Introduction
Currently, conventional chemotherapy is one of the
main approaches for the treatment of numerous forms of advanced
cancer. Increasing the dose intensity (DI) of chemotherapeutic
drugs is considered to enhance their ability to kill cancer cells
and reduce the occurrence of drug resistance. However, increasing
the DI is not feasible due to the resultant chemotherapy-induced
myelosuppression (1,2). At present, strategies for the
management of chemotherapy-induced myelosuppression are limited.
Furthermore, the therapeutic effects vary significantly among
individuals, and a number of adverse reactions have been observed.
Therefore, an improved therapeutic method is urgently required to
solve this problem.
In 1988, Dr Eliane Gluckman successfully treated a
child with Fanconi anemia by performing the first umbilical cord
blood (UCB) hematopoietic stem cell (HSC) transplantation, which
demonstrated that UCB-HSC transplantation may be a promising tool
for the treatment of blood system impairments (3,4).
Traditional allogeneic UCB-HSC transplantation requires partial
human leukocyte antigen (HLA) matching, ablation of the recipient’s
marrow and immunosuppression following transplantation (5,6).
These requirements significantly limit the broad application of
UCB-HSC transplantation in patients with chemotherapy-related
myelosuppression. However, a number of studies have shown that
non-HLA matched allogeneic UCB-HSC transplantation exerts no risk
of graft-versus-host disease (GVHD), and encouraging clinical
therapeutic effects have been observed in the treatment of
degenerative diseases (6–8). The underlying mechanism of the cord
blood stem cells is hypothesized to be largely a result of the
secretion of a number of growth factors, which are considered to be
central in the repair of injured cells. However, transplanted
UCB-HSCs are not permanently engrafted in the recipient’s bone
marrow, as transplanted HSCs are eliminated by the host immune
system after a certain period of time (6). These observations indicate that
non-matched UCB-HSCs may be useful in the treatment of
chemotherapy-related myelosuppression.
In the current study, the clinical observations
following the application of allogeneic UCB-HSC transplantation for
the treatment of chemotherapy-related myelosuppression were
investigated.
Materials and methods
Subjects
In total, 65 patients (male, 42; female, 23; age
range, 22–83 years; average age, 59.32 years) that had been
diagnosed with chemotherapy-related myelosuppression were included
in the study. Written informed consent was obtained from the
patient. These patients had a variety of cancer types, including
lymphoma, lung cancer, gastric cancer, colorectal cancer,
nasopharyngeal carcinoma and breast carcinoma, all of which were
confirmed by a biopsy examination. All the patients received the
conventional dose of chemotherapy (1,2). The
chemotherapy drugs administered were pemetrexed, gemcitabine,
paclitaxel, docetaxel, cisplatin, carboplatin, nedaplatin,
fluorouracil, oxaliplatin, irinotecan, cyclophosphamide, epirubicin
and vindesine. Certain patients also received radiotherapy. The
majority of patients enrolled were classified with stage II
myelosuppression (as defined by National Cancer Institute common
toxicity criteria) prior to the initiation of UCB-HSC infusion
(1,2). A routine blood examination was
conducted for each patient to determine the minimum values of the
white blood cell (WBC) count, hemoglobin (Hb) level and platelet
(PLT) count prior to the stem cell treatment, which were found to
be 0.32×109/l, 69 g/l and 25×109/l,
respectively. Drugs that may have affected the blood cell counts,
including granulocyte colony-stimulating factor (G-CSF),
granulocyte-macrophage colony-stimulating factor (GM-CSF),
erythropoietin (EPO) and thrombopoietin (TPO), were avoided for at
least two weeks prior to and two weeks following UCB-HSC
infusion.
