Introduction
Kidney diseases predominantly manifest as renal
dysfunction, with the main pathological changes of
glomerulosclerosis and renal interstitial fibrosis (1). Numerous studies have found that
abnormal lipid metabolism exists commonly in the late stages of
chronic kidney diseases; this is characterized by high triglyceride
(TG) and low high-density lipoprotein (HDL) cholesterol levels,
leading to hyperlipidemia or hyperlipoproteinemia (2–4). The
resulting disease state, which is easily complicated by
atherosclerosis (AS), accounts for the high morbidity and mortality
of chronic kidney diseases complicated by cardiovascular diseases
(5). Elucidation of the
distribution of lipid components in the aorta and blood in early
chronic renal failure (CRF) and the sequence of aortic lipid
deposition may help to clarify the association between lipid
metabolism and the occurrence and development of cardiovascular
diseases in early CRF at the molecular level. In the present study,
the aortic arches of male Sprague Dawley (SD) rats undergoing 5/6
nephrectomy under sterile conditions were sampled on the 10th, 30th
and 60th days to determine the dynamic levels of triglyceride (TG),
total cholesterol (T-Ch) and total phospholipid (T-PL) for
comparison with the levels in the control group at the same
time-point. In addition, the TG, T-Ch and T-PL levels in the plasma
and T-Ch and T-PL levels in erythrocyte membranes were observed
dynamically on the 10th, 30th and 60th days after the
nephrectomies.
Glomerulosclerosis and renal interstitial fibrosis
are closely associated with the increased expression of
transforming growth factor-β1 (TGF-β1) in innate renal and
infiltrated inflammatory cells (6–9); as
such, immunotherapy and genetic therapy specific to TGF-βl are
currently attracting considerable attention. Decorin (DCN), as a
natural antagonist of TGF-β1, can neutralize the biological effects
of TGF-β1. The aim of this study was to explore a novel genetic
therapy for renal insufficiency, based on the hypothesis that the
renal transplantation of DCN-expressing fibroblasts (FBs)
transfected with DCN [FB (LDCNSN) cells] (10,11)
could be used to neutralize the increased TGF-βl activity in the
kidneys of renal failure rats.
Materials and methods
Ethical approval
All animal experiments received approval from the
Animal Ethics Committees of the Shandong Provincial Hospital and
Shandong University Postgraduate College (Shandong, China) and were
performed strictly in accordance with the National Institutes of
Health Guide for the Care and Use of Laboratory Animals.
Grouping
A total of 76 rats (56 male and 20 female) purchased
from the Laboratory Animal Center of Shandong University (Shandong,
China) and weighing 150–200 g underwent a two-step 5/6 nephrectomy
under sterile conditions. Six rats in the sham surgery group (Group
A) received the same surgical procedures, but their kidneys were
retained. The rats were allowed to drink water and eat freely
following surgery. Once the 5/6 nephrectomy rat models with renal
failure had been established, the model rats were further randomly
divided into three groups: i) Group B/surgery control group, no
treatment (n=10); ii) Group C/blank control group, treatment with
FBs transfected with empty vector [FB (LXSN) cells] (n=10); and
iii) Group D/treatment group, treatment with FB (LDCNSN) cells
(n=10) (12).
Dynamic lipid levels in the plasma and
erythrocyte membrane
Four time-points, the 10th, 20th, 40th and 60th
days, were selected for the dynamic observation of lipid levels in
the plasma and erythrocyte membrane, and three-time points, the
10th, 30th and 60th days, were selected for the lipid levels in the
aortic arches. Eight and 12 rats, with equal number of males and
females, were selected for the experimental and control groups,
respectively, at each time-point. The experimental and control
groups underwent the first and second surgeries simultaneously. For
the experimental group, two-thirds of the left kidney was resected
in the first procedure and the whole right kidney was resected in
the second procedure 10 days later. The control group only
underwent the surgical incision. Identical test conditions were
maintained in the two groups. Two hours after the 12 rats in the
control group revived from the anesthesia of the second surgery,
blood was sampled from the heart to measure the levels of T-Ch and
TG of the plasma and the level of T-PL in the erythrocyte membrane,
and the aortic arches were separated as the day 0 control samples.
The heart blood of the experimental and control groups was
additionally collected following the second surgery to prepare the
plasma and erythrocyte membrane, and the aortic arches and kidney
(two rats for pathological monitoring) were obtained at different
time-points. A total of 10 rats were left in the experimental group
at each time-point due to the possibility of death during the
experiment and the failure of the surgery and for
pathomorphological observation during the formation of CRF
(13).
Determination of lipid levels in the
aortic arches
Tissues, such as the fat on the surface of the
vascular outer wall, were removed from the separated aortic arches
and any blood was blotted using filter paper. The samples were then
cut into 5- to 6-mm pieces and weighed with a One Over 10,000
Analytical Balance (Mettler-Toledo, Shanghai, China). The average
weight of the experimental group samples was 261.106±15 mg and that
of the control group was 260.156±16 mg. Each sample was then placed
into the homogenizer and ground for 10 min. Lipids were extracted
by the Rose-Gottlieb extraction (14,15)
method and dried with nitrogen. T-Ch and TG levels were measured
with the same method utilized to measure the levels in the plasma.
