Introduction
Global infarction of the testes is a common
diagnosis in urologic emergencies. Possible causes include torsion
of the spermatic cord, incarcerated hernia, severe epididymitis and
iatrogenic injury (1). In
contrast, the segmental infarct of the testicle is uncommon. The
condition is typically idiopathic and usually affects patients
between the second and the fourth decades of life. The classical
clinical presentation of segmental testicular infarction would be
acute onset of scrotal pain which mimics testicular torsion.
However the radiological presentation of segmental testicular
infarction would resemble that of testicular tumor, and tends to
prompt treatment by radical surgery. Thus, the diagnosis was
usually established following orchidectomy (2) Only a few cases of segmental
testicular infarction have been reported previously (3,4). The
present study describes a case of acute scrotum in a 23-year-old
male.
Case report
A 23-year-old male with unremarkable past medical
history was admitted due to worsening right testicular pain that
had been present for three days. Physical examination revealed a
mildly swollen right testis with tenderness in the upper pole. The
testis was otherwise normal with no mass or hernia. Results of a
complete blood count, urinalysis and tumor marker profile were all
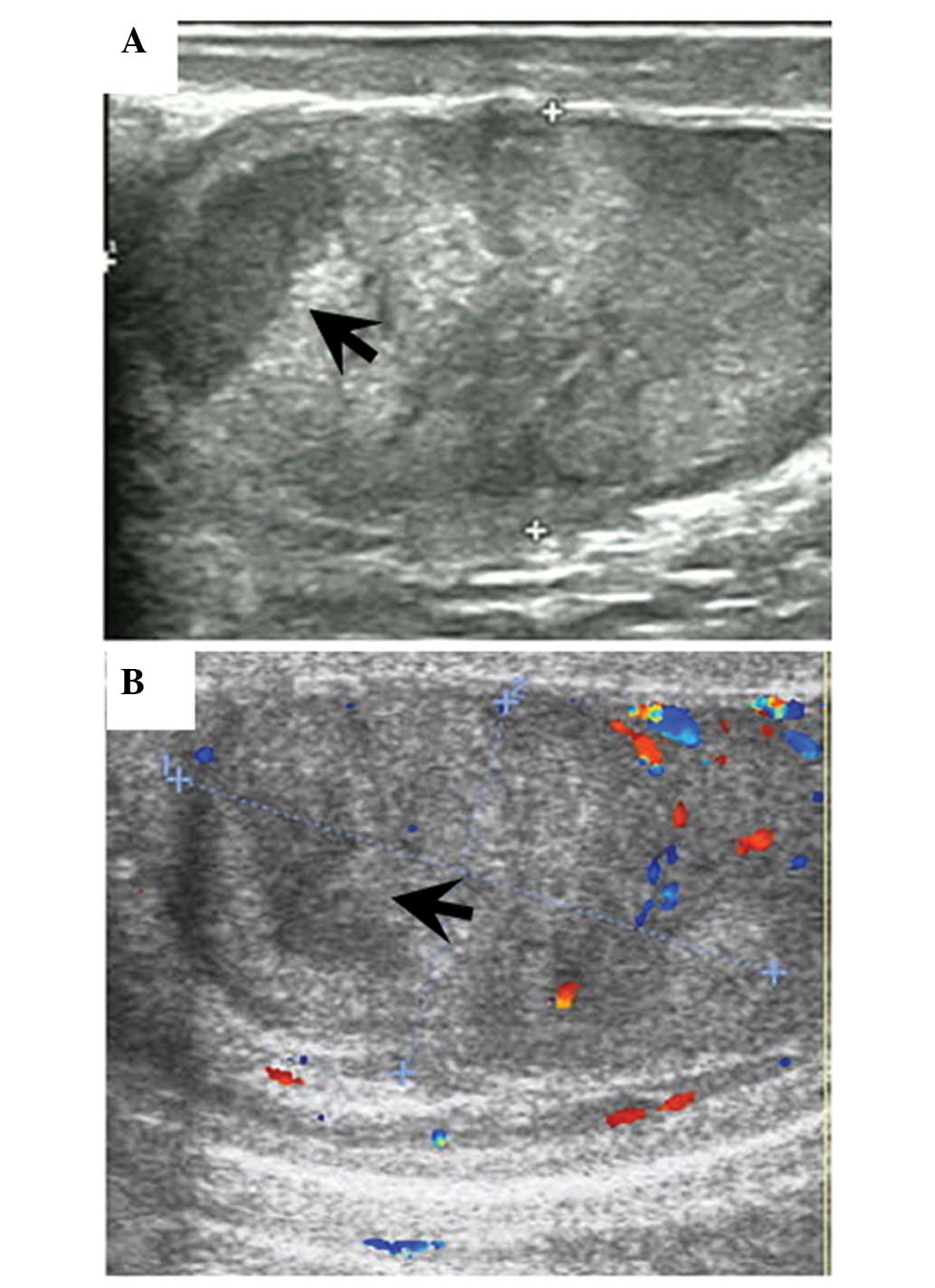
within the normal range. Color Doppler sonography demonstrated a
flowless, well-demarcated, hypoechoic mass located in the upper
pole of the right testis (Fig. 1).