Treatment procedure
UCB was donated by the Obstetrics Department of
Renmin Hospital of Wuhan University (Wuhan, China), and was
harvested in the third stage of labor. HSCs were prepared in the
stem cell laboratory of the Cancer Center of Renmin Hospital. The
study was approved by the Ethics Committee of Renmin Hospital. The
procedures for UCB collection, separation, preservation and testing
were performed according to a previously described protocol
(8,9). UCB-HSCs that were confirmed to be
non-HLA matched and non-ABO matched were stored in 100-ml
suspensions, with an average concentration of 7.07×109/l
and cell viability of >90%. The cells were transfused via a
needle with a diameter of 0.9 mm through the peripheral vein. To
avoid a transfusion reaction and GVHD, 5 mg dexamethasone was
regularly administered via an intravenous drip prior to
transplantation. The vital signs of the patients were closely
monitored during the 30-min period of stem cell infusion.
Evaluation
Karnofsky performance status (KPS) scores were
determined prior to and following UCB-HSC transplantation (10). In addition, routine blood tests
were performed prior to treatment and between days 7 and 14
following treatment. Laboratory parameters, including the WBC and
PLT counts and the Hb level, were recorded and analyzed.
Statistical analysis
SPSS version 12.0 (SPSS, Inc. Chicago, IL, USA) for
Windows was used for statistical analysis, and the data are
expressed as the mean ± standard deviation. A paired t-test was
used to analyze the differences between parameters prior to and
following treatment. In addition, Spearman’s correlation analysis
was performed to analyze correlations among the variables. All the
calculated P-values were two-tailed, and P<0.05 was considered
to indicate a statistically significant difference.
Results
Overall data analysis
As shown in Table
I, the mean WBC count, Hb level and PLT count of the patients
prior to treatment were 4.82±2.41×109/l, 105.75±20.90
g/l and 154.20±94.51×109/l, respectively. Following
UCB-HSC transplantation, these values increased to
5.92±2.51×109/l, 107.02±21.45 g/l and 172.66±105.08 ×
109/l, respectively, with the WBC count increasing by
22.98% (P=0.0001) and the PLT count increasing by 11.97% (P=0.01).
These differences were found to be statistically significant.
 | Table IValues of three blood-related
parameters and KPS scores prior to and following UCB-HSC
transplantation. |
Table I
Values of three blood-related
parameters and KPS scores prior to and following UCB-HSC
transplantation.
| Groups | WBC
(×109/l) | PLT
(×109/l) | Hb (g/l) | KPS |
|---|
| Before treatment |
| Total | 4.82±2.41 | 154.20±94.50 | 105.75±20.90 | 60.00±19.28 |
| Males | 4.85±2.23 | 150.88±96.50 | 109.52±20.00 | 59.28±19.68 |
| Females | 4.75±2.76 | 160.26±92.57 | 98.87±21.16 | 61.30±18.90 |
| KPS ≥60 | 4.49±2.44 | 153.95±73.01 | 109.07±21.78 | 70.89±9.25 |
| KPS <60 | 5.56±2.24 | 154.75±133.19 | 98.30±16.96 | 35.50±11.91 |
| After treatment |
| Total | 5.92±2.51b | 172.66±105.08b | 107.02±21.45 | 67.23±18.83b |
| Males | 6.14±2.45b | 181.62±112.83b | 108.90±22.73 | 65.00±18.38b |
| Females | 5.53±2.62a | 156.30±89.24 | 103.56±18.89 | 71.30±19.38b |
| KPS ≥60 | 5.71±2.54b | 168.29±65.59a | 110.00±20.25 | 77.33±8.89b |
| KPS <60 | 6.42±2.43 | 182.50±164.58 | 100.30±23.06 | 44.5±15.04b |
Subgroup analysis
When analyzed according to gender, the WBC count in
the males (n=42) increased from 4.85±2.23×109/l to
6.14±2.45×109/l (P=0.003), while the PLT count increased
from 150.88±96.50×109/l to
181.62±112.84×109/l (P=0.004). In the female group
(n=23), a statistically significant difference was not observed in
the PLT count following stem cell treatment. However, the WBC count
increased significantly from 4.75±2.76×109/l to
5.53±2.63×109/l (P=0.03), which was a 16.44% increase
(Table I).