The T-PL level was determined using the coefficient between
inorganic phosphorus and T-PL. The level of inorganic phosphorous
was measured using the molybdenum blue colorimetric method
following acid digestion. Acid digestion was performed by adding
140 ml concentrated sulfuric acid to 250 ml distilled water,
agitating the mixture, and then adding 32.5 ml 70% perchloric acid
and distilled water to make a total volume of 500 ml. This mixture
was then further agitated. The results are expressed in μmol per
gram of aortic tissue (16).
Determination of plasma lipids
Measurements of TG, T-Ch and T-PL levels were made
using the glycerol-3-phosphate oxidase-phenol-aminophenazone (PAP),
cholesterol oxidase-PAP and ammonium molybdate reduction methods,
respectively. Measurements of urea and creatinine (Cr) were made
using the PAP rate method. Five samples were added to each batch of
samples as the intra- and inter-assay quality controls (17). The relevant kits were purchased
from Beijing Zhongshan Golden Bridge Biotechnology Co., Ltd.
(Beijing, China). The procedures were performed strictly in
accordance with the manufacturer’s instructions.
Determination of lipid levels in the
erythrocyte membrane
T-Ch and T-PL were extracted from the erythrocyte
membrane by the Rose-Gottlieb method, and measured by the plasma
method. The results are expressed in mmol/l hematocrit. Hematoxylin
and eosin (HE) staining was used for renal pathological monitoring
and observed using a light microscope. The instruments used
included a Monarch22000 automatic biochemical analyzer (Arris, IL
company, USA) and a Beckman-700 biochemical analyzer (Beckman
Coulter, Miami, FL, USA).
FB (LDCNSN) and FB (LXSN) cells were cultured in
Dulbecco’s modified Eagle’s medium containing 300 ng/ml G418 and
10% fetal calf serum. The cells were then digested and collected
using EDTA-trypsin, and washed three times with high-pressure
sterilized normal saline. The cell concentration was adjusted to
1×107/ml. The FB (LXSN) and FB (LDCNSN) cells were
administered to the renal medulla in the control and treatment
groups, respectively, via multi-point injection during the 5/6
nephrectomy. The injection points were distributed uniformly across
five to six sites, with 1×106 cells/kidney in total. The
rats had free access to water and food following surgery.
Sample collection and renal function
indices
Prior to treatment and in the first and fourth weeks
after treatment, the body weights (BW) of the rats in each group
were measured, femoral arterial blood was taken and serum TG, T-Ch,
Cr and urea nitrogen (BUN) levels were detected using an automatic
biochemical analyzer. The renal tissue samples were fixed in 10%
formalin solution and liquid nitrogen respectively.
Immunohistochemical examination
The renal tissues were embedded in paraffin, and
sliced into 3- to 4-μm sections. Following conventional
deparaffinization, the slices that underwent HE, Periodic Acid
Schiff and Masson staining were observed under light microscopy.
The tubulointerstitial lesions were then subjected to
semi-quantitative grading, as follows: 0, normal; I, lesion scope
≤25%; II, lesion scope 26–50%; and III, lesion scope >50%.
The EnVision™ immunohistochemistry system (Beijing
Zhongshan Golden Bridge Biotechnology Co., Ltd.) was used to detect
the changes in DCN and TGF-β1 expression in the renal tissues.
Following conventional deparaffinization, microwave-induced antigen
retrieval was performed for 10 min and a drop of 3%
H2O2 was added to each slice. Incubation was
then carried out for 20 min at room temperature. The primary
antibody, rabbit anti-rat monoclonal anti-TGFβ1 (cat. no. RS-0105R;
Beijing Zhongshan Golden Bridge Biotechnology Co., Ltd.), was added
at a 1:200 dilution followed by rabbit anti-rat monoclonal anti-DCN
(cat. no RS-0017R; Beijing Zhongshan Golden Bridge Biotechnology
Co., Ltd.) at a 1:200 dilution, prior to incubation for 2 h at room
temperature. Following incubation, the slice was rinsed with
phosphate-buffered saline (PBS) three times for 5 min, avidin was
added and the slice was further incubated for 20 min at room
temperature. The slice was then rinsed again with PBS three times
for 3 min, and horseradish peroxidase-labeled goat anti-rabbit
secondary antibody (cat. no PV-0202R; Beijing Zhongshan Golden
Bridge Biotechnology Co., Ltd.) was added prior to incubation for
30 min at room temperature. Following incubation, the slice was
rinsed with PBS three times for 5 min, 3,3′-diaminobenzidine was
added and the slice was examined under a light microscope for 5
min. The slices were restained with hematoxylin and 0.1%
hydrochloric acid and washed with water, following which they
turned blue. They were subsequently dehydrated in gradient ethanol,
vitricated by dimethylbenzene, mounted with neutral balsam
(mounting medium) and examined subsequent to air drying. The
results from the immunohistochemistry of TGF-βl and DCN were
subjected to semi-quantitative analysis performed by three
personnels simultaneously. The distribution of staining in the
tubulointerstitial area was graded into levels, as follows: 0, no
staining; 1, occasional staining; 2, focal staining; and 3, diffuse
staining.
