Introduction
The principal mechanisms underlying the development
of coronary artery atherosclerosis and myocardial infarction (MI)
are numerous and complex. Coronary artery disease (CAD) is
associated with significant patient morbidity and mortality. A
larger infarction size and greater mortality are associated with
ST-segment elevation myocardial infarction (STEMI) compared with
non-STEMI (1).
Inflammation is increasingly being considered as a
key player and critical feature in coronary atherosclerosis
(2). Previous studies have
observed that areas of plaque rupture are associated with increased
levels of inflammatory cells (3,4). In
addition, coronary plaques have been observed to be infiltrated by
diffused inflammatory cells, including neutrophils, in patients who
succumbed following MI (3,5). The neutrophil/lymphocyte ratio is
known to be an important predictor of adverse outcomes in MI
(6).
Factors that promote endothelial dysfunction,
inflammatory reactions and platelet aggregation may result in
vascular dysfunction and atherosclerosis. Plasma levels of
inflammatory biomarkers such as C-reactive protein (CRP) have been
shown to increase and predict atherothrombotic events (7) suggesting that inflammation
contributes to MI (2).
Neutrophils are an important source of the
myeloperoxidase enzyme (MPO), a peroxidase and an inflammatory
factor. MPO is present in atherosclerotic plaques and may aggravate
cardiac ischemia (8). MPO has been
shown to promote the oxidation of low density protein (LDL)
(9) and apolipoprotein A-I
(10), thus, reducing its ability
to cause cholesterol efflux. Additionally, MPO promotes endothelial
dysfunction (11) and
apoptosis/detachment, promoting plaque rupture (2,12).
Thus, MPO may mediate the development of atherosclerotic plaques in
patients with CAD and may increase the risk of acute coronary
syndrome (ACS) (13). However, it
is unclear whether the plasma MPO (pMPO) level predicts the
severity of CAD and the coronary intervention required for the
reperfusion of atherosclerotic arteries.
The goal of the present study was to assess the
correlation of the pMPO level and neutrophil/lymphocyte ratio with
clinical characteristics, the need for coronary reperfusion and the
left ventricular ejection fraction (LVEF) prior to coronary
angiography in patients with CAD.
Methods
Patient selection
Inclusion criteria of this study were patients who
presented to King Abdullah University Hospital (KAUH; Irbid,
Jordan) with chest pain (angina) or recent MI (presented within
less than a week of the onset of symptoms). The majority of the
patients were referred from peripheral hospitals to KAUH and
underwent coronary angiograms for diagnosis and/or reperfusion when
required by percutaneous coronary intervention (PCI) or coronary
artery bypass graft surgery (CABG).
All included patients provided written informed
consent, and the study was conducted with approval from the
Institutional Review Board of KAUH. Demographic/clinical
characteristics and laboratory tests were obtained prospectively
from patients and from their medical records. Plasma lipids levels,
inflammatory cell percentages (neutrophils, lymphocytes and
monocytes), and glucose levels were obtained from patients’ data
registry at KAUH. Data concerning ejection fraction, left atrial
(LA) size, need for revascularization, and the use of medication
prior to hospitalization were also collected at baseline (for 210
patients) and at 30 days follow-up (for 100 patients). A detailed
clinical history, physical examination and relevant laboratory
investigations were used to confirm the presence of CAD or MI.
Levels of the cardiac biomarkers troponin I,
troponin T, creatine kinase (CK) and/or CK-MB, were measured to
document MI. The diagnosis of MI was established according to World
Health Organization (14) and
American Heart Association/American College of Cardiology criteria
(1), with a history of chest pain
lasting >20 min, the presence of cardiac enzyme leakage and
characteristic electrocardiogram (ECG) changes. The presence of an
elevated ST segment/Q wave on the ECG indicates STEMI. Angina was
defined as chest pain at rest or during exertion with a slight or
significant limitation of daily physical activity. Exclusion
criteria were patients with recent infection, patients with heart
failure (HF) without evidence of CAD, and patients who had suffered
an MI attack within the month prior to their current chest pain or
MI.
Echocardiographic and coronary
angiographic analysis
Echocardiographic studies were conducted using a two
dimensional imaging system [ALT (model HD1) 6,000 ht with a 2–4 MHz
probe; Philips Medical Systems, Inc., Bothell, WA, USA] to evaluate
the LA diameter (size) and LVEF. The LA size was indexed to the
body surface area. Coronary catheterization was used to confirm the
presence of CAD (coronary occlusion ≥50%) in one or more of the
main coronary arteries.