Next, the patients were divided into two groups
according to their KPS score (≥60 and <60 points). The WBC and
PLT counts in the group with a KPS score of ≥60 (n=45) increased
from 4.49±2.44×109/l and 153.96±73.01×109/l
to 5.71±2.54×109/l and 168.29±65.59×109/l,
respectively (P=0.0001 and 0.037, respectively). However, in the
patients with a KPS score of <60 (n=20), no statistically
significant differences were observed in the WBC count, PLT count
or Hb level (Table I).
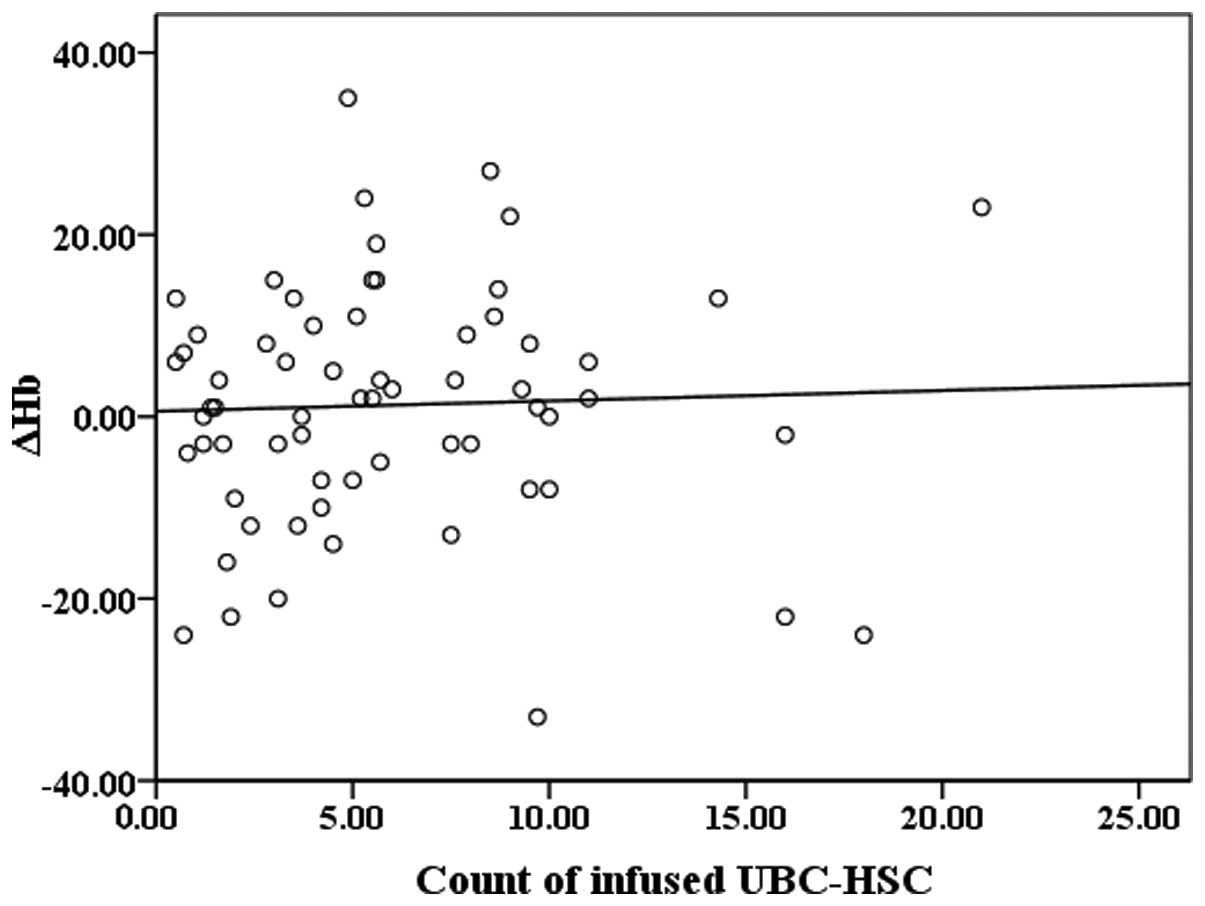
Correlation analysis
To determine whether the actual number of UCB-HSCs
transfused into the patients was associated with the changes in the
WBC count (Fig. 1), PLT count
(Fig. 2) and Hb level (Fig. 3) following treatment, three scatter
plots showing these data were constructed. Notably, the scatter
plots revealed that the three parameters tended to change with the
number of transfused stem cells. Spearman’s correlation analysis
was subsequently conducted and linear correlations were observed
between the number of transfused UCB-HSCs and the ΔWBC (WBC count
following treatment - WBC count prior to treatment; correlation
coefficient, 0.289; P=0.02) or the ΔPLT (PLT count following
treatment - PLT count prior to treatment; correlation coefficient,
0.271; P=0.03).
