Introduction
Pleural effusion is commonly found in patients
suffering from various kinds of disease, and malignancy is one of
the most frequent causes of pleural effusion (1). Pleural effusion may occur with almost
all types of cancers, of which lung cancer is responsible for ~30%
of cases (2). The etiological
diagnosis and differential diagnosis between malignant pleural
effusion (MPE) and benign pleural effusion is of significant
importance due to the differences in treatment and prognosis
between these two types of pleural effusions. Development of MPE
usually defines advanced cancer with a poor prognosis, and
moreover, current strategies for the diagnosis of MPE are clearly
inadequate (3). As a standard
method for the diagnosis of MPE, conventional pleural fluid
cytology findings are positive in only 60% of cases on average
(4). Additionally, closed pleural
biopsy merely confers a small additive diagnostic value (5,6).
Thoracoscopy has a high diagnostic accuracy and is able to
establish the diagnosis in ~95% of cases; however, this
interventional procedure may not be well accepted among patients
and may not be available at all facilities (7).
Carbohydrate antigen 15-3 (CA 15-3), a glycoprotein
expressed in normal and malignant tissues, including breast, lung
and ovary cancer, has been found to be associated with malignancy
and its secretion is increased in the presence of a tumor (8). It is easily detected in various
biological specimens such as blood, serous liquid and tissue
samples (9). Thus an increasing
number of studies consider it to be a biomarker for diagnosing MPE
(10–12). Although the accuracy of CA 15-3 in
detecting MPE has been extensively studied, the precise diagnostic
value remains unclear. Therefore, the present meta-analysis was
performed to evaluate the overall accuracy of pleural CA 15-3 for
diagnosing MPE.
Materials and methods
Identification of studies
The databases Medline (using PubMed as the search
engine), Embase, Ovid, Web of Science and Cochrane database were
searched to identify relevant studies published up to December
2013. No lower date limit was applied. Relevant references of
articles were also searched manually. Relevant studies were
identified using any of the following keywords: ‘tumor marker’,
‘carbohydrate antigen 15-3’, ‘CA 15-3’, ‘malignant pleural
effusion’, ‘sensitivity’, ‘specificity’ and ‘accuracy’. The
language of publication was limited to English. A study was
included in the present meta-analysis if it provided both
sensitivity and specificity data of CA 15-3 for the diagnosis of
MPE. Letters to journal editors and conference abstracts, however,
were excluded due to limited data. Two authors independently
identified eligible studies when screening the searched studies.
Any disagreements were arbitrated by a third author.
Quality assessment
To assess the methodology of the included studies
(13–33), the present meta-analysis was
conducted in line with the Quality Assessment for Studies of
Diagnostic Accuracy (QUADAS) statement (34). Two authors independently evaluated
all included studies based on randomized sequence generation. Any
disagreements were arbitrated by a third author.
Data extraction
The data was extracted by two authors. The reviewers
were blinded to publication details, such as author details,
journal, patient characteristics, test method, cut-off value,
sensitivity, specificity and methodological quality. Additionally,
the following characteristics of study design for each article were
retrieved: a) cross-sectional design (versus case-control design);
b) consecutive or random sampling of patients; c) blinded (single
or double) interpretation of determination and reference standard
results; and d) prospective data collection. If no data on the
above criteria were reported in the primary studies, these were
treated as ‘Unknown’. Discrepancies were resolved by consensus.
When multiple publications of the same study were identified, data
was extracted as a single study.
Statistical analysis
Standard methods recommended to provide diagnostic
accuracy in meta-analyses were used (35). Then, the following indices of test
accuracy were calculated for each study: sensitivity, specificity,
positive likelihood ratio (PLR), negative likelihood ratio (NLR)
and diagnostic odds ratio (DOR).
The sensitivity and specificity of each single test
threshold identified for each study were used to plot a summary ROC
(SROC) (36,37). Spearman’s rank correlation was
performed as a test for threshold effect. The χ2 and
Fisher’s exact tests were used to detect statistically significant
heterogeneity across the studies. The average sensitivity,
specificity and other related measurements of the studies were
calculated using a random-effects model (38,39).
