Introduction
Acute suppurative thyroiditis (AST), an inflammatory
disease of the thyroid gland, is extremely rare in adults, since
they typically exhibit a strong resistance to local infection
(1). Thyroid abscesses are more
likely to occur in children in instances of congenital anomaly
(2). The majority of AST cases are
caused by Gram-positive Streptococcus species (3). If AST is left untreated, it may enter
the neck or extend to the chest. Rupture of the abscess into the
esophagus or trachea is also possible. Despite outpatient
parenteral antibiotic therapy, a number of cases have required
surgical drainage in conjunction with the removal of any associated
anatomic abnormality, in order to decrease the recurrence of
abscess formation (4). Abscesses
may exhibit anechoic or internal echoes; therefore, it may not be
possible to establish a definitive diagnosis using standard
ultrasonography alone. In such cases, ultrasound-guided fine-needle
aspiration cytology (FNAC) and bacterial culture may be performed
to confirm the diagnosis. The present study reports two cases of
AST that were accompanied by abscesses, together with a review of
the literature.
Case reports
Case 1
A seven-year-old male patient presented with a
painful swelling in the left side of the neck, a sore throat and a
hoarse voice for one day, as well as fever for four days.
Laboratory analyses revealed a leukocyte count of 12,940/ml, with
66.1% neutrophils and 26% lymphocytes, and normal thyroid function.
The blood culture was sterile with no bacterial presence; however,
the patient received ampicillin on admission. Ultrasonography
examination of the neck revealed a 30×25×21 mm3
heterogeneous hypoechoic mass with hyperechoic spots, which almost
filled the entire left lobe and isthmus of the thyroid gland. In
addition, peripheral and interval vascular flow was observed,
indicating a malignant nodule (Fig. 1A
and B). A FNAC procedure was performed using a disposable 5-ml
syringe on the sixth day following patient admission. The
aspiration fluid was expressed onto slides, and smears were
prepared. One of the smears was immediately fixed in 95% ethyl
alcohol for subsequent hematoxylin-eosin staining. The remaining
smears were air-dried and stained rapidly with Diff-Quik (Baso
diagnostics Inc., Zhuhai, China). The FNAC procedure revealed no
evidence of nodule malignancy. A mixture of various inflammatory
cells were observed; however, no follicular cells were identified
(Fig. 1C). A 0.1-ml sample of
pus-like fluid was extracted from the abscess by aspiration, which
subsequently grew colonies of viridans streptococci when cultured,
confirming the diagnosis of AST. However, the abscess was not
surgically drained as the patient exhibited clinical improvement
after receiving antibiotics. Written informed patient consent was
obtained from the patient’s family prior to participation in the
present study.
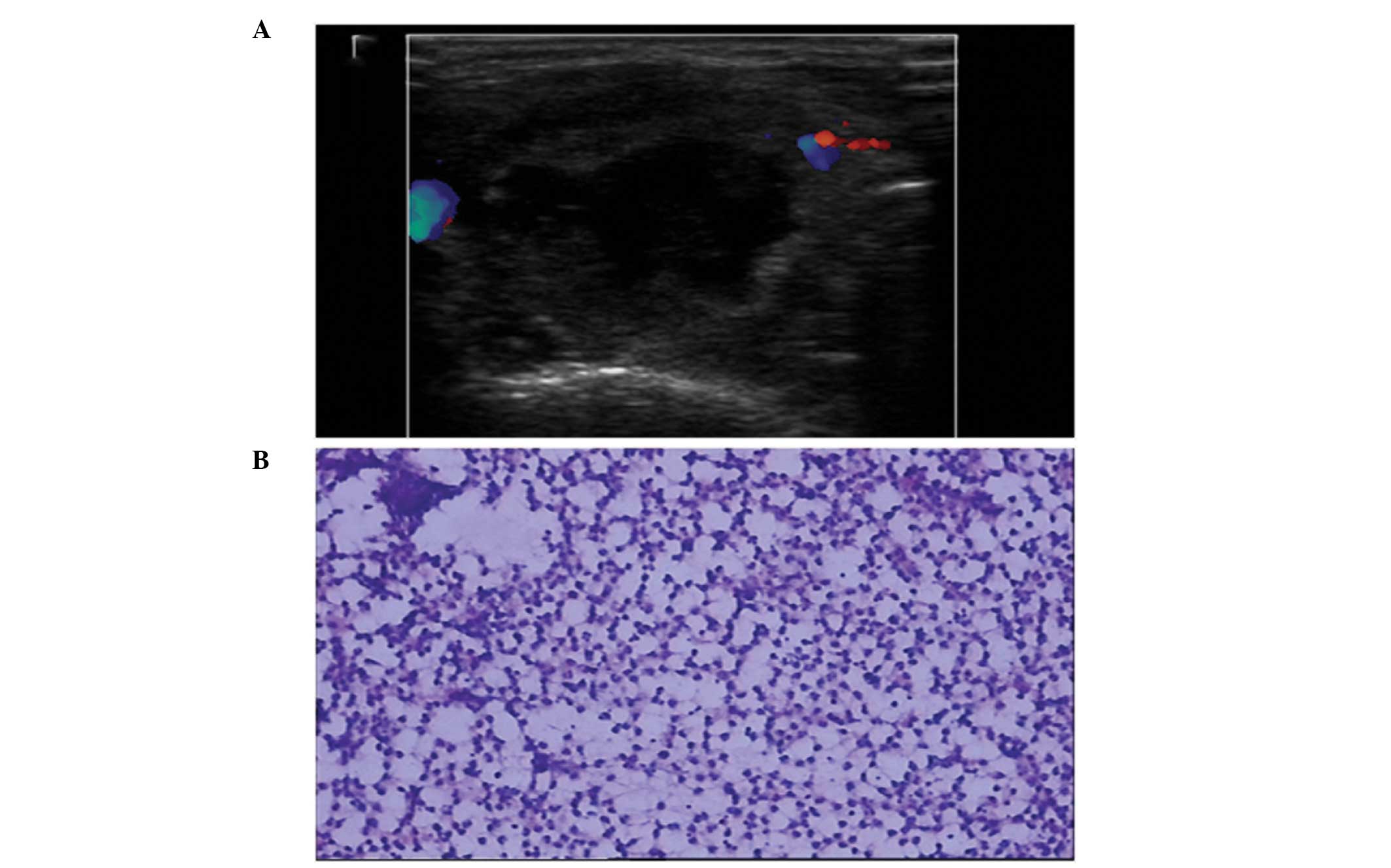
Case 2
A nine-year-old male patient was admitted to the
General Hospital (Tianjin, China) suffering from painful swelling
and fever for two days. Laboratory examinations revealed a
leukocyte count of 12,400/ml, consisting of 76.4% neutrophils and
18.2% lymphocytes, and normal thyroid function. A 23×21×20
mm3 cystic mixed mass was observed in the left lobe of
thyroid gland, with no interval vascular flow (Fig. 2A). A FNAC examination was
