Introduction
Double aortic arch (DAA) is the most common form of
vascular ring and accounts for 33–73% of vascular ring
malformations (1). DAA entirely or
partially surrounds the trachea and esophagus and causes
compression and symptoms, including wheezing and difficulties in
respiration and swallowing. However, unclear clinical features lead
to misdiagnosis or even fatal aorta-tracheal fistula due to
tracheal cannula (2). Therefore,
early accurate diagnosis is critical (3). In the present study, data from 15
patients who were surgically diagnosed with DAA were summarized and
compared with the patients’ multi-slice spiral computed tomography
(MSCT) results. DAA classification and MSCT characteristic
performance were also analyzed to assess the diagnostic value of
MSCT and increase its accuracy in DAA diagnosis.
Subjects and methods
Clinical data
A total of 15 cases (nine males and six females;
aged between seven days and 66 years old, with an average age of
2.5 years) diagnosed with DAA malformation through computed
tomography (CT) and confirmed by surgery were recruited from the
Wuhan Asia Heart Hospital (Wuhan, China) between May 2005 and March
2013. All patients underwent a chest X-ray and echocardiography
concurrently. The pediatric patients exhibited different levels of
wheezing, coughing, and shortness of breath or failure of the
respiratory system, and nine of them had feeding difficulties. This
study was conducted in accordance with the Declaration of Helsinki
and with approval from the Ethics Committee of Wuhan Asia Heart
Hospital. Written informed consent was obtained from the subjects
or their legal guardians.
Scanning method
A Brilliance CT 64-channel scanner (Koninklijke
Philips N.V., Amsterdam, Holland) or Somatom Definition Flash
dual-source CT scanner (Siemens AG, Forchheim, Germany) was
utilized for the scanning. Patients incapable of coordination
fasted for 4–6 h and were then anesthetized (polyphenols: 2.0–2.5
mg/kg) and scanned. Patients capable of respiratory coordination
were asked to hold their breath for 15–20 sec after inspiration
during the scanning. Electrocardiogram (ECG)-gating and oxygen
inhalation were employed, and ECG and saturation of blood oxygen
were detected during the scanning. A non-ionic contrast agent
(Ultravist; 370 mgI/ml; Bayer Schering Pharma AG, Berlin, Germany)
and a dual syringe injector (Medrad Stellant CT Injector system;
Medrad, Pittsburgh, PA, USA) were used, and the injection duration
was 15–22 sec. The injection dose and flow speed of the Ultravist
were as follows: If ≤12 years old, 2.0–2.5 ml/kg and 2.0–2.5
ml/sec; and if >12 years old, 60–80 ml and 3.0–3.8 ml/sec;
followed with 4–15 ml saline injection at 0.8–3.0 ml/sec. If ≤12
years old, delayed scanning was employed after the injections, with
a delay time of 15–19 sec; and if >12 years old, bolus tracking
and its automatic triggering were employed to monitor the
enhancement of the descending aorta, and the view of interest was
set in the descending aorta on the aortopulmonary window level,
with a threshold value of 100–140 HU. The scanning scope ranged
from the upper edge of the sixth cervical vertebra to 1 cm below
the lower edge of the apex. The Brilliance CT 64-channel scanning
parameters were as follows: 80–120 kV, 100–300 mAsec, pitch of
0.2–0.3, X-ray tube rotation time of 0.4 sec/round, 180×180 to
300×300 mm field of view (FOV), matrix size of 512×512, slice
thickness of 0.67 mm, reconstruction interval of 0.33 mm,
reconstruction phase 40% and 75%. The Somatom Definition Flash
dual-source CT scanning parameters were as follows: 80–120 kV,
100–300mAsec, pitch of 0.2–0.5, X-ray tube rotation time of 0.33
sec/round, 180×180 to 300×300 mm FOV, matrix size of 512×512, slice
thickness of 0.75 mm, reconstruction interval of 0.40 mm, and the
reconstruction phase was automatically determined by a computer to
select the best systolic and diastolic periods. Following the
scanning, the original data were uploaded to the Philips Extended
Brilliance Workspace (Koninklijke Philips N.V.).
Medical care of patients
All subjects were asked to wear lead eyeglasses,
scarves and aprons below the abdomen to reduce the radiation damage
to the thyroid, gonads and eyes.
Results of the diagnosis and imaging
diagnostic methods
All diagnoses were provided by at least two experts
in cardiovascular imaging following the independent analysis of the
CT imaging results and clinical features according to the principle
of DAA pathological anatomy. The tracheal stenosis and its location
were also assessed. Agreements were obtained and in-depth
discussions were held when disagreements occurred. The post
analysis included multi-planar reconstruction (MPR), maximum
intensity projection (MIP), minimum intensity projection (MinIP)
and volume rendering (VR).