Blood collection
Blood was collected from the femoral artery in EDTA
tubes during femoral artery puncture prior to catheterization and
before the administration of adjunctive drug therapy for all
patients. Samples were brought to the laboratory immediately and
centrifuged at 700 × g for 15 min to separate the plasma. Samples
were stored at −80°C until the analysis of pMPO.
pMPO measurements
pMPO concentrations prior to catheterization were
determined using instant enzyme-linked immunoassays (BMS2038INST;
eBioscience, Inc., Vienna, Austria). Human plasma samples (diluted
1:50), controls and standards were pipetted in wells coated with
biotin-conjugated mouse anti-human MPO monoclonal antibody bound to
streptavidin-horseradish peroxidase and incubated on a horizontal
shaker at 400 rpm at room temperature. Standards and samples were
assayed in duplicate. Following 3 h of incubation, the contents of
the wells were washed, and then 100 μl tetramethylbenzidine (TMB)
substrate was added for 10 min followed by 100 μl stop solution.
Absorbance values were immediately determined using an ELISA reader
(EL×800, Bio-tek instruments, Winooski, VT, USA) at 450 nm, using
620 nm absorbance as a reference. The quantity of MPO was
interpolated from a calibration curve of standards. The assay was
sensitive (lower limit of detection, 0.026 ng/ml), specific and
reproducible with calculated overall inter- and intra-assay
coefficients of variation of <10 and <6%; respectively.
Plasma inflammatory cell
measurements
Plasma levels of white blood cells (WBCs) and
percentages of neutrophils, lymphocytes and monocytes were measured
using a Beckman Coulter (LH 780) Hematology Analyzer (Coulter
Technology Center, Miami, FL, USA).
Statistical analysis
Continuous variables are presented as mean ±
standard error of the mean (SEM) while categorical data are
presented as numbers and percentages. Univariate and multivariate
analyses were used to evaluate the association of demographic and
clinical parameters with pMPO levels and the neutrophil/lymphocyte
ratio. Normally distributed variables were analyzed using analysis
of variance or t-test. Non-normally distributed variables were
analyzed using Mann-Whitney U test and Kruskal-Wallis test. To
compare frequencies among study groups, the Chi-square test was
used. Spearman’s correlation was used to assess the correlation
between variables. Univariate analysis was performed and figures
created using GraphPad Prism 5 (GraphPad Software, Inc., La Jolla,
CA, USA). pMPO levels were not normally distributed; thus, a log
transformation of MPO levels was used in the multivariate analysis
to normalize the dataset. Multivariate analyses were performed
using JMP11 software (SAS Institute Inc., Cary, NC, USA). P<0.05
was considered to indicate a statistically significant
difference.
Results
Patient characteristics
Plasma samples from 210 patients were used for the
biochemical analysis of MPO protein levels and inflammatory cell
measurements. Study groups were stratified based on their clinical
presentation, coronary angiographic findings and cardiac enzyme
levels. The study groups comprised: i) patients who presented with
negative cardiac enzymes and normal main coronary arteries with
<50% stenosis (CAD <50% group, n=60), ii) patients with
negative cardiac enzymes and CAD with ≥50% stenosis in one or more
of the main coronary arteries (CAD ≥50% group, n=68); and iii)
patients that presented with recent MI (within the last week) as
documented by cardiac enzyme leakage and coronary angiogram (MI
group, n=82). The MI group was further subdivided into two groups
based on ECG findings: STEMI (n=41) and non-STEMI (n=41). Certain
STEMI patients (n=27) had received thrombolytic agents prior to
referral to KAUH. Patients with recent MI underwent emergency
catheterization (within <24 h, 42%) or elective catheterization
(within 24 h to 1 week, 57%). A total of 11 patients were scheduled
for CABG. Hypertension (HT) and diabetes mellitus (DM) were present
in 67.9 and 42.4% of patients, respectively (Table I). There were 25 patients that
presented with heart failure (HF), seven of whom had CAD and 18 of
whom had MI. The majority of patients with MI presented with acute
HF (n=15) whereas three patients with MI and seven patients with
CAD presented with a history of chronic HF.
 | Table IPatients characteristics. |
Table I
Patients characteristics.