subsequently performed. A 2-ml sample of purulent yellow-brown
fluid was extracted from the abscess, after which the anechoic area
disappeared. A number of the smears were rapidly stained with
Diff-Quik and the remainder were stained by the conventional
hematoxylin-eosin method. Aspiration cytology revealed no thyroid
follicular cells; however, numerous neutrophils and a number of
macrophages were observed (Fig.
2B). Culture of the aspirated fluid resulted in the growth of
viridans streptococci. Thus, a diagnosis of AST with an abscess was
confirmed. The patient was treated with ampicillin upon admission
and the fever subsided two days after the FNAC procedure. Written
informed patient consent was obtained from the patient’s family
prior to participation in the present study.
Discussion
The thyroid gland is known to strongly resist
infections due to its encapsulation, abundant blood supply and
lymph nodes, iodine concentration and generation of hydrogen
peroxide (5). A thyroid abscess
caused by AST is an extremely rare form of solitary thyroid nodule,
which results from an infection via a pyriform sinus fistula
(6) and is most commonly observed
in children (7). According to the
results of previously published studies and the anatomical and
histological results of the current case reports, the authors of
the present study believe that the development of the fistulas
originated from the embryonic remnant of the fourth branchial
pouch, which regularly presents in the first decade of life
(8–10).
Streptococcal, staphylococcal and pneumococcal are
the three types of infection most commonly associated with cases of
AST (3). The disorder is primarily
characterized by a sudden enlargement and tenderness of the thyroid
gland, accompanied by a fever, sore throat, dysphagia, hoarseness
and a limited range of head movement (11). Ultrasound examination provides
real-time imaging of the affected area without the use of ionizing
radiation, and is able to reveal intra- or extra-thyroid abscesses
and solid or mixed lesions of the thyroid gland. However, the
echotexture of an abscess may vary due to extensive internal debris
or hemorrhage, accompanied by peripheral and interval vascular
flow. In such cases, a definitive diagnosis may be impossible to
establish using ultrasonography alone, and FNAC may play a
significant role in discriminating between benign and malignant
lesions, while generating few complications (12). The use of a rapid staining protocol
allows the quality of the stain, smear and specimen to be assessed
immediately (13). In the two
present cases, a diagnosis of AST was rapidly and easily
established on the basis of Diff-Quik staining only. However,
additional materials may be evaluated using hematoxylin-eosin
staining to aid a more specific final diagnosis. If there is a
notable anechoic area in the lesion, pus-fluid can be collected
during the FNAC procedure and cultured. In the present cases, the
cultures revealed the presence of veridians streptococci, which are
normal microbiota encountered in the respiratory tract. The
existence of a pyriform sinus fistula was suspected, where the
sinus exhibits a proximal opening in the apex of the pyriform fossa
and the distal end extends to the thyroid, resulting in the thyroid
becoming prone to inflammation and infection.