KPS score
Following UCB-HSC transplantation therapy, the
majority of patients reported noticeable subjective improvements in
numerous symptoms, including fatigue, anorexia, dizziness and chest
congestion. As shown in Table I,
the KPS scores increased significantly following stem cell
treatment (P<0.01).
Adverse reactions
No serious adverse reactions were observed in the
stem cell treatment patients. In addition, there were no
transfusion reactions, evidence of GVHD or cases of morbidity and
mortality attributable to the stem cell transplant procedure.
Discussion
In addition to surgery, chemotherapy is
well-recognized as one of the most important anticancer
interventions. The therapeutic efficacy and overall survival rate
associated with chemotherapy are constantly increasing. However,
chemotherapy-induced myelosuppression limits the possible intensity
and progress of chemotherapy. Although several solutions to the
problem of chemotherapy-induced myelosuppression have emerged in
recent decades, including G-CSF, GM-CSF, interleukin (IL)-11, EPO,
TPO or even blood component infusion (2), these therapies have been found to
have certain disadvantages in clinical practice. For example, these
therapeutic methods are accompanied by numerous adverse reactions,
including edema, headache, fever, palpitation, nausea, vomiting,
dizziness, insomnia, dyspnea, rash, conjunctival congestion and
muscle and joint pain. Furthermore, their therapeutic effects vary
greatly among individuals and the exact efficacy remains unknown
(2,10,11).
Bone marrow is the source of all hematological cells
in the human body, and the majority of blood cells are generated by
HSCs or hematopoietic progenitor cells in the bone marrow. HSCs
have the capacity to self-renew and generate multiple progenitor
cell and mature cell types (12);
thus, in theory, the cells are widely applicable in clinical
practice. Compared with stem cells derived from the bone marrow and
peripheral blood, those derived from the UCB may be a better source
for transplantation due to their various advantages, including
their rich source, strong regeneration ability and weak
antigenicity to cord blood lymphocytes, as well as the low
incidence and severity of GVHD with their use. Furthermore, UCB-HSC
transplantation can be performed even if there are one or two
differences in the HLA between the donor and recipient. Therefore,
this treatment does not require any HLA matching or use of
immunosuppressives (13).
Moreover, the incidence of infection following UCB-HSC
transplantation is low, the response is rapid and the cost is
relatively low. Thus, UCB-HSC transplantation may be a promising
therapy in numerous fields of medicine (13–15).
Previous studies have reported that the use of
UCB-HSCs in the treatment of myelosuppression may activate the bone
marrow (5,7,19).
UCB has been shown to be abundant in hematopoietic growth factors,
including G-CSF (16), GM-CSF
(5), EPO (16), IL-2 (16), IL-6 (16,17),
insulin-like growth factors (18)
and steel factor (7). The
expression levels of these growth factors are significantly higher
in UCB compared with the peripheral blood. Following transfusion,
UCB-HSCs strongly activate stem cells in the bone marrow, thereby
playing an important role in the treatment of myelosuppression
(5,7,19).