| Variables | CAD <50%
(n=60) | CAD ≥50% (n=68) | MI (n=82) | P-value |
|---|
| Clinical
characteristics |
| Age, years | 53.7±1.44 | 60.7±1.38 | 56.1±1.17 | 0.0012a |
| Male gender, n
(%) | 27 (45.0) | 46 (67.6) | 68 (82.9) | <0.0001a |
| Body mass index | 30.33±0.87 | 28.88±0.70 | 28.46±0.51 | 0.1440 |
| Hypertension, n
(%) | 46 (77.9) | 53 (77.9) | 43 (52.4) | 0.0006a |
| Heart failure, n
(%) | 0 (0) | 7 (10.2) | 18 (21.9) | 0.0003a |
| Diabetes mellitus, n
(%) | 22 (36.6) | 35 (53.0) | 30 (37.9) | 0.1057 |
| Current smoking, n
(%) | 20 (33.9) | 25 (36.7) | 47 (57.3) | 0.0075a |
| Laboratory tests |
| White blood cell
count | 8.23±0.30 | 7.77±0.29 | 9.77±0.38 | 0.0003a |
| Neutrophils % | 63.55±1.25 | 62.33±1.17 | 68.00±1.68 | 0.0486a |
| Monocytes % | 6.59±0.26 | 8.54±1.54 | 7.94±0.45 | 0.0921 |
|
Neutrophils/lymphocytes | 2.72±0.19 | 2.61±0.17 | 4.75±0.93 | 0.0143a |
| Low density
lipoprotein, mmol/l | 3.29±0.18 | 2.81±0.15 | 3.17±0.13 | 0.0655 |
| High density
lipoprotein, mmol/l | 1.08±0.04 | 1.00±0.04 | 0.91±0.02 | 0.0112a |
| Triglycerides,
mmol/l | 2.19±0.15 | 2.44±0.21 | 2.35±0.17 | 0.7831 |
| Total cholesterol,
mmol/l | 4.95±0.20 | 4.39±0.15 | 4.73±0.14 | 0.0669 |
| Fasting plasma
glucose | 7.44±0.54 | 10.67±0.92 | 8.24±0.64 | 0.0145a |
| HBA1C | 6.83±0.32 | 7.41±0.34 | 7.05±0.36 | 0.5085 |
| Intervention, n
(%) |
| PCI | 0 (0) | 47 (69.1) | 65 (79.2) | <0.0001a |
| Coronary artery
bypass graft | 0 (0) | 4 (5.8) | 7 (8.6) | 0.0820 |
| Pre-operative
echocardiographic data |
| Indexed LA diameter,
cm/m2 | 2.04±0.05 | 2.09±0.06 | 2.01±0.03 | 0.8892 |
| Left ventricular
ejection fraction | 56.45±0.93 | 50.57±1.41 | 46.60±1.39 | <0.0001a |
| Pre-operative use of
medication, n (%) |
| ACE inhibitors | 22 (36.6) | 20 (29.8) | 17 (20.7) | 0.1070 |
| ARBs | 12 (20.0) | 13 (19.4) | 6 (7.3) | 0.0487a |
| Diuretics | 14 (23.3) | 16 (23.8) | 9 (10.9) | 0.0722 |
| β blockers | 37 (61.6) | 40 (59.7) | 33 (40.2) | 0.0153a |
| Statins | 33 (55.0) | 47 (70.1) | 33 (40.2) | 0.0011a |
| Aspirin | 51 (86.4) | 56 (82.3) | 40 (48.7) | <0.0001 |
Univariate predictors of pMPO and
inflammatory cell levels
pMPO and inflammatory cell levels were evaluated as
factors in the clinical manifestation of CAD (CAD status graded as
0, CAD with <50% stenosis; 1, CAD ≥50%; and 2, MI) and the
clinical outcome.