To assess the effects of QUADAS score on the diagnostic ability of
CA 15-3, it was included as a covariate in the meta-regression
analysis (inverse-variance weighted). Effects of other covariates
on DOR (cross-sectional design, consecutive or random sampling of
patients, blind design, prospective data collection and assay
method) were also analyzed. The relative DOR (RDOR) was calculated
according to standard methods to analyze the change in diagnostic
precision in the study per unit increase in the covariate (40,41).
Publication bias was tested using funnel plots and the Deeks’ test
(42). Statistical software
packages were used to perform the analysis (Stata, version 8.2,
Stata Corporation, College Station, TX, USA; Meta-Test version 0.6,
New England Medical Center, Boston, MA, USA; and Meta-DiSc for
Windows, XI Cochrane Colloquium, Barcelona, Spain).
Results
Description of studies
Following the literature search, a total of 164
studies regarding CA 15-3 and pleural effusion were considered to
be eligible for the present meta-analysis. Of these publications,
140 literature items that were beyond the scope of the present
study were excluded and three articles without a control group were
also excluded (43–45). Ultimately, 21 studies were selected
with a total of 2,861 patients. A flow chart showing the selection
of references for meta-analysis is shown in Fig. 1.
Quality of included studies
In present meta-analysis, the average sample size of
the included studies was 136 (range, 39 to 416). The diagnosis of
MPE was made based on cytological or/and pathological findings, as
the gold standard. Among the 21 studies, 15 (71.4%) had a
cross-sectional design; in 16 studies (76.2%), the samples were
collected from consecutive patients; 13 studies (61.9%) reported
blinded interpretation of CA 15-3 assays independent of the
reference standard; and 20 studies (95.2%) had a prospective study
design. There were 13 studies with QUADAS scores ≥10 (Table I). As shown in Table I, P≥0.05 indicates values that did
not reach statistical significance and these factors did not affect
diagnostic accuracy. The clinical characteristics and other
information are outlined in Tables
II and III.
 | Table IWeighted meta-regression of the
effects of methodological quality, study design and assay method on
diagnostic precision of pleural CA 15-3 in 21 assays. |
Table I
Weighted meta-regression of the
effects of methodological quality, study design and assay method on
diagnostic precision of pleural CA 15-3 in 21 assays.
| Covariates | No. of studies | Coefficient | RDOR (95% CI) | P-value |
|---|
| QUADAS ≥10 | 13 | −1.788 | 0.17 (0.01–3.50) | 0.226 |
| Cross-sectional
design | 15 | 0.515 | 1.67
(0.21–13.22) | 0.599 |
| Consecutive or
random | 16 | 1.351 | 3.86
(0.22–66.57) | 0.324 |
| Blinded | 13 | 2.353 | 10.51
(0.72–153.81) | 0.080 |
| Prospective | 19 | −1.154 | 0.32
(0.01–11.65) | 0.502 |
| Assay method
(EIA/non-EIA) | 7/14 | 0.198 | 1.22
(0.16–9.24) | 0.836 |
 | Table IISummary of included studies. |
Table II
Summary of included studies.