Results
Comparison of MSCT with ECG and surgical
observations
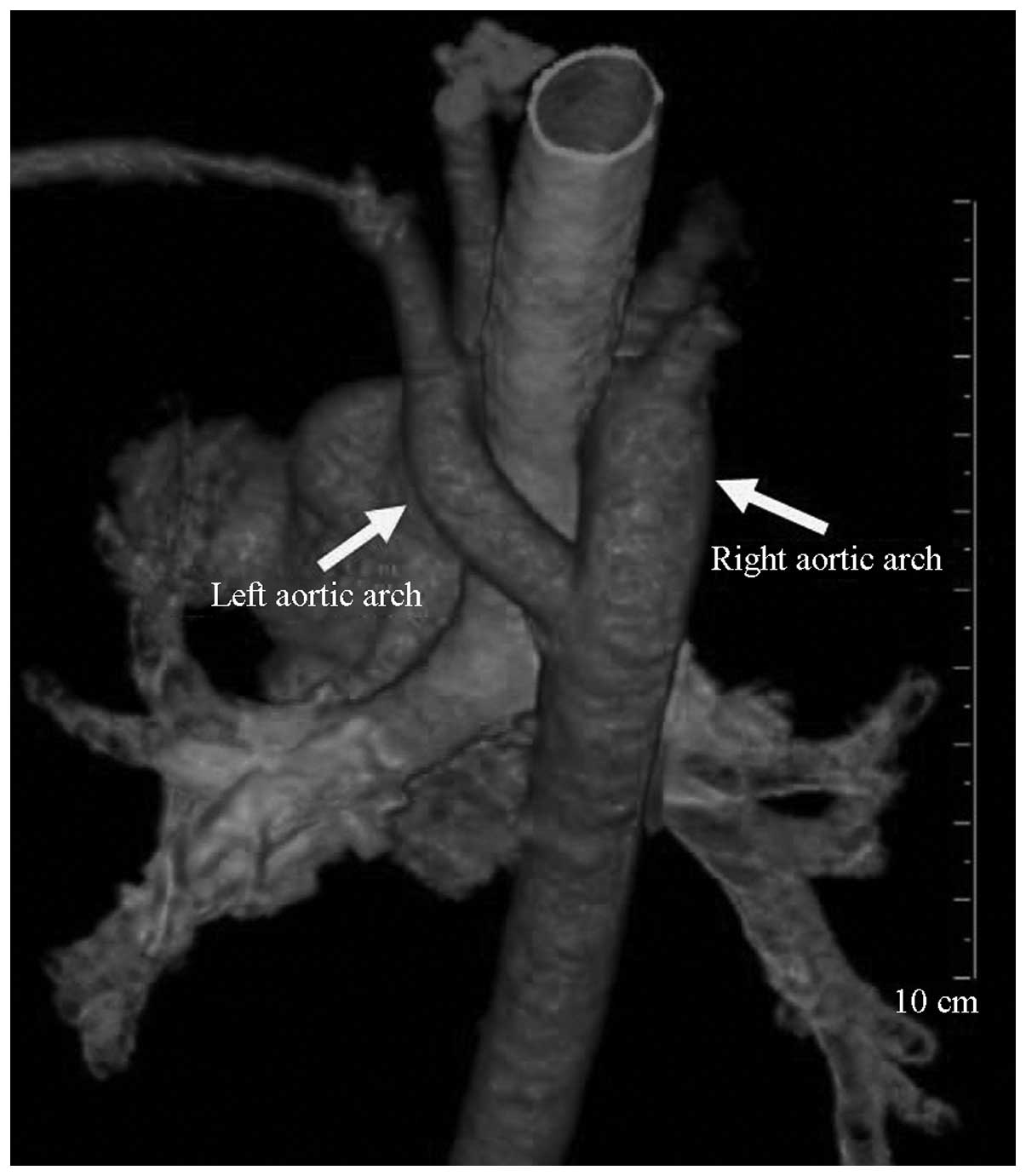
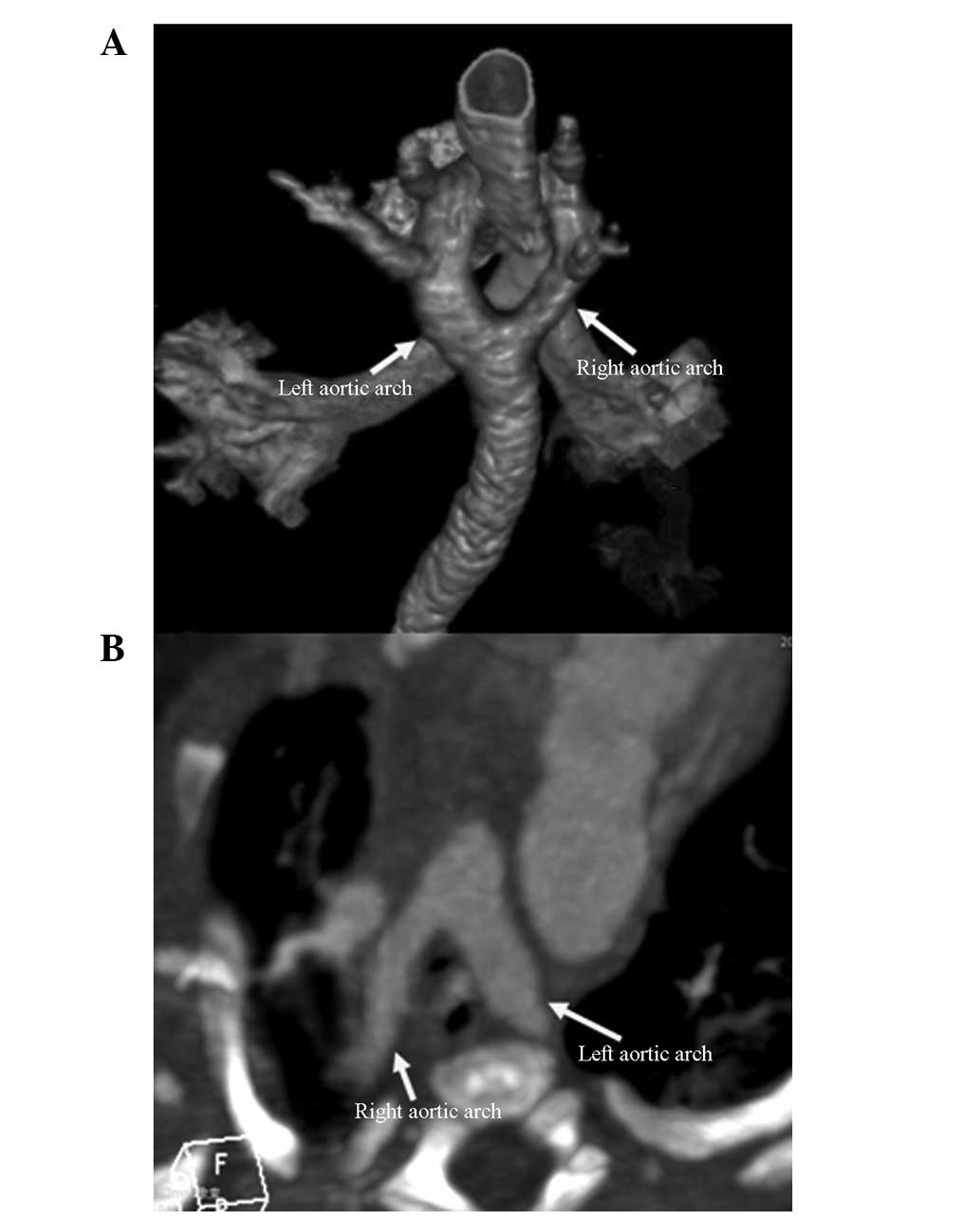
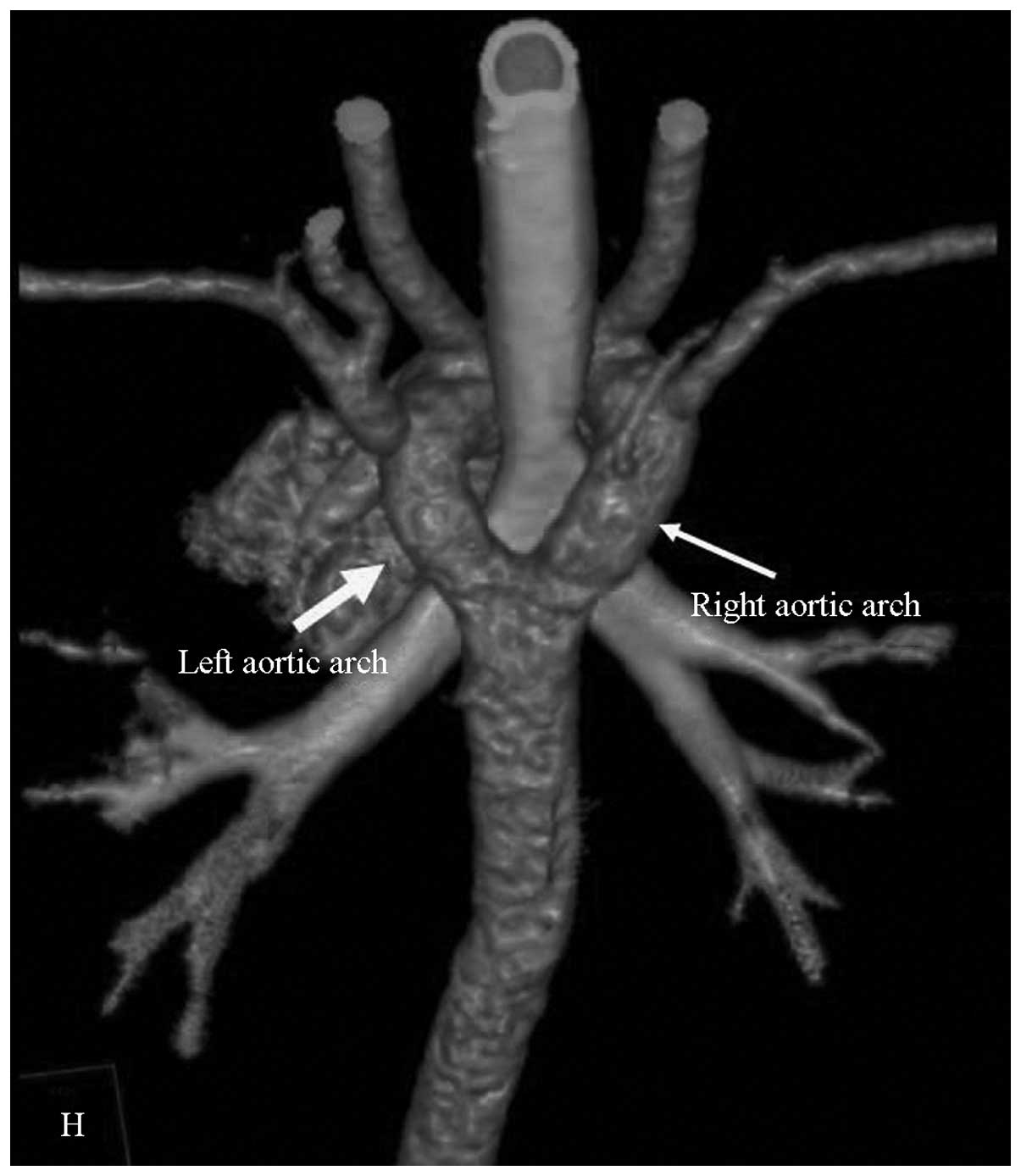
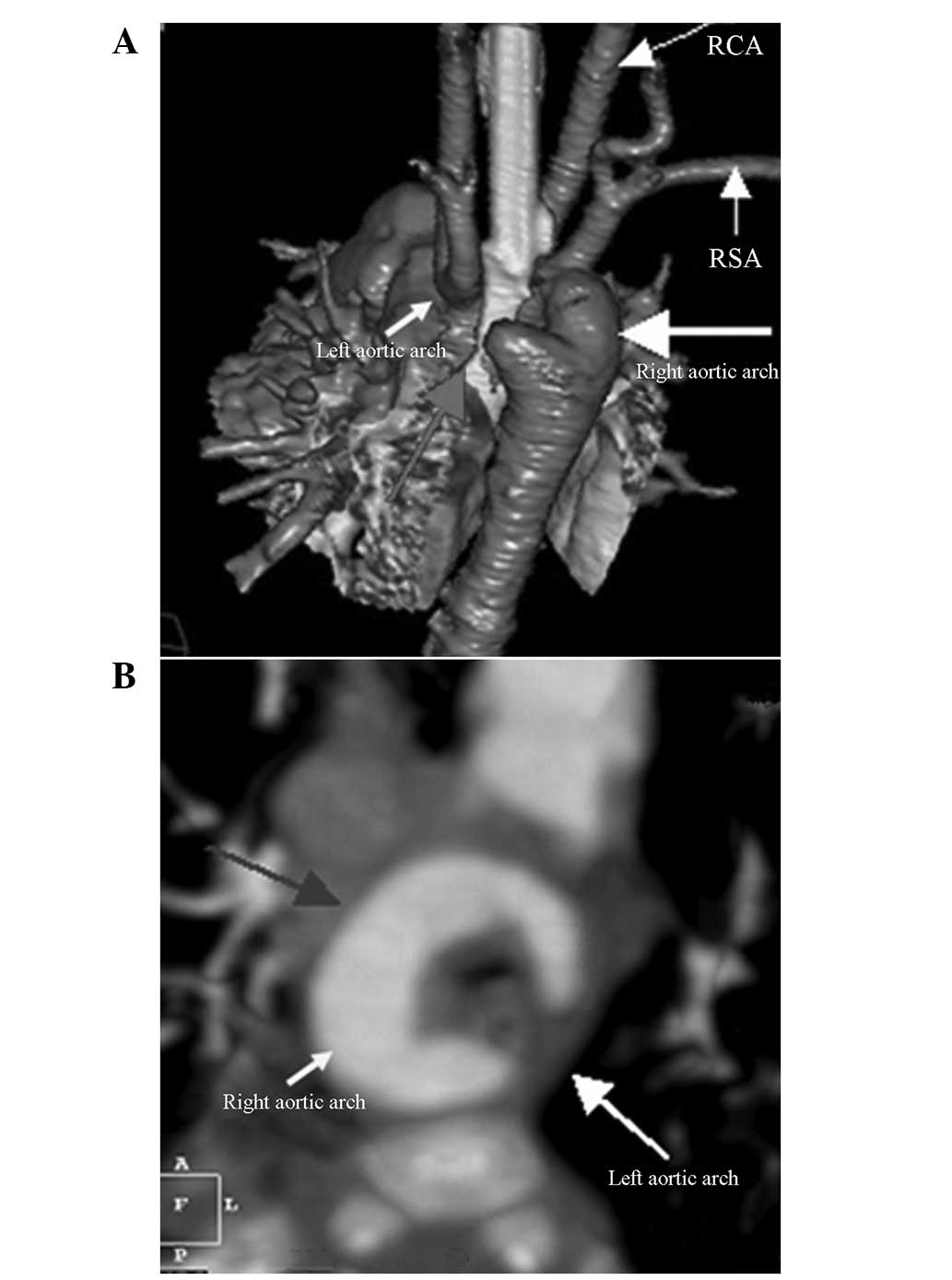
All 15 patients with DDA were precisely diagnosed
using MSCT and they were as follows: 13 cases of type I (double
arches are open), including nine with a larger right arch (Fig. 1), two with a larger left arch
(Fig. 2), and two with balanced
arches (Fig. 3); and two cases of
type II (one atretic arch), which were both cases of left atretic
arch (Fig. 4). The ultrasound
diagnosis succeeded in nine cases and failed in six. In these six
cases, five were diagnosed with right aortic arch, of which three
were diagnosed with DAA with a larger right arch and smaller left
arch. Two of the three cases had DAA with left atretic arch; one
was pre-diagnosed with left aortic arch by ultrasound, which was
actually DAA with a larger left arch and a smaller right arch.