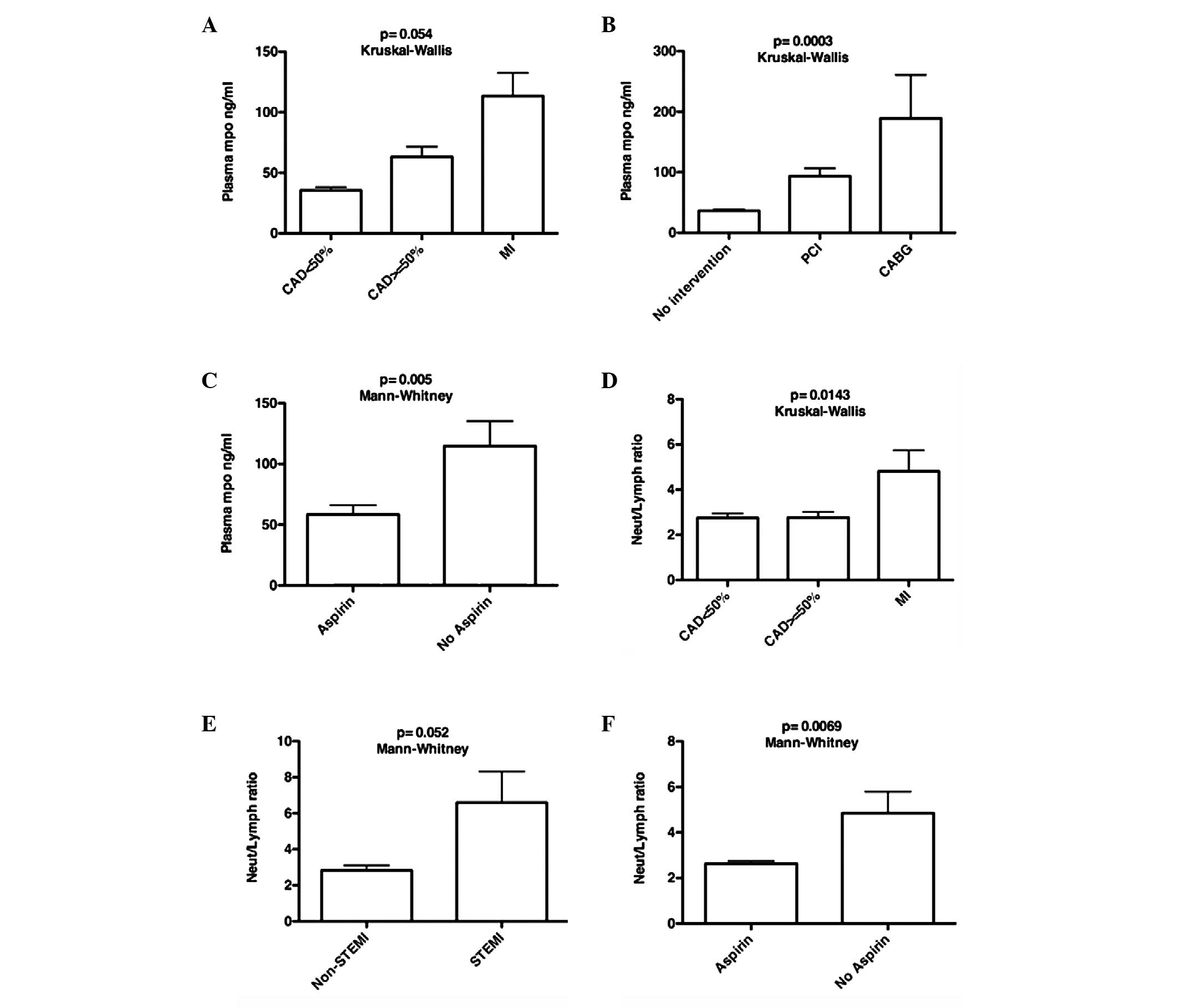
The levels of pMPO in patients with recent MI were
higher than those in patients with CAD ≥50% and those with <50%
coronary artery stenosis (mean ± SEM, 113.39±19.16, 63.134±8.40 and
35.61.±2.62 ng/ml, respectively; P=0.054, Kruskal-Wallis test;
Fig. 1A). The pMPO levels were not
statistically different between the STEMI and non-STEMI groups
(146.878±33.98 vs. 79.905±16.64 ng/ml; P=0.696, Mann-Whitney test).
The pMPO levels also did not differ in patients with STEMI
according to whether they received or did not receive thrombolytic
agents, or among those who underwent elective or emergency
catheterization (P<0.05). pMPO levels were higher in patients
who were scheduled for CABG compared to those in patients who
underwent PCI or no intervention (189.01±71.76, 93.75±12.96,
36.20±2.31 ng/ml, respectively; P=0.0003, Kruskal-Wallis test;
Fig. 1B). pMPO levels in patients
who took aspirin prior to hospitalization were lower compared with
those in patients who did not take aspirin (58.47±7.70 vs.
114.76±20.52 ng/ml; P=0.005, Mann-Whitney test; Fig. 1C).
The white blood cell count (WBC) and neutrophil
percentage were higher in the MI group compared with those in the
CAD <50% and CAD ≥50% groups (Table
I). The neutrophil/lymphocyte ratio also correlated with CAD
status (4.75±0.93, 2.61±0.17 and 2.72±0.19 in the MI, CAD≥50% and
CAD<50% groups, respectively; P=0.0143, Kruskal-Wallis test;
Fig. 1D). The
neutrophil/lymphocyte ratio was higher in patients with STEMI than
in patients with non-STEMI (6.59±1.73 vs. 2.83±0.27, respectively;
P=0.052, Mann-Whitney test; Fig.