Statistical analysis
All statistical analysis was performed by using SPSS
17.0 software (SPSS, Chicago, IL, USA). The Student’s t-test was
applied for intergroup comparisons and linear correlation analysis.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Dynamic changes in early-stage aortic
lipid deposition
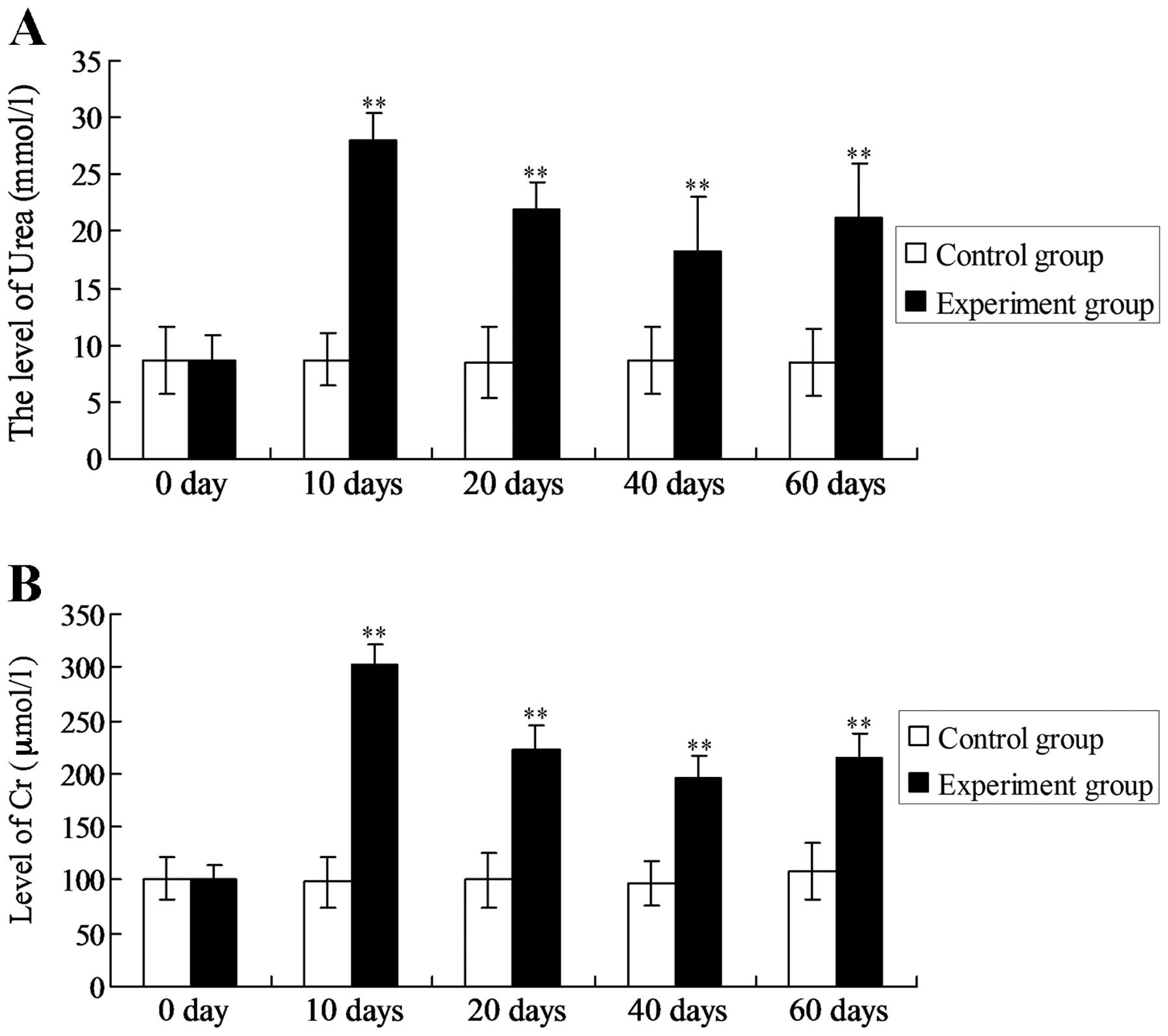
The concentrations of urea and Cr peaked on the 10th
day (27.93±2.46 mmol/l and 308.50±19.65 μmol/l, respectively). The
concentrations began to decline on the 20th day and were minimal on
the 40th day (18.30±4.14 mmol/l and 193.45±22.32 μmol/l,
respectively); however, at both time-points the concentrations were
significantly increased compared with those in the control group
(8.67±3.00 mmol/l and 96.47±21.33 μmol/l, respectively)
(P<0.01). The urea and Cr concentrations started to increase
again on the 60th day (Fig.