| Study/year
(ref.) | Patient no. | Assay method | Cut-off | Test results | QUADAS score |
|---|
|
|
|---|
| MPE | non-PE | TP | FP | FN | TN |
|---|
| Shimokata/1988
(13) | 40 | 41 | RIA | 16 U/ml | 15 | 0 | 25 | 41 | 12 |
| Lotzniker/1991
(14) | 22 | 17 | EIA | 25 U/ml | 10 | 2 | 12 | 15 | 7 |
| Romero/1996
(15) | 42 | 73 | EIA | 25 U/ml | 20 | 2 | 24 | 71 | 12 |
| Villena/1996
(16) | 65 | 142 | EIA | 42 U/ml | 36 | 1 | 75 | 129 | 12 |
| Miédougé/1999
(17) | 215 | 121 | RIA | 36.2 U/ml | 140 | 1 | 75 | 120 | 9 |
| Zimmerman/2000
(18) | 72 | 40 | EIA | Unknown | 65 | 4 | 7 | 36 | 10 |
| Alataş/2001
(19) | 44 | 30 | RIA | 14 U/ml | 35 | 2 | 9 | 28 | 13 |
| Villena/2003
(20) | 101 | 151 | EIA | 45 U/ml | 44 | 1 | 57 | 150 | 12 |
| Porcel/2004
(21) | 166 | 250 | RIA | 75U/ml | 50 | 0 | 116 | 250 | 12 |
| Ustün/2004
(22) | 41 | 40 | EIA | 30 U/ml | 21 | 10 | 20 | 30 | 8 |
| Ghayumi/2005
(23) | 40 | 37 | EIA | 21.1 U/ml | 28 | 6 | 12 | 31 | 12 |
| Shitrit/2005
(24) | 44 | 72 | EIA | 30 U/ml | 17 | 2 | 24 | 62 | 11 |
| Topolcan/2007
(25) | 81 | 77 | EIA | 7.6 kIU/l | 77 | 4 | 3 | 74 | 10 |
| Paşaoğlu/2007
(26) | 35 | 54 | EIA | 53 U/ml | 13 | 0 | 22 | 54 | 9 |
| Wagner/2007
(27) | 36 | 30 | ECIA | 22.38 ng/ml | 24 | 3 | 12 | 27 | 13 |
| Li/2007 (28) | 32 | 30 | EIA | 35 kU/l | 17 | 7 | 15 | 23 | 10 |
| Gaspar/2008
(29) | 40 | 84 | EIA | 62.4 IU/l | 16 | 55 | 24 | 29 | 11 |
| Creaney/2008
(30) | 76 | 30 | EIA | 53 kU/l | 24 | 0 | 52 | 30 | 8 |
| Terracciano/2010
(31) | 103 | 32 | EIA | 41 kU/l | 99 | 0 | 4 | 32 | 9 |
| Antonangelo/2010
(32) | 113 | 62 | ECIA | 27 kU/l | 64 | 5 | 49 | 57 | 8 |
| Farag/2012
(33) | 20 | 20 | ECIA | 35 kU/l | 16 | 7 | 4 | 13 | 7 |
 | Table IIICharacteristics of included
studies. |
Table III
Characteristics of included
studies.
| Study/year
(ref.) | Country | Reference
standard | Cross-sectional
design | Consecutive and/or
random? | Blinded design | Prospective |
|---|
| Shimokata/1988
(13) | Japan | Histology | Yes | Yes | Yes | Yes |
| Lotzniker/1991
(14) | Italy | Histology | Unknown | Unknown | Unknown | Unknown |
| Romero/1996
(15) | Spain | Histology | Unknown | Yes | Yes | Yes |
| Villena/1996
(16) | Spain | Histology | Unknown | Yes | Yes | Yes |
| Miédougé/1999
(17) | France | Histology | Yes | Yes | No | No |
| Zimmerman/2000
(18) | USA | Histology | Yes | Yes | Unknown | Yes |
| Alataş/2001
(19) | Turkey | Histology | No | Yes | Yes | Yes |
| Villena/2003
(20) | Spain | Histology | Unknown | Yes | Yes | Yes |
| Porcel/2004
(21) | Iran | Histology | Yes | Yes | Yes | Yes |
| Ustün/2004
(22) | Turkey | Histology | Unknown | No | Unknown | Yes |
| Ghayumi/2005
(23) | Iran | Histology | Yes | Yes | Yes | Yes |
| Shitrit/2005
(24) | Israel | Histology | Yes | Yes | Yes | Yes |
| Topolcan/2007
(25) | Czech | Histology | Yes | Yes | Yes | Yes |
| Paşaoğlu/2007
(26) | Turkey | Histology | Yes | Yes | Unknown | Yes |
| Wagner/2007
(27) | Brazil | Histology | Yes | Yes | Yes | Yes |
| Li/2007 (28) | China | Histology | Yes | Unknown | Yes | Yes |
| Gaspar/2008
(29) | Spain | Histology | Yes | Yes | Unknown | Yes |
| Creaney/2008
(30) | Australia | Histology | Yes | Yes | Yes | Yes |
| Terracciano/2010
(31) | Italy | Histology | Yes | Unknown | Yes | Yes |
| Antonangelo/2010
(32) | Brazil | Histology | Yes | Yes | Unknown | Yes |
| Farag/2012
(33) | Egypt | Histology | Yes | Unknown | No | Yes |
Diagnostic accuracy
The forest plots of sensitivity and specificity of
CA 15-3 assays in the various studies for the diagnosis of MPE are
shown in Fig. 2. The sensitivity
varied between 0.30 and 0.96 [pooled 0.58, 95% confidence interval
(CI), 0.560–0.61], while the specificity ranged from 0.35 to 1.00
(pooled 0.91, 95% CI, 0.90–0.93). The PLR was 8.93 (95% CI,
4.45–17.93), the NLR was 0.46 (95% CI, 0.37–0.56) and the DOR was
24.89 (95% CI, 10.39–56.63). χ2 values of sensitivity,
specificity, PLR, NLR and DOR were 314.02, 312.53, 201.71, 214.78
and 163.24, respectively, with all P-values <0.001, indicating
significant heterogeneity between all studies.