1E) and tended to be higher in patients who were scheduled for
CABG relative to patients who required PCI or no intervention
(5.33±1.42, 3.46±0.54 and 2.72±0.15; respectively; P=0.07,
Kruskal-Wallis test). Patients who were taking aspirin had a lower
plasma neutrophil percentage relative to those who were not taking
aspirin (63.02±0.82 vs. 67.66±1.84%; P=0.047, Mann-Whitney test)
and had a lower neutrophil/lymphocyte ratio (2.62±0.12 vs.
4.88±0.96; P=0.0069, Mann-Whitney test; Fig. 1F).
The pMPO level was not identified to be associated
with HF (regardless of chronic or acute presentation),
hypertension, diabetes, smoking, indexed LA size, use of statins
prior to admission to hospital, angiotensin converting enzyme
inhibitors (ACEi)/receptor blockers (ARBs), or β blockers. However,
the pMPO level was found to be positively correlated with the
neutrophil percentage (Spearman’s r=0.207, P=0.0115) and the
neutrophil/lymphocyte ratio (r=0.253, P=0.0019), but not with the
WBC count (P=0.226) or monocyte percentage (P=0.523). In addition,
the pMPO level did not correlate with the baseline LVEF (P=0.212),
or the levels of high density lipoprotein (HDL; P=0.35), LDL
(P=0.588) or total cholesterol (P=0.148). However, plasma
inflammatory cells were negatively correlated with the baseline
LVEF; WBC (r=−0.145, P=0.073), the neutrophil percentage (r=−0.204,
P=0.027), the neutrophil/lymphocyte ratio (r=−0.264, P=0.004) and
monocyte percentage (r=−0.227, P=0.0137). The plasma
neutrophil/lymphocyte ratio correlated with HF (2.94±0.18 vs.
6.13±2.23; P=0.044, Mann-Whitney test) and tended to be higher in
patients with acute HF (8.39±4.08).
Independent predictors of pMPO level
Multivariate analysis was performed to determine
independent predictors of pMPO level. By step-wise analysis, it was
identified that diabetes, HF, LVEF, HT, smoking, plasma lipids, and
the use of ACEi/ARBs, statins or β blockers did not correlate with
pMPO level; thus, they were excluded from the final model. By
step-wise analysis adjusting for age, BMI and gender, pMPO was
found to be associated with CAD status (graded as 0, CAD <50%
stenosis; 1, CAD ≥50% stenosis; 2, MI; P=0.008). As the CAD status
was collinear with coronary intervention (graded as 0, no
intervention; 1, PCI; 2, CABG), it was not presented in the final
model to avoid masking the correlation of pMPO with coronary
intervention. Adjusting for age, gender and BMI, multivariate
analysis showed that the neutrophil/lymphocyte ratio and coronary
intervention were significantly and positively associated with the
pMPO level (Table II). Notably,
this analysis revealed that patients who took aspirin had lower
pMPO levels than patients who did not take aspirin (P=0.0155).
 | Table IIMultivariate factors associated with
plasma MPO content. |
Table II
Multivariate factors associated with
plasma MPO content.
| Response = log
plasma MPO ng/ml |
|---|
|
|
|---|
| Variable | Estimate (slope,
B) | Standard error | P-value | Standardized
coefficient (β) |
|---|
| Age, years | 0.0004 | 0.0060 | 0.9417 | 0.07 |
| Female gender | −0.0825 | 0.1517 | 0.5875 | −0.54 |
| BMI | 0.0004 | 0.0115 | 0.6849 | 0.41 |
|
Neutrophil/lymphocyte ratio | 0.0866 | 0.0202 | <0.0001a | 4.27 |
| Coronary
intervention | 0.1561 | 0.0676 | 0.0224a | 2.31 |
| Use of aspirin | −0.3359 | 0.1652 | 0.0439a | −2.03 |
Independent predictors of the plasma
neutrophil/lymphocyte ratio
Multivariate analysis was used to evaluate
independent predictors of the plasma neutrophil/lymphocyte ratio.
By step-wise analysis, it was identified that diabetes, HT,
smoking, plasma lipids, and the use of ACEi/ARBs, β blockers or
statins did not correlate with the neutrophil/lymphocyte ratio;
thus, they were excluded from the model. By step-wise analysis
adjusting for age, BMI, and gender, the neutrophil/lymphocyte ratio
was found to be associated with CAD status (P=0.018) and coronary
intervention (P=0.05). As both CAD status and coronary intervention
were collinear with LVEF, they were excluded from the final model
to avoid masking the correlation of LVEF with the
neutrophil/lymphocyte ratio. Adjusting for age, gender and BMI,
multivariate analysis showed that both baseline LVEF and the use of
aspirin were negatively correlated with the neutrophil/lymphocyte
ratio (Table III). Similarly, HF
was also independently associated with the neutrophil/lymphocyte
ratio (P<0.0001), but was not presented in the model due to it
being collinear with LVEF.
