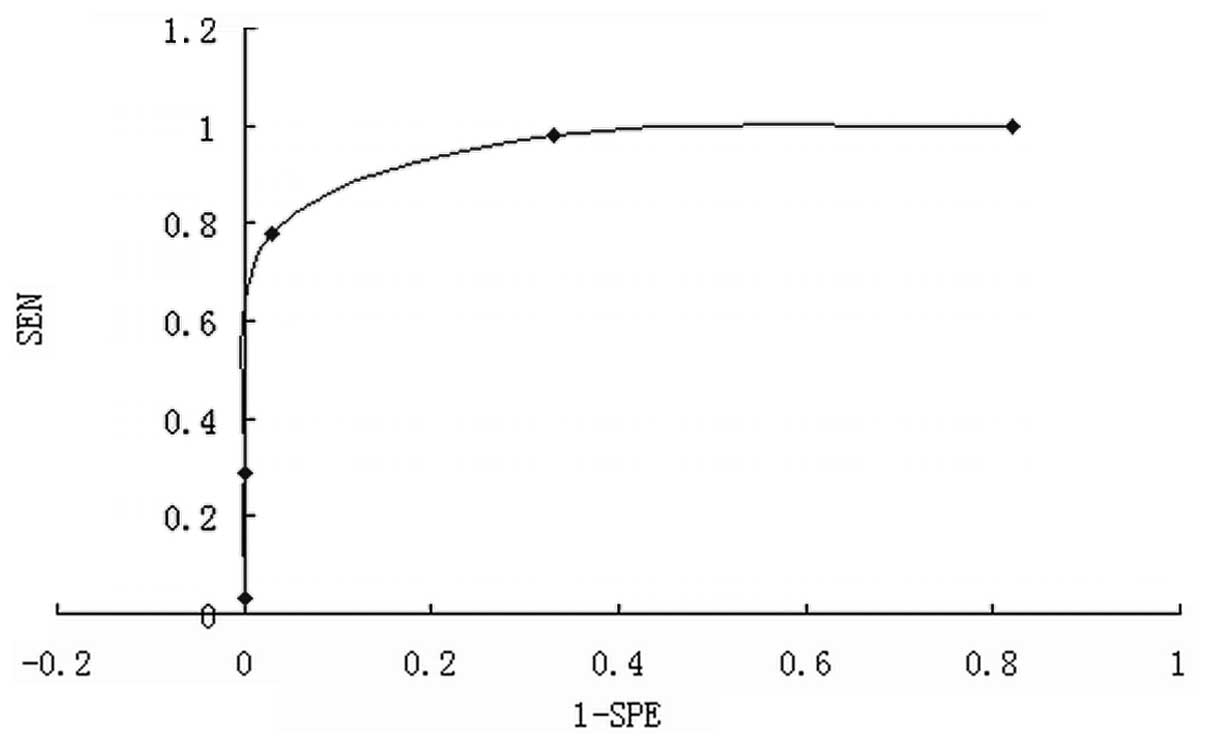
The reliability of the method was further confirmed
by ROC curve analysis, where the AUC was 0.82, with a standard
error of 0.018 and a 95% confidence interval value of 0.783–0.856
(Fig. 1), indicating that the risk
assessment method is able to reliably identify the risks in
diabetic patient care.
Discussion
Diabetes is a common metabolic endocrine disease,
often accompanied by systemic chronic complications in multiple
organs and systems. Diabetes has high morbidity and mortality
rates, resulting in a physically and economically heavy burden on
patients. According to the 2007–2008 statistics, the overall
prevalence of diabetes has reached 9.7% in China (11,12).
There is an urgent requirement to perform a risk assessment for the
large number of patients with diabetes in order to improve their
care and treatment. If such assessments can be made from a nursing
prospective to identify the nutritional risk at an early stage, it
would aid in providing improved nutrition-based therapy and early
warning signs for healthcare activities.
A number of risk predictive methods are available to
determine whether there are nutritional risks for diabetic
patients, and what the clinical outcomes for the patients with
these risks would be (13–15). These methods have been used as
preliminary tools to screen for individuals with a high risk of
diabetes, and are therefore useful in assisting and identifying the
risk of diabetes in patients at an early stage. The method
described in the present study is an integrated screen that may be
used by nursing staff and patients to assess nutrition and
nursing-related risks. This would consequently result in nursing
staff having an improved understanding of the patient’s nutritional
care requirements, in order to provide superior educational and
healthcare service to patients and to prevent or delay disease
progression, with fewer complications.