Among the 15 patients with DAA, only two were identified to have a
single malformation, whereas the remainder had single or multiple
combination(s) of intracardiac and extracardiac malformations.
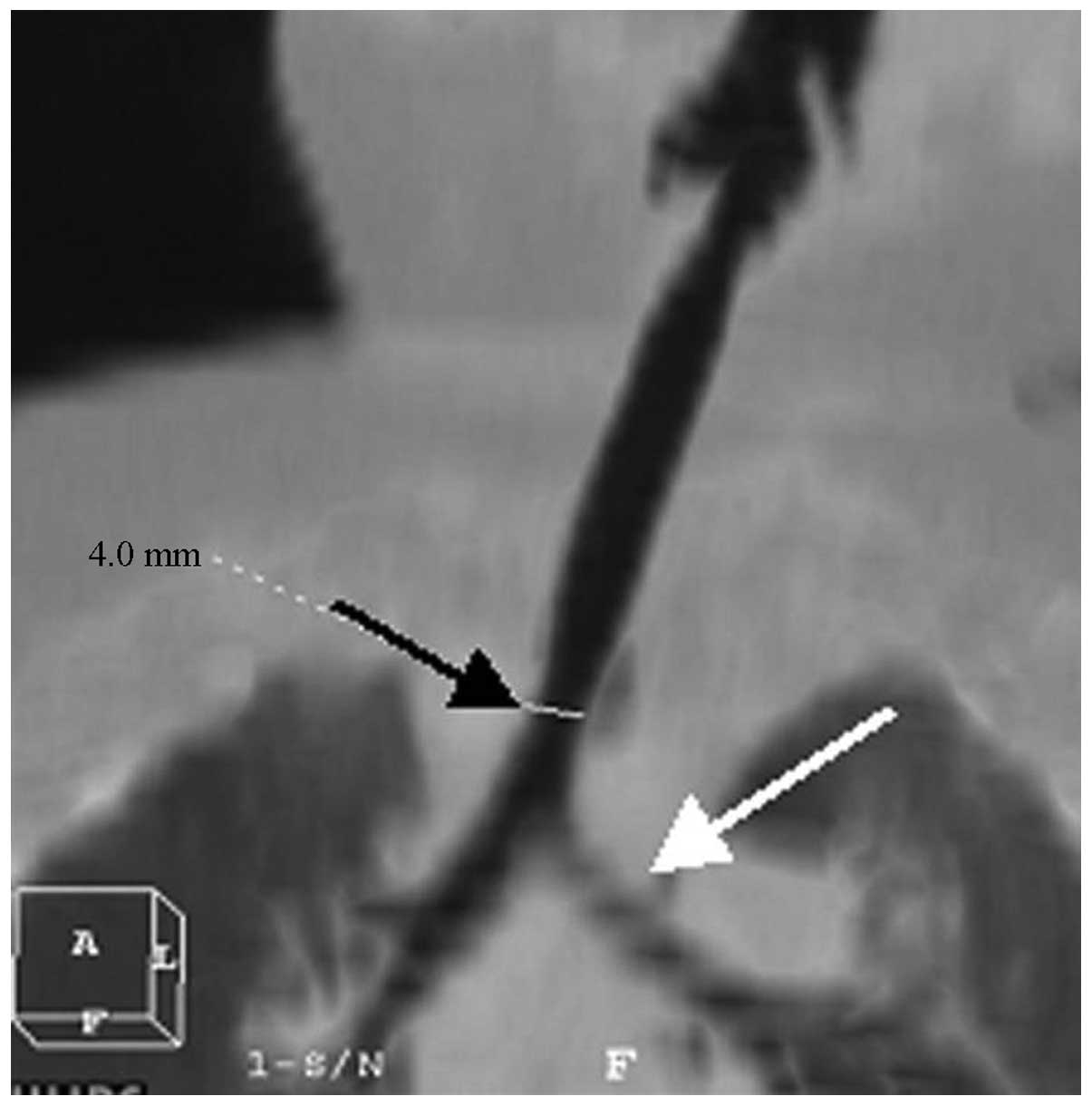
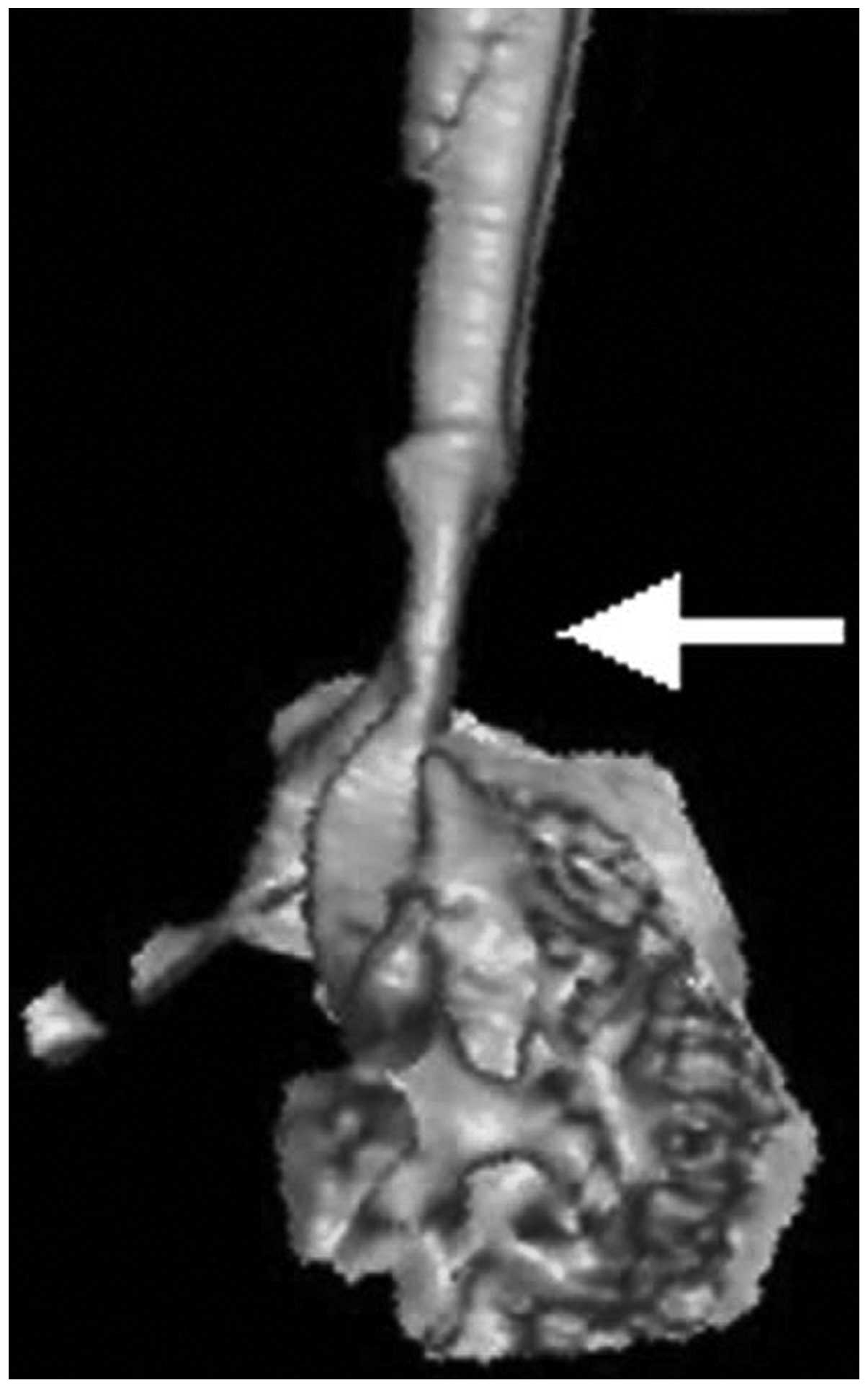
Complication of tracheal stenosis and
morphological abnormalities
Seven patients exhibited complications caused by
different levels of tracheobronchial stenosis. The MPR, VR and MIP
analyses revealed the stenosis of the lower trachea or the bronchus
that was involved due to compression (Figs. 5 and 6).
Discussion
MSCT examination of the DAA anomalies was conducted
to clarify the classification and degrees of the combined trachea
and bronchial stenosis, as well as the type of the combined endo-
and extra-cardiac malformations, which are of clinical significance
to the clinicians who select the treatment options. There are few
applications of MSCT in cardiovascular disease diagnosis due to the
limitations of early CT devices. Therefore, published studies
relating to the MSCT diagnosis of DAA anomalies have mainly been
case report studies, e.g., that by Choi et al (4). With the development of chest imaging
tomographic technology, congenital abnormal blood vessel-induced
tracheal stenosis is easily and accurately diagnosed and surgically
treated, although the risks associated with sedation remain
relatively high (5,6). Previous CT equipment prior to
64-slice spiral CT scanners, including single-slice, four-slice and
even 16-slice spiral CT, generally takes 10–20 sec to obtain chest
images of an infant or toddler. The image motion artifacts are
heavy as infants are not able to independently hold their breath.