 | Table IIIMultivariate factors associated with
plasma neutrophils/lymphocytes ratio. |
Table III
Multivariate factors associated with
plasma neutrophils/lymphocytes ratio.
| Response =
neutrophil/lymphocyte ratio |
|---|
|
|
|---|
| Variable | Estimate (slope,
B) | Standard error | P-value | Standardized
coefficient (β) |
|---|
| Age, years | −0.0166 | 0.0304 | 0.5639 | −0.55 |
| Female gender | −0.1278 | 0.7583 | 0.8666 | −0.17 |
| BMI | 0.0331 | 0.0615 | 0.5916 | 0.54 |
| Baseline LVEF | −0.1065 | 0.0349 | 0.0029a | −3.05 |
| Use of aspirin | −1.8282 | 0.7644 | 0.0185a | −2.39 |
Prognostic value of the baseline pMPO
level and the neutrophil/lymphocyte ratio at the 30 day
follow-up
A total of 100 patients (41 from the MI group, 34
from the CAD ≥50% group and 25 from the CAD <50% group) were
followed up for clinical assessment 30 days after angiography. Two
patients required coronary reperfusion; one presented with
recurrent MI (pMPO, 12.71 ng/ml) and one presented with restenosis
requiring PCI (pMPO, 21.19 ng/ml). One patient who presented with
recurrent angina underwent angiography without need for stenting
(pMPO, 293.19 ng/ml). By multivariate analysis adjusting for age,
gender, BMI and smoking, the baseline pMPO was not associated with
LVEF at 30 days or with the change in LVEF at the 30-day follow-up
(P>0.05; data not shown). The plasma neutrophil/lymphocyte ratio
was correlated negatively with LVEF after 30 days (Spearman’s
r=−0.402, P=0.0007), but was not associated with the change in LVEF
after 30 days (P=0.251). By this time, the increase in LVEF was
minimal and not significant (mean % increase in LVEF: all patients,
3.11%±1.34, P=0.53; CAD <50%, 1.28±2.22; CAD ≥50%, 1.22±2.57;
and MI, 5.55±2.10; P=0.18, Kruskal-Wallis).
Adjusting for age, BMI, gender and use of aspirin,
the pMPO and neutrophil/lymphocyte ratio were not found to be
associated with the change in LVEF at the 30-day follow-up (P=0.240
and P=0.812, respectively; data not shown).
Discussion
MPO, an enzyme derived from activated neutrophils
and monocytes, is involved in the generation of reactive oxygen
species (ROS) and nitric oxide-derived oxidants (8). Thus, MPO promotes inflammation and
oxidative stress and contributes to endothelial dysfunction and
plaque formation, rupture and ventricular remodeling following MI
(3,12).
The levels and activity of pMPO have been reported
to increase in MI patients (15,16)
and to predict endothelial dysfunction (11), the risk of ACS (13,17)
and mortality (15). In addition,
high pMPO levels have been shown to predict 30-day mortality and
major adverse clinical events in patients with STEMI (18–20)
and long-term adverse clinical events in stable cardiac patients
(19). However, it is not known
whether this relationship is similar for other clinical
presentations of CAD. In the present study, it was found that pMPO
levels were elevated in the patients with recent MI compared with
those in patients with or without CAD and correlate with the
neutrophil/lymphocyte ratio, suggesting that the increased
circulatory neutrophils promote MPO release, plaque formation and
the development of MI. Neutrophil infiltration is actively
associated with plaque rupture and MI (3). The neutrophil/lymphocyte ratio is
known to be as strong predictor of adverse outcomes in patients
with STEMI (6). Notably, in the
present study, the neutrophil/lymphocyte ratio was correlated with
CAD status and was higher in STEMI than non-STEMI. As MPO is
derived from activated neutrophils and monocytes, a higher pMPO
level in patients with STEMI relative to those with non-STEMI was
expected; however, the differences in data did not reach
statistical significance.
The current study provides important insights
regarding the pathophysiologic significance of pMPO in patients
with CAD. One important finding is that the pMPO level is higher in
patients undergoing CABG than in those undergoing PCI or no
intervention. Similarly, the neutrophil/lymphocyte ratio was found
to correlate with the type of coronary intervention, suggesting
that plasma inflammatory neutrophils and MPO contribute
significantly to the extent and severity of CAD and could be used
clinically to predict the appropriate choice of clinical
intervention required for the reperfusion of atherosclerotic
arteries.