1).
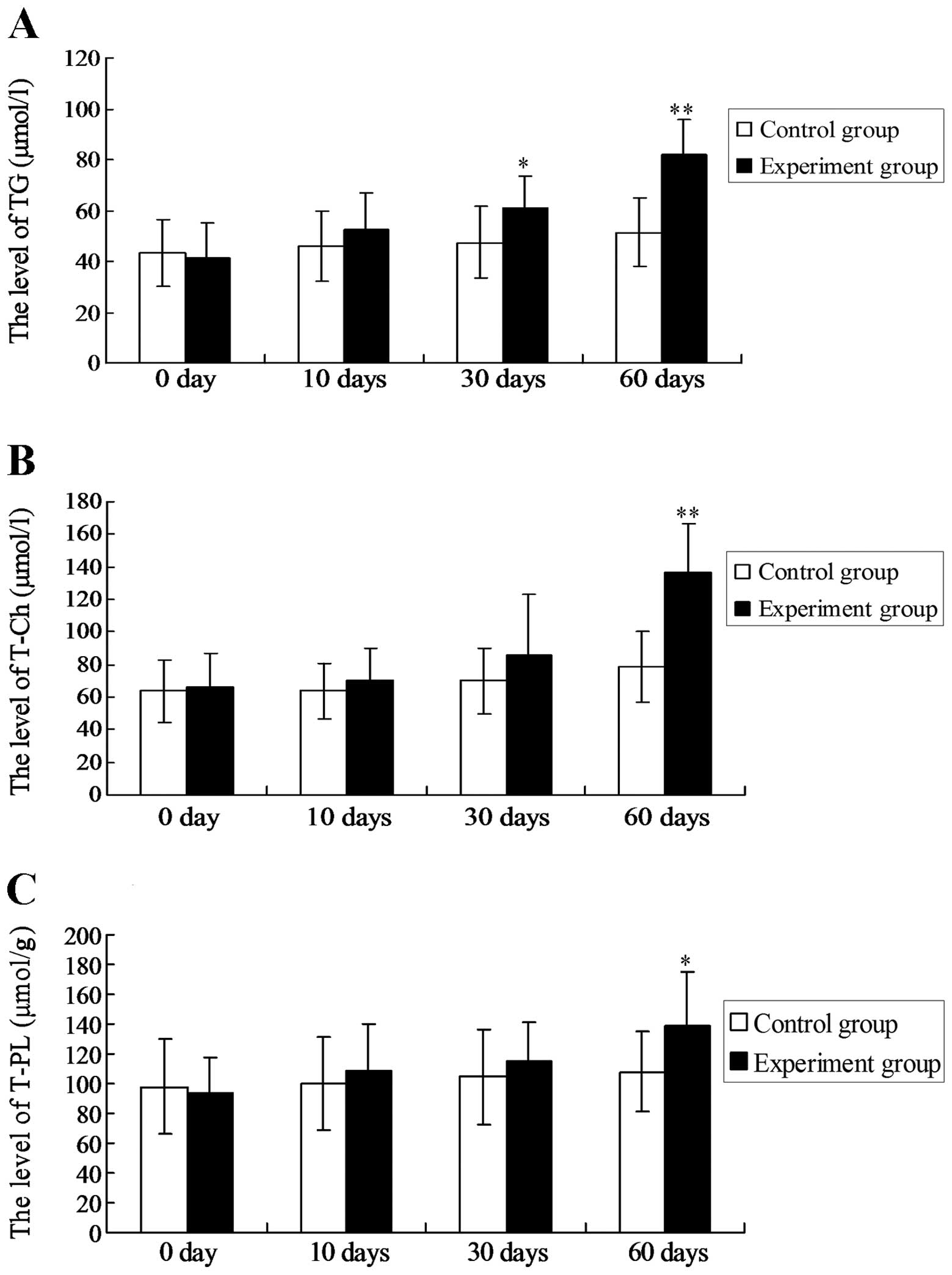
The levels of the three lipids started to increase
on the 10th day and presented a rising trend thereafter. The TG
level was increased significantly compared with that of the control
group at the same time-point on the 30th day (P<0.05) and on the
60th day (P<0.01). The T-Ch and T-PL levels started to increase
on the 10th day and were significantly higher than those of the
control group on the 60th day (P<0.01 and P<0.05,
respectively).