The 64-slice spiral and dual-source CT scanners have a high time
resolution rate; and combined with the ECG-gating technique, chest
and cardiovascular scanning achieves high-quality images and even
avoids motion artifacts. In the present study, the diagnostic
accuracy rate of aortic double arch anomalies and types, and
tracheal stenosis reached 100%.
DAA is involved in embryonic aortic arch
abnormality; the fourth pairs of the bilateral aortic arch and
dorsal aortic root fail in degradation and absorption. DAA is
pathologically characterized by the normal position of the
ascending aorta that bifurcates into the left and right aortic
arches in front of the trachea. Pathological classification is into
the following two types: i) The two aortic arches are open,
generally with a larger right arch and a smaller left arch
(7) and ii) one arch is atretic,
which has been reported to account for 42–60% of cases and is
usually on the left side (8–10).
Two of the 15 cases in the present study had DAA with left atretic
arch, which is a markedly different frequency compared with that
indicated in the literature and is possibly due to the limited
number of subjects in the present study. Statistically, DAA is
frequently complicated by intracardiac and extracardiac
malformations, including tetralogy of Fallot, complete
transposition of the great arteries, atrial septal defect,
ventricular septal defect and patent ductus arteriosus (11). Among all the cases with aortic arch
anomalies in the present study, only one was observed without
cardiac malformations. DAA is regarded as the most common type of
vascular ring that causes difficulty in respiration due to trachea
compression according to a previous study (12). In the present study, seven patients
suffered from different degrees of tracheobronchial stenosis.
MSCT is a non-invasive method characterized by a
short scanning time, rapid imaging, high time and spatial
resolution, and higher isotropic of Z-axis direction. The powerful
post-processing function of MSCT allows for the observation of
lesions from different angles. MSCT not only clearly reveals the
shape and direction of an abnormal vascular ring but also
accurately identifies the situation of the tracheal and esophageal
compression, which is essential in the diagnosis of pediatric
cardiovascular and respiratory diseases (13,14).
The MSCT angiography and 3D reconstruction techniques used in the
diagnosis of DAA include MIP, VR and MinIP. Axial CT imaging is the
basis for DAA diagnosis. The MSCT characteristics of DAA are the
visible ‘()’-like vascular structure on the two sides of the
trachea in the CT image of the aortic arch in the axial dimension,
the narrowing of the trachea, and the enclosed esophagus. If one
arch is closed, ‘(’ or ‘)’ are observed in the axial dimension of
the aortic arch, and a visible ligament-like structure on the side
of the closed aortic arch; similar trachea compression is also
observed. It is possible to set the MIP image to an appropriate
thickness and orientation to display different pathological changes
in the same window. The image is also used to observe cardiac
malformations, including atrial and ventricular septal defects, and
measure the diameter of the aortic arch. VR is a 3D image that can
be rotated at any angle, and intuitively and stereoscopically
displays the entire vascular ring and its branches and origin, and
the development of the pulmonary arteries, as well as the 3D
association between the vascular ring and tracheal compression. VR
transparency technology and MinIP show the structural relationship
of air-rich trachea, bronchus and lungs with good contrast and
sharpness and clearly display anatomical structures with high
accuracy and minor human factors (1,15,16).
Angiocardiography is a conventional method that is
considered the gold standard in diagnosing DAA due to its high
selectivity and excellent capability to indicate anatomy and blood
flow in the main pulmonary artery and its branches. However,
angiocardiography is invasive, difficult for patients (particularly
pediatric patients) to tolerate, and unable to show the compression
of the esophagus and trachea as a 2D image. Plain chest radiography
and the barium swallow test have been used as auxiliary methods in
DAA diagnosis; the two methods reveal indirect signs, including
compression of the trachea and esophagus by the aorta and the
pulmonary artery and its branches (17). Echocardiography is a non-invasive
and simple examination method that identifies the section
morphology of the aorta and pulmonary artery and their blood flow
in real time. The technique facilitates the diagnosis of
complicated intracardiac malformations. However, the disadvantages
of echocardiography include the following: i) The display of
branches is affected by numerous factors, including the chest bone,
pulmonary air, and the technique of the examiner; and ii) poor 3D
imaging, which fails to show the vascular spatial orientation and
compression of the trachea and esophagus, particularly in patients
suffering from double arch deformity with one arch atresia that
cannot be accurately diagnosed by echocardiography (18,19).
MRI angiography is an effective diagnostic method that does not
involve radiation but produces worse image reconstruction, density
and time resolution than those of MSCT (20,21).
In addition, MRI angiography is not feasible for children who do
not cooperate and critically ill patients due to the long duration
of MRI scanning (22). The main
disadvantage of MSCT angiography is radiation, which is solved by
wearing lead eyeglasses, scarves and aprons to minimize the
exposure of patients without influencing the diagnosis (23).
In summary, patients with DAA commonly suffer from
complications caused by intracardiac and extracardiac malformations
and different degrees of airway stenosis, whereas DAA with one-side
arch atresia mostly involves left arch atresia. MSCT precisely
diagnoses DAA complicated by anomalies and airway stenosis. MSCT is
important in treating DAA and thus serves as the primary tool for
DAA diagnosis.