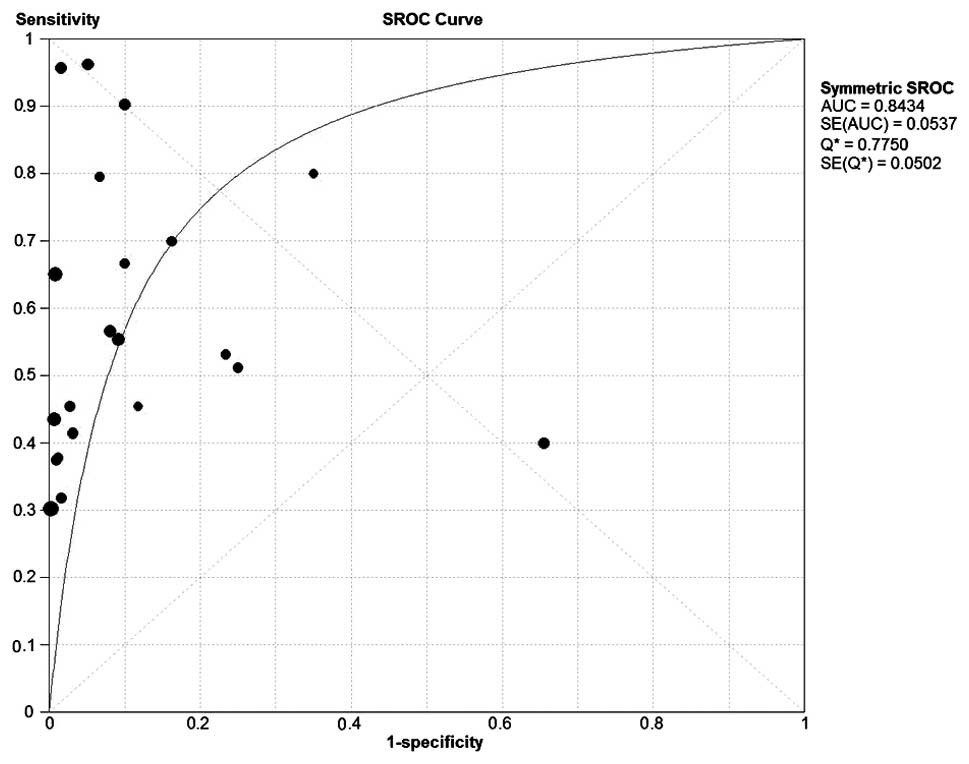
The Fig. 3 shows
the SROC curve, which summarizes the test performance, and shows
the balance between sensitivity and specificity. The Q-value is a
global measure of test efficacy. It is the point of intersection of
the SROC curve with a diagonal line from the left upper corner to
the right lower corner of the ROC space, and corresponds to the
highest common value of sensitivity and specificity for the test.
This point does not indicate the only or even the best combination
of sensitivity and specificity for a particular clinical setting,
but represents an overall measure of the discriminatory power of a
test. In present meta-analysis, the maximum joint sensitivity and
specificity (the Q-value) was 0.77. The area under the curve (AUC)
was 0.84.
When evaluating the publication bias, Deeks’ test
was performed and it was significant (P=0.01). The funnel plot for
publication bias (Fig. 4) is also
essentially asymmetric. Thus, the results suggest a potential for
publication bias.