The TG and T-Ch levels in the plasma of the
experimental group rats started to increase from the 10th day and
continuously rose; the levels were significantly higher than those
of the control group on the 10th, 30th, 40th and 60th days
(P<0.05; Table I). The T-PL
levels increased significantly on the 10th day, then decreased on
the 20th and 30th days, and slightly increased again on the 60th
day. The T-Ch level in the erythrocyte membranes began to increase
on the 10th day and was significantly higher compared to that of
the control group on the 40th and 60th days (P<0.05). The T-PL
level in the erythrocyte membranes was slightly lower than that of
the control group on the 20th (P<0.05), and significantly
decreased on the 40th and 60th days (P<0.01). The results are
shown in Table II. The TG and
T-Ch levels in the plasma were significantly positively correlated
with those in aortic tissue (r=0.99 and r=0.97), while the T-PL
level in the plasma was significantly negatively correlated with
that in aortic tissue (r=−0.92).
 | Table IDynamic changes in plasma TG, T-Ch and
T-PL levels. |
Table I
Dynamic changes in plasma TG, T-Ch and
T-PL levels.
| | Day |
|---|
| |
|
|---|
| Item | Group | 0 | 10 | 20 | 30 | 60 |
|---|
| TG | Control | 8.58±2.94 | 8.73±2.36 | 8.42±3.13 | 8.67±3.00 | 8.44±2.94 |
| Experimental | 8.19±1.89 | 27.93±2.46a | 22.01±2.33a | 18.3±4.64a | 21.1±4.82a |
| T-Ch | Control | 23.14±1.49 | 25.31±3.29 | 25.93±1.59 | 24.58±3.46 | 27.81±5.14 |
| Experimental | 24.53±2.34 | 35.41±3.26a | 39.42±1.69a | 43.25±4.16a | 51.28±5.65b |
| T-PL | Control | 101.53±7.89 | 98.33±24.31 | 99.90±26.13 | 96.46±21.32 | 108.46±26.45 |
| Experimental | 112.24±4.57 | 301.83±19.63b | 223.19±21.84b | 195.46±22.29b | 214.32±23.36b |
 | Table IIDynamic changes in T-CH and T-PL
levels in erythrocyte membranes. |
Table II
Dynamic changes in T-CH and T-PL
levels in erythrocyte membranes.
| | Day |
|---|
| |
|
|---|
| Item | Group | 0 | 10 | 20 | 40 | 60 |
|---|
| T-Ch | Control | 3.59±0.36 | 3.62±0.25 | 3.57±0.32 | 3.58±0.34 | 3.61±0.33 |
| Experimental | 3.58±0.41 | 3.63±0.37 | 3.82±0.38a | 4.25±0.36b | 4.64±0.39b |
| T-PL | Control | 2.58±0.32 | 2.57±0.34 | 2.59±0.31 | 2.58±0.33 | 2.60±0.35 |
| Experimental | 2.61±0.36 | 2.55±0.32 | 2.40±0.29a | 1.92±0.26b | 1.53±0.22b |
Effects of gene therapy on CRF rats
No significant differences were observed in the BWs
of rats among the groups prior to the experiment. In the fourth
week, the weights of rats in all the groups increased to different
degrees, but the differences among the groups were not
statistically significant (data not shown).
The blood lipid levels in the rats were
significantly increased after four weeks compared with those at
week 0 (Table III), and the BUN
and serum Cr levels in Group D were significantly lower than those
in Group C on the 4th week (P<0.05). Although a slight increase
was observed in group D compared with group A for the values in
week 0, the difference was not statistically significant (Table IV).
 | Table IIIBlood lipid levels at different
time-points. |
Table III
Blood lipid levels at different
time-points.
| Item | Time-point | Group A | Group B | Group C | Group D |
|---|
| T-Ch | Week 0 | 0.76±0.31 | 0.75±0.53 | 0.78±0.27 | 0.78±0.56 |
| Week 1 | 0.96±0.43 | 1.63±0.45 | 1.16±0.43 | 0.87±0.27 |
| Week 4 | 1.18±0.24a | 1.09±0.12a | 1.46±0.08a | 1.09±0.44a |
| TG | Week 0 | 1.36±0.27 | 1.60±0.31 | 1.70±0.26 | 1.45±0.27 |
| Week 1 | 1.39±0.24 | 1.96±0.54 | 2.15±0.51 | 2.33±0.06 |
| Week 4 | 1.84±0.09a | 1.81±0.34b | 1.98±0.24b | 1.83±0.13b |
 | Table IVRenal functions at different time
intervals. |
Table IV
Renal functions at different time
intervals.