Zhang et al (7) summarized
the clinical function of UCB-HSCs as follows: i) Specific
stimulation, where UCB is able to stimulate hematopoiesis in the
host to reverse anemia and granulocytopenia; and ii) non-specific
stimulation, where the subjective symptoms of the patients improve
significantly following UCB transplantation.
UCB is rich in not only hematopoietic growth
factors, but also HSCs, which may be responsible for producing the
majority of the aforementioned growth factors (5). The HSCs in UCB release hematopoietic
growth factors and stimulate hematopoiesis following infusion.
Subsequently, the function of hematopoiesis is gradually restored
in the activated bone marrow. An et al (20) treated 52 patients with
chemotherapy-and radiotherapy-induced myelosuppression using
UCB-HSC transplantation, and found that the WBC and red blood cell
counts in the patients significantly and rapidly improved following
treatment, although the increase in the PLT count was less
significant.
In the present study, the 65 patients exhibited
similar results, with only a few differences. Furthermore, GVHD did
not occur in any patient. Following transplantation, the majority
of the patients achieved a higher KPS score and marked improvements
in a number of clinical symptoms, including fatigue, loss of
appetite, dizziness and chest congestion. At two weeks after
treatment, the blood circulation impairment caused by
myelosuppression recovered, with the WBC and PLT counts increasing
by an average of 22.82 and 11.97%, respectively. However, the
difference in the Hb level prior to and following treatment was not
significant. Additional subgroup analysis based on the gender and
KPS scores revealed that male patients and those with a good KPS
score appeared to benefit more from stem cell transplantation
compared with female patients and those with a poor KPS score,
respectively. In addition, the ΔWBC and ΔPLT in each patient was
found to positively correlate with the number of stem cells
transfused. These observations indicated that increasing the number
of stem cells transfused may promote the restoration of bone marrow
function in patients with myelosuppression. The possibility that
the bone marrows of male patients and patients with a good
performance status showed a better response to growth factors
released by UCB-HSCs was considered. Furthermore, it was
hypothesized that UCB-HSCs stimulate different types of blood cells
via different mechanisms. In future studies, these issues should be
addressed.
In conclusion, the results of the present study
demonstrated that peripheral vein infusion of non-HLA matched
UCB-HSCs markedly improved chemotherapy-related myelosuppression in
a safe and effective manner. In addition, UCB-HSC infusion was
shown to significantly ease the symptoms of myelosuppression;
however, the therapy was more effective in male patients and
patients with a good KPS status. In order to achieve greater
therapeutic benefits, increasing the number of UCB-HSCs in each
infusion, or the number of infusions, may be considered. Further
research into the subgroup differences observed in the present
study and potential strategies for increasing the number of stem
cells delivered per infusion are currently under investigation.
Acknowledgements
The authors thank all the individuals who
participated in the study. The study would not have been possible
without the cooperation of the patients and their families, the
donors, and the assistance of the doctors and nurses at the Cancer
Center of Renmin Hospital of Wuhan University.
References
|
1
|
Yeshurun M, Labopin M, Blaise D, et al:
Impact of postremission consolidation chemotherapy on outcome after
reduced-intensity conditioning allogeneic stem cell transplantation
for patients with acute myeloid leukemia in first complete
remission: a report from the Acute Leukemia Working Party of the
European Group for Blood and Marrow Transplantation. Cancer.
120:885–863. 2014.
|
|
2
|
Dale DC, McCarter GC, Crawford J and Lyman
GH: Myelotoxicity and dose intensity of chemotherapy: reporting
practices from randomized clinical trials. J Natl Compr Canc Netw.
1:440–454. 2003.PubMed/NCBI
|
|
3
|
Zhong XY, Zhang B, Asadollahi R, et al:
Umbilical cord blood stem cells: what to expect. Ann NY Acad Sci.