Discussion
MPE is one of the most common pleura-associated
problems encountered in clinical practice. The diagnosis of
malignancy in pleural effusions continues to be challenging
(4). Finding an effectively
diagnostic tool for MPE is of great importance. The detection of
tumor markers such as CA 15-3 in the pleural fluid has been
proposed as an alternative non-invasive method for the diagnosis of
MPE (11).
The present meta-analysis investigated the overall
diagnostic value of CA 15-3 measurements in pleural effusions in
the diagnosis of MPE. The specificity was 0.91 (95% CI, 0.91–0.93),
indicating a potential role for CA 15-3 analysis in the
confirmation of MPE. In contrast with the high specificity, the
sensitivity was only 0.58 (95% CI, 0.56–0.61), which is
insufficient to exclude MPE. Thus, negative tests do not clearly
indicate the absence of MPE, and patients with negative CA 15-3
results have a fairly high chance of having MPE. This trade-off has
significant clinical implications.
To summarize the test performance, an SROC curve was
generated, which indicates the balance between sensitivity and
specificity (46). The SROC curve
for the present meta-analysis revealed that the maximum joint
sensitivity and specificity (Q value) was 0.77 and the AUC was
0.84, indicating that the overall accuracy was not very high.
The DOR, which is the ratio of the odds of a
positive test result in the diseased relative to that in the
non-diseased state, is an alternative indicator of test accuracy.
The higher the DOR value, the more discriminatory the test
(47). In the present
meta-analysis, the mean DOR was found to be 24.89 (95% CI,
10.39–59.63), suggesting that CA 15-3 testing is a useful tool for
aiding the diagnosis of MPE.
The PLR and NLR were also determined as measures of
diagnostic accuracy in the present study, as likelihood ratios are
considered to be more clinically meaningful than the DOR (48,49).
A PLR value of 8.93 in the present study suggested that patients
with MPE have an ~9-fold higher chance of testing positive in the
CA 15-3 assay than patients without MPE, which should be helpful
for in clinical practice. However, the NLR value of 0.46 determined
in the present study meant that if the CA 15-3 assay result was
negative, the probability that a patient was affected by MPE was
~46%, which is too high to rule out MPE.
In present study, QUADAS scores were used in the
meta-regression to assess the effect of study quality on RDOR. As
shown in Table I, the studies with
higher quality (QUADAS ≥10) produced lower RDORs than those with
lower quality. The meta-regression also indicated that differences
between CA 15-3 assay methods (EIA versus non-EIA), studies with or
without blinded design, cross-sectional, consecutive/random and
prospective design, did not reach statistical significance. Thus,
these factors do not affect diagnostic accuracy.
Notably, the results of the present study were
consistent with those of a previous meta-analysis conducted by
Liang et al (50). This
earlier meta-analysis included 11 related studies prior to 2005.
Since that time, additional studies on this field have been
reported and are included in the present study. The search strategy
and data extraction methods used in the present meta-analysis were
more comprehensive than those in the previous meta-analysis, which
was an important strength. Literature selection, quality assessment
and data extraction were performed independently and in a blinded
fashion by five reviewers. By meta-regression, the current study
assessed the effects of covariates such as CA 15-3 assay methods on
the RDOR, which was not performed in the previous meta-analysis
(50). However, the present study
had certain limitations. Firstly, studies published in languages
other than English, unpublished studies and abstracts from
conference proceedings were not included, which was probably a
cause of publication bias. Secondly, issues such as the exact
condition of the patients and laboratory infrastructure were not
analyzed due to limited data.
The present meta-analysis suggested that the
diagnostic value of CA 15-3 for MPE was far from perfection.
Combining CA 15-3 with other markers may be an appropriate method
for improving the diagnostic accuracy. The study by Romero et
al found that the sensitivity and specificity of
carcinoembryonic antigen combined with CA 15-3 in pleural fluid
were 71% and 96%, respectively, which was better than testing CA
15-3 alone (15). Another study
reported that the combination of thymidine kinase with CA 15-3 and
procalcitonin appeared to be an optimal combination, nearly
enabling differential diagnosing in all types of effusion (25).