| Item | Time-point | Group A | Group B | Group C | Group D |
|---|
| BUN | Week 0 | 7.2±1.0 | 7.5±1.4 | 8.7±1.4 | 11.8±6.8 |
| Week 1 | 7.2±1.5 | 11.5±1.0 | 21.9±1.2 | 26.9±3.6 |
| Week 4 | 7.4±1.6 | 22.0±0.4a | 27.9±7.8a | 16.4±2.8a |
| Scr | Week 0 | 42.3±5.9 | 50.2±8.1 | 61.5±7.8 | 64.7±6.9 |
| Week 1 | 49.1±4.8 | 76.2±4.4 | 108.9±5.6 | 91.9±18.6 |
| Week 4 | 47.9±10.2 | 99.6±10.7a | 110.6±21.1a | 68.3±5.5b |
TGF-βl expression was predominantly found in the
fibrotic renal interstitium, renal tubular epithelial cells and
glomerulus. DCN was mainly distributed in interstitial fibrotic
sites, the sclerotic glomerulus and vascular adventitia. Four weeks
after the treatment with FB (LDCNSN) cells, the DCN expression in
the renal tissues was increased significantly. The expression of
TGF-β1 in Group D was not significantly different from that in
Groups B and C (Table V).
 | Table VExpression of DCN and TGF-βl in the
renal tubular interstitium after four weeks. |
Table V
Expression of DCN and TGF-βl in the
renal tubular interstitium after four weeks.
| Item | Group A | Group B | Group C | Group D |
|---|
| DCN | 1.20±0.44 | 1.41±0.18 | 1.32±0.57 | 2.39±0.54a,b |
| TGF-βl | 1.19±0.44 | 1.91±0.18 | 1.66±0.57 | 1.49±0.49 |
Discussion
In the model rats that had undergone 5/6
nephrectomy, Cr and urea levels in the plasma peaked on the 10th
day and then decreased gradually, prior to increasing again on the
60th day. These results were consistent with those reported
previously in which the levels increased initially in the fourth
week, indicating that renal function experienced a gradual
progression from acute kidney injury into CRF (18). AS frequently occurs in patients
with end-stage uremia, blood and peritoneal dialysis, nephrotic
syndrome and other renal diseases, and is an important complication
in patients with advanced renal failure (19). In the present study, the levels of
TG and T-Ch in the plasma of the experimental group were
significantly higher than those of the control group on the 10th,
20th, 30th and 60th days respectively (P<0.05). This study shows
that abnormal lipid metabolism exists at the early stage of CRF,
which typically suggests an imbalance in the lipid transport and
lipid metabolism regulatory systems, as well as other abnormal
changes. In particular, increased TG levels in the plasma may
contribute to the early diagnosis of CRF cardiovascular
complications (20).
In the present study, the lipid levels were
dynamically observed in the aortic arches of the experimental group
rats during the formation of CRF on the 10th, 20th and 40th days
subsequent to 5/6 nephrectomy. It was found that the TG, T-CH and
T-PL levels were higher than those of the control group on the 10th
day and then continued to rise linearly. The TG level in the aortic
arches was significantly increased on the 30th day (P<0.05;
Fig. 2). The levels of T-Ch was
significantly elevated in the aortic arches (P<0.001) and that
of T-PL decreased significantly on the 60th day. The results
suggest that lipid deposition occurs in the aorta on the 30th day
after 5/6 nephrectomy, and that the increases in TG and T-Ch levels
in the aortic arches occur simultaneously with those in the plasma.
In the aortic tissues, the TG levels were elevated first, followed
by increases in the T-Ch and T-PL levels; this indicates that TG
was deposited in the aortic tissue in early CRF more rapidly than
cholesterol and phospholipid. Cholesterol deposition was
subsequently accelerated. The cholesterol deposition in the aortic
intima may explain the development of AS (21). The TG and T-Ch levels in plasma
were significantly positively correlated with those in aortic
tissue (r=0.99 and r=0.97, respectively), while the T-PL level in
plasma was significantly negatively correlated with that in aortic
tissue (r=−0.92), suggesting that plasma lipid levels may reflect
the deposition in aortic tissue and that the TG level may be the
earliest indicator for aortic lipid deposition (22). In triglyceridemia, the transport
reaction of the core lipid of lipoprotein is enhanced to
collaborate with cholesterol in protein transfer, which transfers
cholesterol ester from HDL to very-low-density lipoprotein (VLDL)
(the predecessor of LDL). Furthermore, TG is transferred from VLDL
to HDL, leading to elevations in LDL-cholesterol and reductions in
HDL (23). In addition, a
non-esterified fatty acid is produced when lipoprotein lipase
exerts its hydrolytic effect, which increases the permeability of
the tunica intima and promotes LDL-cholesterol deposition in the
cell. Non-esterified fatty acids can additionally promote platelet
adhesion on the vessel wall and reduce the activity of the
fibrinolytic system to collaborate in inducing AS (24). The levels of T-Ch in the
erythrocyte membranes were significantly positively correlated with
those in the plasma (r=0.97); the increase in T-Ch level and
decrease in T-PL level led to increased erythrocyte viscosity and
membrane and decreased deformation ability (25). Thus, the results revealed that the
abnormal lipid metabolism in CRF leads to microcirculatory
disturbance in all tissues as well as cardiovascular
complications.