Results from this study demonstrated that
nutritional and nursing risk assessment screening can effectively
reduce the nursing risk and should be part of the integrated risk
management system in hospitals. This method can be used by nursing
staff and patients. Risk assessment screening is a simple, fast and
highly sensitive method, with a high detection rate for positively
diagnosed patients and a low implementation cost and false positive
(or high specificity) rate.
Acknowledgements
The present study was supported by a research fund
from the Sichuan Provincial Health Department (project number,
090441) and a research fund from Sichuan Provincial Science and
Technology Department (project number, 2009SZ0249).
References
|
1
|
Kuzu MA, Terzioğlu H, Genç V, et al:
Preoperative nutritional risk assessment in predicting
postoperative outcome in patients undergoing major surgery. World J
Surg. 30:378–390. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Vellas B, Guigoz Y, Garry PJ, et al: The
Mini Nutritional Assessment (MNA) and its use in grading the
nutritional state of elderly patients. Nutrition. 15:116–122. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Peng LT, Li R, Zhao WH, et al: Nutritional
risk screening and its clinical significance in 706 children
hospitalized in the surgical department. Zhongguo Dang Dai Er Ke Za
Zhi. 15:880–885. 2013.(In Chinese).
|
|
4
|
Schiesser M, Müller S, Kirchhoff P,
Breitenstein S, Schäfer M and Clavien PA: Assessment of a novel
screening score for nutritional risk in predicting complications in
gastro-intestinal surgery. Clin Nutr. 27:565–570. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Schiesser M, Kirchhoff P, Müller MK,
Schäfer M and Clavien PA: The correlation of nutrition risk index,
nutrition risk score, and bioimpedance analysis with postoperative
complications in patients undergoing gastrointestinal surgery.
Surgery. 145:519–526. 2009. View Article : Google Scholar
|
|
6
|
Kondrup J, Allison SP, Elia M, et al:
Educational and Clinical Practice Committee, European Society of
Parenteral and Enteral Nutrition (ESPEN): ESPEN guidelines for
nutrition screening 2002. Clin Nutr. 22:415–421. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kondrup J, Rasmussen HH, Hamberg O and
Stanga Z; Ad Hoc ESPEN Working Group. Nutritional risk screening
(NRS 2002): a new method based on an analysis of controlled
clinical trials. Clin Nutr. 22:321–336. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kiyici S, Ersoy C, Kaderli A, et al:
Effect of rosiglitazone, metformin and medical nutrition treatment
on arterial stiffness, serum MMP-9 and MCP-1 levels in drug naive
type 2 diabetic patients. Diabetes Res Clin Pract. 86:44–50. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jing XF, Qiao R, Li M, Kang DY, Liu XH and
Huang CY: Developing a risk appraisal model for gestational
diabetes mellitus. Sichuan Da Xue Xue Bao Yi Xue Ban. 42:353–357.
2011.(In Chinese).
|
|
10
|
Youden WJ: Index for rating diagnostic
tests. Cancer. 3:32–35. 1950. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang H, Song Z, Ba Y, Zhu L and Wen Y:
Nutritional and eating education improves knowledge and practice of
patients with type 2 diabetes concerning dietary intake and blood
glucose control in an outlying city of China. Public Health Nutr.
1–8. 2013.PubMed/NCBI
|
|
12
|
Yang YN, Xie X, Ma YT, et al: Type 2
diabetes in Xinjiang Uygur autonomous region, China. PLoS One.
7:e352702012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Danquah I, Bedu-Addo G, Terpe KJ, et al:
Diabetes mellitus type 2 in urban Ghana: characteristics and
associated factors. BMC Public Health. 12:2102012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chung SH, Han DC, Noh H, et al: Risk
factors for mortality in diabetic peritoneal dialysis patients.
Nephrol Dial Transplant. 25:3742–3748. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Debussche X, Roddier M, Fianu A, et al:
REDIA Study Group: Health perceptions of diabetic patients in the
REDIA study. Diabetes Metab. 32:50–55. 2006. View Article : Google Scholar : PubMed/NCBI
|