In conclusion, with significantly high specificity
in the detection of MPE, pleural CA 15-3 analysis is likely to be a
effective assay to ascertain the potential existence of MPE in
patients, particularly those who present clinical manifestation of
MPE but with negative cytological findings of the pleural fluid,
and thus provide the benefit of further invasive pathologic
examination when elevated CA 15-3 levels are found in pleural
effusions. However, ruling out MPE by testing CA15-3 alone is not
recommended due to its limited sensitivity, and the results of
CA15-3 assays should be interpreted in parallel with conventional
test results and other clinical findings.
Acknowledgements
This study was supported by a grant from the
National Basic Research Program of China (no. 2011CB935800).
References
|
1
|
American Thoracic Society. Management of
malignant pleural effusions. Am J Respir Crit Care Med.
162:1987–2001. 2001.
|
|
2
|
Heffner JE: Management of the patient with
a malignant pleural effusion. Semin Respir Crit Care Med.
31:723–733. 2010. View Article : Google Scholar
|
|
3
|
Light RW: Pleural effusion related to
metastatic malignancies. Pleural Diseases. 4th edition. Lippincott;
Philadelphia: pp. 133–161. 2001
|
|
4
|
Bennett R and Maskell N: Management of
malignant pleural effusions. Curr Opin Pulm Med. 11:296–300.
2005.PubMed/NCBI
|
|
5
|
Prakash UB and Reiman HM: Comparison of
needle biopsy with cytologic analysis for the evaluation of pleural
effusion: analysis of 414 cases. Mayo Clin Proc. 60:158–164. 1985.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nance KV, Shermer RW and Askin FB:
Diagnostic efficacy of pleural biopsy as compared with that of
pleural fluid examination. Mod Pathol. 4:320–324. 1991.PubMed/NCBI
|
|
7
|
Lombardi G, Zustovich F, Nicoletto MO,
Donach M, Artioli G and Pastorelli D: Diagnosis and treatment of
malignant pleural effusion: a systematic literature review and new
approaches. Am J Clin Oncol. 33:420–423. 2010. View Article : Google Scholar
|
|
8
|
Novaković S: Tumor markers in clinical
oncology. Radiol Oncol. 38:73–83. 2004.
|
|
9
|
Fenton KN and Richardson JD: Diagnosis and
management of malignant pleural effusions. Am J Surg. 170:69–74.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Porcel JM, Vives M, Esquerda A, Salud A,
Pérez B and Rodríguez-Panadero F: Use of a panel of tumor markers
(carcinoembryonic antigen, cancer antigen 125, carbohydrate antigen
15-3, and cytokeratin 19 fragments) in pleural fluid for the
differential diagnosis of benign and malignant effusions. Chest.
126:1757–1763. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Light RW: Tumor markers in undiagnosed
pleural effusions. Chest. 126:1721–1722. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Buccheri G and Ferrigno D: Lung tumor
markers of cytokeratin origin: an overview. Lung Cancer. 34(Suppl
2): S65–S69. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Shimokata K, Totani Y, Nakanishi K, et al:
Diagnostic value of cancer antigen 15-3(CA 15-3) detected by
monoclonal antibodies (115D8 and DF3) in exudative pleural
effusions. Eur Respir J. 1:341–344. 1988.PubMed/NCBI
|
|
14
|
Lotzniker M, Pavesi F, Scarabelli M,
Vadacca G, Franchi M and Moratti R: Tumour associated antigens CA
15-3 and CA 125 in ovarian cancer. Int J Bid Markers. 6:115–121.
1991.
|
|
15
|
Romero S, Fernandez C and Arriero JM: CEA,
CA15-3 and CYFRA21-1 in serum and pleural fluid of patients with
pleural effusions. Eur Respir J. 9:17–23. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Villena V, López-Encuentra A,
Echave-Sustaeta J, Martín-Escribano P, Ortuño-de-Solo B and
Estenoz-Alfaro J: Diagnostic value of CA 72-4, carcinoembrynic
antigen, CA 15-3 and CA 19-9 assay in pleural fluid: A study of 207
patients. Cancer. 78:736–740. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Miédougé M, Rouzand P, Salama G, et al:
Evaluation of seven tumor markers in pleural fluid for the
diagnosis of malignant effusions. Br J Cancer. 81:1059–1065. 1999.