After four weeks, the BWs and blood lipid levels of
each treatment group were increased compared with the basic levels,
but no significant differences were observed among the groups. The
influence of blood lipids on renal function and pathology was
therefore excluded (26). The
serum Cr level of rats in Group D was significantly lower than that
of rats in Groups B and C, indicating that DCN can alleviate the
renal function of kidney failure rats (27). In terms of the pathological
mechanism in the kidney, it was additionally observed that DCN
mitigated the renal interstitial fibrosis of rats, which thus
verified the hypothesis that DCN is able to repair renal fibrosis
and delay renal failure. The expression levels of DCN and TGF-βl in
the kidneys of Groups B, C and D were increased to varying degrees
compared with those of Group A. Furthermore, the expression of DCN
was significantly higher in Group D than that in Groups B and C;
this was associated with the DCN expression of the DCN-transfected
FBs in the renal tissue (28). The
increases in TGF-β1 expression in the model rats were closely
associated with the progression of the impairment of renal
function. The balance between DCN and TGF-β1 in the kidney during
renal failure is therefore critical. High levels of DCN can
neutralize TGF-β1, thereby reducing pathological renal damage and
improving renal function (29).
Furthermore, the application of exogenous DCN or DCN genetic
therapy can prevent extracellular matrix accumulation (30,31).
In conclusion, DCN is feasible in the treatment of renal diseases
resulting from the excessive activity of TGF-β1. DCN may also can
mitigate the abnormal lipid metabolism and cardiovascular
complications in CRF.
References
|
1
|
Wang L, Wang J, Wang Y, Fu Q, Lei YH, Nie
ZY, Qiu J and Bao TY: Protective effect of exogenous matrix
metalloproteinase-9 on chronic renal failure. Exp Ther Med.
7:329–334. 2014.PubMed/NCBI
|
|
2
|
Bhagwat R, Joshi SP, Salgia P and Sepaha
A: Lipid abnormalities in chronic renal failure. Indian J Clin
Biochem. 12:81–85. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kim HJ, Moradi H, Yuan J, Norris K and
Vaziri ND: Renal mass reduction results in accumulation of lipids
and dysregulation of lipid regulatory proteins in the remnant
kidney. Am J Physiol Renal Physiol. 296:F1297–1306. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Muntener P, Coresh J, Smith JC, Eckfeldt J
and Klag MJ: Plasma lipids and risk of developing renal
dysfunction: the atherosclerosis risk in communities study. Kidney
Int. 58:293–301. 2000. View Article : Google Scholar
|
|
5
|
Caimi G, Carollo C, Montana M, Vaccaro F
and Lo Presti R: Elastase, myeloperoxidase, nitric oxide
metabolites and oxidative status in subjects with clinical stable
chronic renal failure on conservative treatment. Clin Hemorheol
Microcirc. 43:253–258. 2009.PubMed/NCBI
|
|
6
|
Liu N, Tolbere E, Pang M, Ponnusamy M, Yan
H and Zhuang S: Suramin inhibits renal fibrosis in chronic kidney
disease. J Am Soc Nephrol. 22:1064–1075. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Han JY, Kim YJ, Kim L, Choi SJ, Park IS,
Kim JM, Chu YC and Cha DR: PPARgamma agonist and angiotensin II
receptor antagonist ameliorate renal tubulointerstitial fibrosis. J
Korean Med Sci. 25:35–41. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Suzuki S, Ohashi N and Kitagawa M: Roles
of the Skp2/p27 axis in the progression of chronic nephropathy.
Cell Mol Life Sci. 70:3277–3287. 2013. View Article : Google Scholar :
|
|
9
|
Chen G, Chen H, Wang C, Peng Y, Sun L, Liu
H and Liu F: Rapamycin ameliorates kidney fibrosis by inhibiting
the activation of mTOR signaling in interstitial macrophages and
myofibroblasts. PLoS One. 7:March 28–2012.(Epub ahed of print).
View Article : Google Scholar
|
|
10
|
Pedersen EB, Ardal B, Bech JN, Lauridsen
TG, Larsen NA, Mikkelsen L, Sangill M and Thomsen IM: The effect of
glucose added to the dialysis fluid on blood pressure, vasoactive
hormones and energy transfer during hemodialysis in chronic renal
failure. Open J Neph. 1:5–14. 2011. View Article : Google Scholar
|
|
11
|
Pohjolainen V, Rysä J, Näpänkangas J,
Kööbi P, Eräranta A, Ilves M, Serpi R, Pörsti I and Ruskoaho H:
Left ventricular periostin gene expression is associated with
fibrogenesis in experimental renal insufficiency. Nephrol Dial
Transplant. 27:115–122. 2012. View Article : Google Scholar
|
|
12
|
Mu J, Li YK and Fu SG: Influence of Shenqi
Recipe on mesangial cells and interstitial fibroblasts of chronic
renal failure rats. Zhong Xi Yi Jie He Xue Bao. 1:122–124. 2003.(In
Chinese). View Article : Google Scholar
|
|
13
|
Korish AA and Arafah MM: Catechin combined
with vitamins C and E ameliorates insulin resistance (IR) and
atherosclerotic changes in aged rats with chronic renal failure
(CRF). Arch Gerontol Geriatr. 46:25–39. 2008. View Article : Google Scholar
|
|
14
|
Görs S, Kucia M, Langhammer M, Junghans P
and Metges CC: Technical note: Milk composition in mice -
methodological aspects and effects of mouse strain and lactation
day. J Dairy Sci. 92:632–637. 2009. View Article : Google Scholar
|
|
15
|
Kang NH, Lee WK, Yi BR, Park MA, Lee HR,
Park SK, Hwang KA, Park HK and Choi KC: Modulation of lipid
metabolism by mixtures of protamine and chitooligosaccharide
through pancreatic lipase inhibitory activity in a rat model. Lab
Anim Res. 28:31–38. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wasserman DH, Lacy DB, Goldstein RE,
Williams PE and Cherrington AD: Exercise-induced fall in insulin
and increase in fat metabolism during prolonged muscular work.