Aspirin is a commonly prescribed anti-platelet
non-steroidal anti-inflammatory drug (NSAID) for preventing ACS and
mortality in CAD patients. The effects of NSAIDs occur through the
inhibition of prostaglandin H synthase, which is produced from
arachidonic acid via the actions of cyclooxygenase and peroxidase
(21). In the present study, the
use of aspirin was identified to be associated with a reduced
neutrophil/lymphocyte ratio and lower levels of pMPO, which might
further explain the use of aspirin and its benefits in the
prevention of MI and mortality. Similarly, the use of aspirin has
previously been shown to reduce MPO activity (22) and neutrophil levels (23).
LVEF is an important determinant of cardiac function
and a predictor of morbidity and mortality (24). In the present study, the pMPO
levels were not correlated with baseline LVEF, 30-day follow-up
LVEF or the change in LVEF during follow-up. However, inflammatory
cell percentages, including the neutrophil/lymphocyte ratio, were
significantly correlated with HF, and with baseline and 30-day
LVEF. A previous study identified a correlation between LVEF and
WBC count (18), clearly
indicating that inflammation is significant in LV dysfunction and
the development of HF. The lack of a correlation between pMPO and
LVEF suggests the presence of other inflammatory mediators that may
contribute more significantly to LVEF. The changes in LVEF at 30
days were not significant, which might also explain the lack of
correlations of the pMPO level and neutrophil/lymphocyte ratio with
changes in LVEF after 30 days.
The present study demonstrates an association of
pMPO with MI in relation to patients with and without CAD who have
a low risk of ACS compared with other groups.
However, the present study does not provide
information regarding the kinetics of the increase and decrease of
pMPO levels. One limitation of the study is the inclusion of
patients with MI who presented within a week and received drug
therapies that might have affected the pMPO levels. However, pMPO
levels were not different between patients who received
thrombolytics relative and those who did not receive them.
Similarly, pMPO levels have been shown to be similar in patients
with MI regardless the use of thrombolytic therapy (25).
MPO is a key inflammatory mediator associated with
MI, the neutrophil/lymphocyte ratio and the type of coronary
intervention, suggesting that it may contribute to inflammation and
the increased risk, severity, and extent of CAD in patients. The
association of the neutrophil/lymphocyte ratio with low ejection
fraction further suggests that inflammation promotes the
development of ventricular dysfunction and HF in patients with CAD.
The use of interventions that reduce pMPO production, such as
aspirin, limit MI development and related adverse outcomes. This
study suggests the use of pMPO levels and the neutrophil/lymphocyte
ratio as CAD risk markers and clinical predictors for reperfusion
by PCI or CABG. It may also help with the selection of patients who
may benefit from use of additional treatments that reduce pMPO and
neutrophil levels.
Acknowledgements
This study was supported by the deanship of research
at Jordan University of Science and Technology, Irbid, Jordan.
References
|
1
|
Fitchett DH, Theroux P, Brophy JM, et al:
Assessment and management of acute coronary syndromes (ACS): a
Canadian perspective on current guideline-recommended treatment -
part 2: ST-segment elevation myocardial infarction. Can J Cardiol.
27(Suppl A): S402–S412. 2011. View Article : Google Scholar
|
|
2
|
Duivenvoorden R, Mani V, Woodward M, et
al: Relationship of serum inflammatory biomarkers with plaque
inflammation assessed by FDG PET/CT: the dal-PLAQUE study. JACC
Cardiovasc Imaging. 6:1087–1094. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Naruko T, Ueda M, Haze K, et al:
Neutrophil infiltration of culprit lesions in acute coronary
syndromes. Circulation. 106:2894–2900. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
van der Wal AC, Becker AE, van der Loos CM
and Das PK: Site of intimal rupture or erosion of thrombosed
coronary atherosclerotic plaques is characterized by an
inflammatory process irrespective of the dominant plaque
morphology. Circulation. 89:36–44. 1994.
|
|
5
|
Mauriello A, Sangiorgi G, Fratoni S, et
al: Diffuse and active inflammation occurs in both vulnerable and
stable plaques of the entire coronary tree: a histopathologic study
of patients dying of acute myocardial infarction. J Am Coll
Cardiol. 45:1585–1593. 2005. View Article : Google Scholar
|
|
6
|
Kaya MG, Akpek M, Lam YY, et al:
Prognostic value of neutrophil/lymphocyte ratio in patients with
ST-elevated myocardial infarction undergoing primary coronary
intervention: a prospective, multicenter study. Int J Cardiol.