Acknowledgements
This study was supported by the Natural Science
Foundation of Hubei Province (no. 2012FFB04422).
References
|
1
|
Juraszek AL and Guleserian KJ: Common
aortic arch anomalies: diagnosis and management. Curr Treat Options
Cardiovasc Med. 8:414–418. 2006. View Article : Google Scholar
|
|
2
|
Miura T, Nakamura J, Yamada S, et al: A
fatal aortoesophageal fistula caused by critical combination of
double aortic arch and nasogastric tube insertion for superior
mesenteric artery syndrome. Case Rep Gastroenterol. 4:198–203.
2010. View Article : Google Scholar
|
|
3
|
Shanmugam G, Macarthur K and Pollock J:
Surgical repair of double aortic arch: 16-year experience. Asian
Cardiovasc Thorac Ann. 13:4–10. 2005.PubMed/NCBI
|
|
4
|
Choi HS, Shin DH, Kim KR and Park YA:
Preoperative three-dimensional CT angiography to distinguish
between an aberrant subclavian artery and a double aortic arch in
thyroid surgery: Report of 2 cases. Auris Nasus Larynx. 38:127–132.
2011. View Article : Google Scholar
|
|
5
|
Pacharn P, Poe SA and Donnelly LF:
Low-tube-current multidetector CT for children with suspected
extrinsic airway compression. AJR Am J Roentgenol. 179:1523–1527.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Berdon WE: Rings, slings, and other
things: vascular compression of the infant trachea updated from the
midcentury to the millennium - the legacy of Robert E. Gross, MD,
and Edward B. D. Neuhauser, MD. Radiology. 216:624–632. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Danzi GB, Salice P and Mosca F: Double
aortic arch in neonates: optimal definition by means of
contrast-enhanced helical CT scan. Heart. 97:9502011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Subramanyan R, Venugopalan P and Narayan
R: Vascular rings: an important cause of persistent respiratory
symptoms in infants and children. Indian Pediatr. 40:951–957.
2003.PubMed/NCBI
|
|
9
|
Narayan RL, Kanwar A, Jacobi A and Sanz J:
Imaging a boa constrictor - the incomplete double aortic arch
syndrome. Heart Lung Circ. 21:745–746. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Schlesinger AE, Krishnamurthy R, Sena LM,
et al: Incomplete double aortic arch with atresia of the distal
left arch: distinctive imaging appearance. AJR Am J Roentgenol.
184:1634–1639. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Alsenaidi K, Gurofsky R, Karamlou T, et
al: Management and outcomes of double aortic arch in 81 patients.
Pediatrics. 118:e1336–1341. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Singh C, Gupta M and Sharma S: Compression
of trachea due to double aortic arch: demonstration by multi-slice
CT scan (MSCT). Heart Lung Circ. 15:332–333. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Katz M, Konen E, Rozenman J, et al: Spiral
CT and 3D image reconstruction of vascular rings and associated
tracheobronchial anomalies. J Comput Assist Tomogr. 19:564–568.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gustafson LM, Liu JH, Link DT, Strife JL
and Cotton RT: Spiral CT versus MRI in neonatal airway evaluation.
Int J Pediatr Otorhinolaryngol. 52:197–201. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Honnef D, Wildberger JE, Das M, et al:
Value of virtual tracheobronchoscopy and bronchography from
16-slice multidetector-row spiral computed tomography for
assessment of suspected tracheobronchial stenosis in children. Eur
Radiol. 16:1684–1691. 2006. View Article : Google Scholar
|
|
16
|
Lee EY, Zurakowski D, Waltz DA, et al:
MDCT evaluation of the prevalence of tracheomalacia in children
with mediastinal aortic vascular anomalies. J Thorac Imaging.
23:258–265. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Alboliras ET, Lombardo S and Antillon J:
Truncus arteriosus with double aortic arch: two-dimensional and
color flow Doppler echocardiographic diagnosis. Am Heart J.
129:415–417. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Turan S, Turan OM, Maisel P, Gaskin P,
Harman CR and Baschat AA: Three-dimensional sonography in the
prenatal diagnosis of aortic arch abnormalities. J Clin Ultrasound.
37:253–257. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sivaprakasam MC and Vettukattil JJ: 3-D
echocardiographic imaging of double aortic arch. Eur J
Echocardiogr. 7:476–477. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Russo V, Renzulli M, La Palombara C and
Fattori R: Congenital diseases of the thoracic aorta. Role of MRI
and MRA. Eur Radiol. 16:676–684. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Cantinotti M, Hegde S, Bell A and Razavi
R: Diagnostic role of magnetic resonance imaging in identifying
aortic arch anomalies. Congenit Heart Dis. 3:117–123. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kilner PJ: Imaging congenital heart
disease in adults. Br J Radiol. 84:S258–S268. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Chen X, Qu YJ, Peng ZY, Lu JG and Ma XJ:
Diagnosis of congenital aortic arch anomalies in Chinese children
by multi-detector computed tomography angiography. J Huazhong Univ
Sci Technolog Med Sci. 33:447–451. 2013. View Article : Google Scholar : PubMed/NCBI
|