The remaining area of the testis exhibited normal echogenicity and
vascularity. Since the underlying cause of the testicular pain was
unclear, surgical exploration was performed.
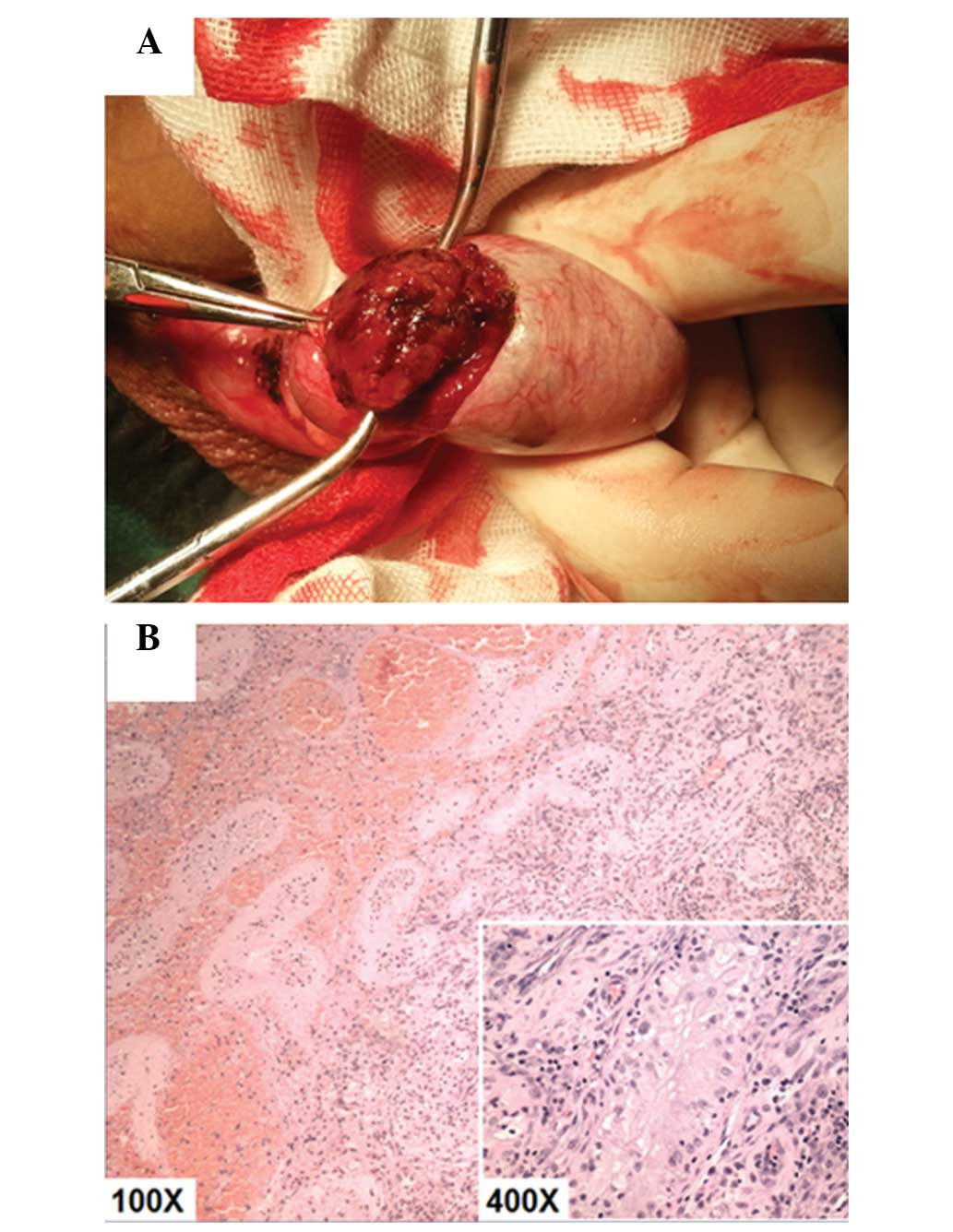
The patient’s scrotum was immediately explored via a
scrotal approach. During the surgery, the upper pole of the testis
showed a faint blue discoloration; however, no torsion of the
spermatic cord or the epididymis was detected. The tunica albuginea
of the testicle was incised, revealing necrosis of the upper pole
with grossly normal residual testis tissue (Fig. 2A). Partial orchiectomy was
performed. The pathological examination of the excised specimen
showed diffuse hemorrhagic infarction of the testis tissue, with
the surrounding normal tissue exhibiting the characteristic
histological features of sertoli cell-only syndrome (Fig. 2B). The surgery was successful, with
no complications, and the patient fully recovered. Written informed
consent was obtained from the patient prior to publication of this
case report and of any accompanying images.