1205:17–22. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wagner JE and Gluckman E: Umbilical cord
blood transplantation: the first 20 years. Semin Hematol. 47:3–12.
2010.PubMed/NCBI
|
|
5
|
Sun HP, Zhang X, Chen XH, et al: Human
umbilical cord blood-derived stromal cells are superior to human
umbilical cord blood-derived mesenchymal stem cells in inducing
myeloid lineage differentiation in vitro. Stem Cells Dev.
21:1429–1440. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yang WZ, Zhang Y, Wu F, et al: Safety
evaluation of allogeneic umbilical cord blood mononuclear cell
therapy for degenerative conditions. J Transl Med. 8:752010.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhang XZ, Xu YL and Tian R: The research
and application of cord blood plasma. Lin Chuang Xue Ye Xue Za Zhi.
1:39–40. 2003.(In Chinese).
|
|
8
|
Liao C, Liu B and Huang Y: Establishment
of cord blood stem cell bank and its clinical application. Zhonghua
Xue Ye Xue Za Zhi. 22:411–414. 2001.(In Chinese).
|
|
9
|
Isasi R, Dalpe G and Knoppers BM:
Fostering public cord blood banking and research in Canada. Stem
Cells Dev. 22(Suppl 1): 29–34. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wang BH, Zhang MZ, Fu XR, et al:
Pathogenesis, prevention and treatment of chemotherapy and
radiotherapy induced myelosuppression: the state of the art. Zhong
Liu Ji Chu Yu Lin Chuang Za Zhi. 26:162–165. 2013.(In Chinese).
|
|
11
|
Duong CD and Loh JY: Laboratory monitoring
in oncology. J Oncol Pharm Pract. 12:223–236. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lv M and Huang XJ: Allogeneic
hematopoietic stem cell transplantation in China: where we are and
where to go. J Hematol Oncol. 5:102012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Riordan NH, Chan K, Marleau AM and Ichim
TE: Cord blood in regenerative medicine: do we need immune
suppression. J Transl Med. 5:82007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Jiang XF, Wang GZ, Li GX, et al:
Transplantation of unrelated donor umbilical cord blood in 28
patients with malignant hematopathy. Zhonghua Xue Ye Xue Za Zhi.
27:279–280. 2006.(In Chinese).
|
|
15
|
Gu DS, Liu B and Han ZC: The research and
application of cord blood stem cells. Zhongguo Ke Xue Yuan Sheng Wu
Ke Xue Yu Ji Shu Ju. 18:323–327. 2006.(In Chinese).
|
|
16
|
Wang XH, Zhang XZ, Shi HZ, et al: The
evaluation of Epo, G-CSF, IL-2, IL-6 in cord blood plasma. Zhonghua
Xue Ye Xue Za Zhi. 11:391999.(In Chinese).
|
|
17
|
Biesecker LG and Emerson SG: Interleukin-6
is a component of human umbilical cord serum and stimulates
hematopoiesis in embryonic stem cells in vitro. Exp Hematol.
21:774–778. 1993.PubMed/NCBI
|
|
18
|
Sanders M, Sorba S and Dainiak N:
Insulin-like growth factors stimulate erythropoiesis in
serum-substituted umbilical cord blood cultures. Exp Hematol.
21:25–30. 1993.PubMed/NCBI
|
|
19
|
Carow CE, Hangoc G and Broxmeyer HE: Human
multipotential progenitor cells (CFU-GEMM) have extensive replating
capacity for secondary CFU-GEMM: an effect enhanced by cord blood
plasma. Blood. 81:942–949. 1993.
|
|
20
|
An YH, Zhou RX, Zhang GJ, et al:
Transplantation of cord blood hematopoietic stem cells: effects on
marrow function of cancer patients on chemotherapy. Qingdao Da Xue
Yi Xue Yuan Xue Bao. 36:88–90. 2000.(In Chinese).
|