168:1154–1159. 2013. View Article : Google Scholar
|
|
7
|
Danesh J, Wheeler JG, Hirschfield GM, et
al: C-reactive protein and other circulating markers of
inflammation in the prediction of coronary heart disease. N Engl J
Med. 350:1387–1397. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zhang R, Brennan ML, Shen Z, et al:
Myeloperoxidase functions as a major enzymatic catalyst for
initiation of lipid peroxidation at sites of inflammation. J Biol
Chem. 277:46116–46122. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Podrez EA, Schmitt D, Hoff HF and Hazen
SL: Myeloperoxidase-generated reactive nitrogen species convert LDL
into an atherogenic form in vitro. J Clin Invest. 103:1547–1560.
1999. View
Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zheng L, Nukuna B, Brennan ML, et al:
Apolipoprotein A-I is a selective target for
myeloperoxidase-catalyzed oxidation and functional impairment in
subjects with cardiovascular disease. J Clin Invest. 114:529–541.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Vita JA and Loscalzo J: Shouldering the
risk factor burden: infection, atherosclerosis, and the vascular
endothelium. Circulation. 106:164–166. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sugiyama S, Kugiyama K, Aikawa M, et al:
Hypochlorous acid, a macrophage product, induces endothelial
apoptosis and tissue factor expression: involvement of
myeloperoxidase-mediated oxidant in plaque erosion and
thrombogenesis. Arterioscler Thromb Vasc Biol. 24:1309–1314. 2004.
View Article : Google Scholar
|
|
13
|
Tang WH, Wu Y, Nicholls SJ and Hazen SL:
Plasma myeloperoxidase predicts incident cardiovascular risks in
stable patients undergoing medical management for coronary artery
disease. Clin Chem. 57:33–39. 2011. View Article : Google Scholar
|
|
14
|
Proposal for the multinational monitoring
of trends and determinants in cardiovascular disease and protocol
(MONICA Project). WHO/MNC/821. Cardiovascular Disease Unit, World
Health Organization; Geneva: 1982
|
|
15
|
Cavusoglu E, Ruwende C, Eng C, et al:
Usefulness of baseline plasma myeloperoxidase levels as an
independent predictor of myocardial infarction at two years in
patients presenting with acute coronary syndrome. Am J Cardiol.
99:1364–1368. 2007.
|
|
16
|
Zhang R, Brennan ML, Fu X, et al:
Association between myeloperoxidase levels and risk of coronary
artery disease. JAMA. 286:2136–2142. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Baldus S, Heeschen C, Meinertz T, et al;
CAPTURE Investigators. Myeloperoxidase serum levels predict risk in
patients with acute coronary syndromes. Circulation. 108:1440–1445.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Chang LT, Chua S, Sheu JJ, et al: Level
and prognostic value of serum myeloperoxidase in patients with
acute myocardial infarction undergoing primary percutaneous
coronary intervention. Circ J. 73:726–731. 2009. View Article : Google Scholar
|
|
19
|
Dominguez-Rodriguez A, Samimi-Fard S,
Abreu-Gonzalez P, Garcia-Gonzalez MJ and Kaski JC: Prognostic value
of admission myeloperoxidase levels in patients with ST-segment
elevation myocardial infarction and cardiogenic shock. Am J
Cardiol. 101:1537–1540. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kaya MG, Yalcin R, Okyay K, et al:
Potential role of plasma myeloperoxidase level in predicting
long-term outcome of acute myocardial infarction. Tex Heart Inst J.
39:500–506. 2012.PubMed/NCBI
|
|
21
|
Miura T: Direction of strategic use: a new
classification of non-steroidal anti-inflammatory drugs based on
reactivity with peroxidase. Yakugaku Zasshi. 133:681–689. 2013.(In
Japanese).
|
|
22
|
Coimbra LS, Steffens JP, Muscará MN, Rossa
C Jr and Spolidorio LC: Antiplatelet drugs reduce the
immunoinflammatory response in a rat model of periodontal disease.
J Periodontal Res. 2013.PubMed/NCBI
|
|
23
|
Eickmeier O, Seki H, Haworth O, et al:
Aspirin-triggered resolvin D1 reduces mucosal inflammation and
promotes resolution in a murine model of acute lung injury. Mucosal
Immunol. 6:256–266. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
King M, Kingery JE and Casey B: Diagnosis
and evaluation of heart failure. Am Fam Physician. 85:1161–1168.
2012.
|
|
25
|
Brügger-Andersen T, Hetland Ø, Ponitz V,
Grundt H and Nilsen DW: The effect of primary percutaneous coronary
intervention as compared to tenecteplase on myeloperoxidase,
pregnancy-associated plasma protein A, soluble fibrin and D-dimer
in acute myocardial infarction. Thromb Res. 119:415–421. 2007.
|