Discussion
Segmental infarct of testicle is a rare clinical
entity that is usually diagnosed following orchiectomy. Since the
first reported case in 1909 (5),
<70 cases have been reported. The condition typically has an
idiopathic etiology, although in certain cases predisposing factors
for segmental infarction have been noted, such as
hypercoagulability disorders, vasculitis, trauma, infection,
torsion and iatrogenic vascular injury (3–8). In
the present case, the presence of sertoli cell-only syndrome would
possibly indicate an association between spermatogenesis and
segmental testicular infarction, as similar spermatogenesis arrest
morphology was described in the case reported by Baratelli et
al (9); however, whether there
exists a convincing association warrants further study.
The most common symptom of segmental testicular
infarction is testis pain, which is unspecific and
indistinguishable from that of other scrotal diseases. Differential
diagnosis should thus depend on laboratory tumor marker screening
and imaging. Although a previous study proposed the diagnostic
value of magnetic resonance imaging in segmental testicular
infarction (10), scrotal
ultrasound remains the most simple and useful tool to distinguish
segmental testicular infarction from other diseases (11). The use of imaging to differentiate
segmental testicular infarction from testis tumor relies on the
recognition that the typical ischemic region should resemble the
lobular morphology of the testicle (12); therefore, the characteristic
ultrasound finding would be an avascular, wedge-shaped, hypoechoic
lesion with well-defined borders. Additional shear-wave
elastography would increase the accuracy of the diagnosis (13).
The management strategy for segmental testicular
infarction remains controversial. The primary intention of surgical
intervention is the salvage of testicular tissue along with the
pathological exclusion of malignancy. Testis-sparing surgery is
therefore an optimal surgical choice, particularly for younger
patients (14). Despite this, the
majority of segmental testicular infarction cases in the literature
have resulted in radical orchiectomy (1,2,4,7),
since it is difficult to establish a firm diagnosis preoperatively,
and the possibility of testis tumor should always be taken into
consideration in these cases. A conservative strategy is also
recommended. In a case series by Madaan et al (15), 16 out of 19 cases of segmental
testicular infarction were successfully managed by careful
observation, and nine patients had gradual regression of the lesion
in the follow-up ultrasonography. Conservative management with
careful observation is also considered feasible and safe whenever
segmental testicular infarction can be diagnosed with
certainty.
In conclusion, we propose that segmental testicular
infarction should be considered in patients with acute testicular
pain. Either surgical exploration or careful observation is
suitable when a preoperative laboratory and imaging evaluation
supports a firm diagnosis.
References
|
1
|
Secil M, Kocyigit A, Aslan G, et al:
Segmental testicular infarction as a complication of
varicocelectomy: sonographic findings. J Clin Ultrasound.
34:143–145. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Costa M, Calleja R, Ball RY and Burgess N:
Segmental testicular infarction. BJU Int. 83:5251999. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sentilhes L, Dunet F, Thoumas D, Khalaf A,
Grise P and Pfister C: Segmental testicular infarction: diagnosis
and strategy. Can J Urol. 9:1698–1701. 2002.
|
|
4
|
Arce Terroba Y, Algaba-Arrea F and
Villavicencio Maverich H: Segmental infarct of testicle: an
infrequent pseudotumor. Actas Urol Esp. 34:194–200. 2010.(In
Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Johnston JH: Localised infarction of the
testis. Br J Urol. 32:97–99. 1960. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gofrit ON, Rund D, Shapiro A, Pappo O,
Landau EH and Pode D: Segmental testicular infarction due to sickle
cell disease. J Urol. 160(3 Pt 1): 835–836. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chin SC, Wu CJ, Chen A and Hsiao HS:
Segmental hemorrhagic infarction of testis associated with
epididymitis. J Clin Ultrasound. 26:326–328. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nistal M, Palacios J, Regadera J and
Paniagua R: Postsurgical focal testicular infarct. Urol Int.
41:149–151. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Baratelli GM, Vischi S, Mandelli PG,
Gambetta GL, Visetti F and Sala EA: Segmental hemorrhagic
infarction of testicle. J Urol. 156:14421996. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kodama K, Yotsuyanagi S, Fuse H, Hirano S,
Kitagawa K and Masuda S: Magnetic resonance imaging to diagnose
segmental testicular infarction. J Urol. 163:910–911. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Aquino M, Nghiem H, Jafri SZ, Schwartz J,
Malhotra R and Amin M: Segmental testicular infarction: sonographic
findings and pathologic correlation. J Ultrasound Med. 32:365–372.
2013.PubMed/NCBI
|
|
12
|
Fernández-Pérez GC, Tardáguila FM, Velasco
M, et al: Radiologic findings of segmental testicular infarction.
AJR Am J Roentgenol. 184:1587–1593. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kantarci F, Cebi Olgun D and Mihmanli I:
Shear-wave elastography of segmental infarction of the testis.
Korean J Radiol. 13:820–822. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sharma SB and Gupta V: Segmental
testicular infarction. Indian J Pediatr. 72:81–82. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Madaan S, Joniau S, Klockaerts K, et al:
Segmental testicular infarction: conservative management is
feasible and safe. Eur Urol. 53:441–445. 2008. View Article : Google Scholar
|