View Article : Google Scholar
|
|
18
|
Zimmerman RL, Fogt F and Goonewardene S:
Diagnostic value of a second generation CA 15-3 antibody to detect
adenocarcinoma in body cavity effusions. Cancer Cytopathol.
90:230–234. 2000. View Article : Google Scholar
|
|
19
|
Alataş F, Alataş O, Metintaş M, Colak O,
Harmanci E and Demir S: Diagnostic value of CEA, CA 15-3, CA 19-9,
CYFRA 21-1, NSE and TSA assay in pleural effusions. Lung Cancer.
31:9–16. 2001. View Article : Google Scholar
|
|
20
|
Villena V, López-Encuentra A,
Echave-Sustaeta J, Martín-Escribano P, Ortuño-de-Solo B and
Estenoz-Alfaro J: Diagnostic value of CA 549 in pleural fluid,
Comparison with CEA, CA 15-3 and CA 72-4. Lung Cancer. 40:289–294.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Porcel JM, Vives M, Esquerda A, Salud A,
Pérez B and Rodríguez-Panadero F: Use of a panel of tumor markers
(carcinoembryonic antigen, cancer antigen 125, carbohy-drate
antigen 15-3 and cytokeratin 19 fragments) in pleural fluid for the
differential diagnosis of benign and malignant effusions. Chest.
126:1757–1763. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ustün H, Borazan A, Bilgiçli N and Yilmaz
A: Diagnostic value of tumoural markers in pleural effusions. Int J
Clin Pract. 58:22–25. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ghayumi SM, Mehrabi S, Doroudchi M and
Ghaderi A: Diagnostic value of tumor markers for differentiating
malignant and benign pleural effusions of Iranian patients. Pathol
Oncol Res. 11:236–241. 2005. View Article : Google Scholar
|
|
24
|
Shitrit D, Zingerman B, Shitrit AB, Shlomi
D and Kramer MR: Diagnostic value of CYFRA21-1, CEA, CA 19-9, CA
15-3 and CA 125 assays in pleural effusions: analysis of 116 case
and review of the literature. Oncologist. 10:501–507. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Topolcan O, Holubec L, Polivkova V, et al:
Tumor markers in pleural effusions. Anticancer Res. 27:1921–1924.
2007.PubMed/NCBI
|
|
26
|
Paşaoğlu G, Zamani A, Can G and İmecik O:
Diagnostic value of CEA, CA 19-9, CA 125 and CA 15-3 levels in
malignant pleural fluids. Eur J Gen Med. 4:165–171. 2007.
|
|
27
|
Wagner IC, Guimarães MJ, da Silva LK, de
Melo FM and Muniz MT: Evaluation of serum and pleural levels of the
tumor markers CEA, CYFRA21-1 and CA 15-3 in patients with pleural
effusion. J Bras Pneumol. 33:185–191. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Li CS, Cheng BC, Ge W and Gao JF: Clinical
value of CYFRA21-1, NSE, CA15-3, CA19-9 and CA125 assay in the
elderly patients with pleural effusions. Int J Clin Pract.
61:444–448. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Gaspar MJ, De Miguel J, García Díaz JD and
Díez M: Clinical utility of a combination of tumor markers in the
diagnosis of malignant pleural effusions. Anticancer Res.
28:2947–2952. 2008.PubMed/NCBI
|
|
30
|
Creaney J, Segal A, Sterrett G, et al:
Overexpression and altered glycosylation of MUC1 in malignant
mesothelioma. Br J Cancer. 98:1562–1569. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Terracciano D, Mazzarelia C, Cicalese M,
et al: Diagnostic value of carbohydrate antigens in supernatants
and sediments of pleural effusions. Oncol Lett. 1:465–471.
2010.PubMed/NCBI
|
|
32
|
Antonangelo L, Cora AP and Sales MP:
Evaluation of pleural fluid levels and Pleural-Serum Ratio of the
tumor markers CEA, CA 15-3, CA 19-9, CA 72-4, CA 125 and CYFRA 21-1
in the diagnosis of malignant pleural effusion. Braz J Biol.