In the present cases, the viridans streptococci
responded to treatment with ampicillin; thus, surgical drainage of
the abscesses was unnecessary. However, AST patients require a
close clinical follow-up to ensure the complete elimination of the
infection. In a limited number of cases, surgical excision of the
fistula may be performed in combination with a direct laryngoscopy
examination, in order to prevent the recurrence of thyroiditis. In
case 1, ultrasonography revealed a heterogeneous hypoechoic mass
with hyperechoic spots, similar to a neoplasm, which may be falsely
diagnosed as a thyroid malignancy. A combination of FNAC and
bacterial culture may aid the diagnosis of AST. Furthermore, during
the aspiration procedure, abscess fluids may be collected, and
further surgical drainage is rarely required, as was observed in
case 2. In cases exhibiting a large abscess, surgical drainage
should be followed by antibiotic treatment.
In summary, FNAC of the thyroid gland is useful for
establishing a diagnosis of AST with a thyroid abscess. This
procedure may prove to be a less invasive and more efficient,
timely and feasible method for discriminating between benign and
malignant thyroid gland nodules, in order to ensure that the
appropriate treatment is administered.
References
|
1
|
Paes JE, Burman KD, Cohen J, et al: Acute
bacterial suppurative thyroiditis: a clinical review and expert
opinion. Thyroid. 20:247–255. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pal I, Sengupta S, Balakrishnan R and
Gupta A: Fourth branchial pouch sinus - an unusually late initial
presentation. Indian J Otolaryngol Head Neck Surg. 61:72–75. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bravo E and Grayev A: Thyroid abscess as a
complication of bacterial throat infection. J Radiol Case Rep.
5:1–7. 2011.PubMed/NCBI
|
|
4
|
Parida PK, Gopalakrishnan S and Saxena SK:
Pediatric recurrent acute suppurative thyroiditis of third
branchial arch origin - our experience in 17 cases. Int J Pediatr
Otorhinolaryngol. 78:1953–1957. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hong JT, Lee JH, Kim SH, et al: Case of
concurrent Riedel’s thyroiditis, acute suppurative thyroiditis, and
micropapillary carcinoma. Korean J Intern Med. 28:236–241. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Prajapaty B and Shah B: Recurrent cervical
abscess due to pyriform sinus fistula - a case report. Indian J
Otolaryngol Head Neck Surg. 49:391–393. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Pearce EN, Farwell AP and Braverman LE:
Thyroiditis. N Engl J Med. 348:2646–2655. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Desai AA, Pandya VK, Chougule S and Nair
U: Recurrent thyroid abscess - Is it a fourth branchial
archanomaly? Indian J Otolaryngol Head Neck Surg. 58:190–191.
2006.PubMed/NCBI
|
|
9
|
Nicoucar K, Giger R, Pope HG Jr, Jaecklin
T and Dulguerov P: Management of congenital fourth branchial arch
anomalies: a review and analysis of published cases. J Pediatr
Surg. 44:1432–1439. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shrime M, Kacker A, Bent J and Ward RF:
Fourth branchial complex anomalies: a case series. Int J Pediatr
Otorhinolaryngol. 67:1227–1233. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ghaemi N, Sayedi J and Bagheri S: Acute
suppurative thyroiditis with thyroid abscess: a case report and
review of the literature. Iran J Otorhinolaryngol. 26:51–55.
2014.PubMed/NCBI
|
|
12
|
Vasudev V, Hemalatha AL, Rakhi B and
Githanjali S: Efficacy and pitfalls of FNAC of thyroid lesions in
children and adolescents. J Clin Diagn Res. 8:35–38.
2014.PubMed/NCBI
|
|
13
|
Powers CN: Diagnosis of infectious
diseases: a cytopathologist’s perspective. Clin Microbiol Rev.
11:341–365. 1998.PubMed/NCBI
|