Diabetes. 38:484–490. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Stoof J, Kuipers EJ and van Vliet AH:
Characterization of NikR-responsive promoters of urease and metal
transport genes of Helicobacter mustelae. Biometals. 23:145–159.
2010. View Article : Google Scholar
|
|
18
|
Lönn J, Shahzad F, Uhlin F, Bengtsson T,
Almroth G and Nayeri F: High concentration but low biological
activity of hepatocyte growth factor in patients with chronic renal
failure. Adv Biosci Biotechnol. 3:516–523. 2012. View Article : Google Scholar
|
|
19
|
Hirako M, Kamiya T, Misu N, Kobayashi Y,
Adachi H, Shikano M, Matsuhisa E and Kimura G: Impaired gastric
motility and its relationship to gastrointestinal symptoms in
patients with chronic renal failure. J Gastroenterol. 40:1116–1122.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sasikala M, Subramanyam C and Sadasivudu
B: Early oxidative change in low density lipoproteins during
progressive chronic renal failure. Indian J Clin Biochem.
14:176–183. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Inaguma D, Tatematsu M, Shinjo H, Suzuki
S, Mishima T, Inaba S and Kurata K: Effect of an educational
program on the predialysis period for patients with chronic renal
failure. Clin Exp Nephrol. 10:274–278. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kuwahara M, Inoshita S, Nakano Y, Terada
Y, Takano Y and Sasaki S: Expression of bone type 1 PTH receptor in
rats with chronic renal failure. Clin Exp Nephrol. 11:34–40. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sadykov AS, Salikhov ShI, et al:
Investigation of membrane-active components from blood serum of
patients with chronic renal failure. Bull Exp Biol Med.
94:1408–1410. 1982. View Article : Google Scholar
|
|
24
|
Markou N, Kanakaki M, et al:
Sleep-disordered breathing in nondialyzed patients with chronic
renal failure. Lung. 184:43–49. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Gavrisheva NA, Malinin VV, Ses TP, Kozlov
KL, Panchenko AV and Titkov AY: Effect of peptide Vilon on the
content of transforming growth factor-beta and permeability of
microvessels during experimental chronic renal failure. Bull Exp
Biol Med. 139:24–26. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Li P, Ma LL, Xie RJ, et al: Treatment of
5/6 nephrectomy rats with sulodexide: a novel therapy for chronic
renal failure. Acta Pharmacol Sin. 33:644–651. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Pusoonthornthum R, Pusoonthornthum P and
Krishnamra N: Calcium-phosphorus homeostasis and changes in
parathyroid hormone secretion in cats with various stages of
spontaneous chronic renal failure. Comp Clin Pathol. 19:287–293.
2010. View Article : Google Scholar
|
|
28
|
Kihara Y, Matsuno N, Mijiti A, Nagao T,
Takeuchi H, Unezaki S and Hirano T: Comparative study of the
cellular pharmacodynamics of calcineurin inhibitors between
patients with chronic renal failure awaiting renal transplantation
and cirrhosis patients awaiting liver transplantation. Cell
Transplant. 18:639–646. 2009.PubMed/NCBI
|
|
29
|
Ienaga K, Mikami H and Yokozawa T: First
indications demonstrating the preventive effects of NZ-419, a novel
intrinsic antioxidant, on the initiation and/or progression of
chronic renal failure in rats. Biol Pharm Bull. 32:1204–1208. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
De Beuf A, D’Haese PC and Verhulst A:
Epoetin delta as an antifibrotic agent in the remnant kidney rat: a
possible role for transforming growth factor beta and hepatocyte
growth factor. Nephron Exp Nephrol. 115:e46–e59. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Lin Z, Wang JS, Lin L, et al: Effects of
BMP2 and VEGF165 on the osteogenic differentiation of rat bone
marrow-derived mesenchymal stem cells. Exp Ther Med. 7:625–629.
2014.PubMed/NCBI
|