15:146–152. 2010.
|
|
33
|
Farag DH, El Hadidi E, El Maraghy MO and
Hussein MM: Pleural cyfra 21-1 and CA 15-3 in differentiation of
malignant from benign pleural effusions. Life Sci J. 9:499–505.
2012.
|
|
34
|
Whiting P, Rutjes AW, Reitsma JB, Bossuyt
PM and Kleijnen J: The development of QUADAS: a tool for the
quality assessment of studies of diagnostic accuracy included in
systematic reviews. BMC Med Res Methodol. 3:252003. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Jones CM, Ashrafian H, Skapinakis P, et
al: Diagnostic accuracy meta-analysis: a review of the basic
principles of interpretation and application. Int J Cardiol.
140:138–144. 2010. View Article : Google Scholar
|
|
36
|
Moses LE, Shapiro D and Littenberg B:
Combining independent studies of a diagnostic test into a summary
ROC curve: data-analytic approaches and some additional
considerations. Stat Med. 12:1293–1316. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Lau J, Ioannidis JP, Balk EM, et al:
Diagnosing acute cardiac ischemia in the emergency department: a
systematic review of the accuracy and clinical effect of current
technologies. Ann Emerg Med. 37:453–460. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Irwig L, Tosteson AN, Gatsonis C, et al:
Guidelines for meta-analyses evaluating diagnostic tests. Ann
Intern Med. 120:667–676. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Vamvakas EC: Meta-analyses of studies of
the diagnostic accuracy of laboratory tests: a review of the
concepts and methods. Arch Pathol Lab Med. 122:675–686.
1998.PubMed/NCBI
|
|
40
|
Suzuki S, Moro-oka T and Choudhry NK: The
conditional relative odds ratio provided less biased results for
comparing diagnostic test accuracy in meta-analyses. J Clin
Epidemiol. 57:461–469. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Westwood ME, Whiting PF and Kleijnen J:
How does study quality affect the results of a diagnostic
meta-analysis? BMC Med Res Methodol. 5:202005. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Deeks JJ, Dinnes J, D’Amico R, et al:
Evaluating non-randomised intervention studies. Health Technol
Assess. 7:1–173. 2003.
|
|
43
|
Bielsa S, Esquerda A, Salud A, et al: High
levels of tumor markers in pleural fluid correlate with poor
survival in patients with adenocarcinomatous or squamous malignant
effusions. Eur J Intern Med. 20:383–386. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Tampellini M, Berruti A, Gorzegno G, et
al: Independent factors predict supranormal CA 15-3 serum levels in
advanced breast cancer patients at first disease relapse. Tumor
Biol. 22:367–373. 2001. View Article : Google Scholar
|
|
45
|
Cascinu S, Del Ferro E, Barbanti I, Ligi
M, Fedeli A and Catalano G: Tumor markers in the diagnosis of
malignant serous effusions. Am J Clin Oncol. 20:247–250. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Moses LE, Shapiro D and Littenberg B:
Combining independent studies of a diagnostic test into a summary
ROC curve: data-analytic approaches and some additional
considerations. Stat Med. 12:1293–1316. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Glas AS, Lijmer JG, Prins MH, Bonsel GJ
and Bossuyt PM: The diagnostic odds ratio: a single indicator of
test performance. J Clin Epidemiol. 56:1129–1135. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Deeks JJ: Systematic reviews of
evaluations of diagnostic and screening tests. Systematic Reviews
in Health Care: Meta-analysis in Context. Egger M, Smith GD and
Altman DG: 2nd edition. BMJ Publishing Group; London, UK: pp.
248–282. 2001, View Article : Google Scholar
|
|
49
|
Jaeschke R, Guyatt G and Lijmer J:
Diagnostic tests. Users’ Guides to the Medical Literature: A Manual
for Evidence-based Clinical Practice. Guyatt G and Rennie D: AMA
Press; Chicago, IL: pp. 121–140. 2002
|
|
50
|
Liang QL, Shi HZ, Qin XJ, Liang XD, Jiang
J and Yang HB: Diagnostic accuracy of tumor markers for malignant
pleural effusion: a meta-analysis. Thorax. 63:35–41. 2008.
View Article : Google Scholar
|