Introduction
The incidence of cerebral venous sinus thrombosis
(CVST) is 3–4/million/year. CVST accounts for <1% of apoplexy.
Misdiagnosis and missed diagnosis of CVST are common due to the
atypical symptoms of the condition at an early stage (1–3).
However, the extensive use of new imaging techniques, including
computed tomography (CT), computed tomography venography, magnetic
resonance imaging (MRI) and magnetic resonance venography (MRV),
allows for the early diagnosis of CVST. The present first-line
treatment is systemic anticoagulation (4,5).
Although early diagnosis and active anticoagulant therapy has
reduced the mortality of CVST from 40% in the 1980s to the current
rate of 4.39–13% (6–8), the disability and mortality rates in
patients with acute onset CVST remain relatively high despite the
use of heparin therapy. In the International Study on Cerebral Vein
and Dural Sinus Thrombosis, Ferro et al reported that the
mortality rate of patients in a coma was 38% (7). Active treatment should be provided to
these patients. Evidence from minor cases indicates that local
thrombolytic therapy is relatively safe and effective in rapidly
recanalizing thrombosed sinuses and reversing neurological deficits
(9,10). Local intrasinus thrombolysis
dissolves the thrombus by infusing the thrombolytic drug into the
occluded sinus and employing mechanical thrombectomy to recanalize
the sinus as early as possible. Mechanical thrombectomy may
strengthen the thrombolytic effect of drugs. As a common type of
thrombolytic agent, recombinant tissue plasminogen activator
(rt-PA) is widely utilized in intra-arterial thrombolysis and is
safer compared with urokinase. Therefore, in the present study,
intrasinus mechanical thrombectomy was combined with thrombolysis
using rt-PA to manage severe CVST. However, due to the absence of
randomized controlled trials, the exact role of intrasinus
thrombolysis and mechanical thrombectomy in the management of CVST
is unclear, particularly with regard to patient selection, optimal
time to intervene and contraindications of this therapy.
Retrospective data analysis of eight patients with severe CVST who
were subjected to local thrombectomy combined with intrasinus rt-PA
thrombolysis was conducted to evaluate the effectiveness and safety
of this endovascular interventional therapy for severe CVST.
Materials and methods
General materials
Eight patients with CVST were treated in Northern
Jiangsu People’s Hospital (Yangzhou, China) between December 2009
and December 2011. Of the eight patients, two were males and six
were females. Patient age ranged between 19 and 48 years with an
average of 27.5±10.4 years. One patient was in puerperium, two
patients had a long-term history of contraceptive use, one patient
had a history of deep vein thrombosis and two patients had severe
anemia, the remaining two patients had no evident risk factors. The
clinical manifestations were as follows: Headache associated with
progressive disturbance of consciousness in all the patients, focal
neurological deficit symptoms in six patients and epilepsy in two
patients. Two patients progressed to the stage of cerebral hernia
while undergoing endovascular treatment. Glasgow Coma Scale (GCS)
scores were between 4 and 9 with an average score of 8.3±2.7
points. The duration from the onset of symptoms to the receipt of
interventional therapy ranged between 3 and 12 days. The study was
conducted in accordance with the Declaration of Helsinki and was
approved by the Ethics Committee of Northern Jiangsu People’s
Hospital. Written informed consent was obtained from all the
participants or their families.
Imaging materials
Patients were diagnosed via CT, MRI, MRV and/or
digital subtraction angiography (DSA). Thrombus locations were as
follows: Superior sagittal sinus in one case, superior sagittal
sinus and left transverse sinus in one case, superior sagittal
sinus and straight sinus in one case, straight sinus and left
transverse sinus in four cases and straight sinus and right
transverse sinus in one case. The patients exhibited varied degrees
of cerebral venous infarction and two cases exhibited cerebral
hemorrhage.
Treatment method
Transforaminal herniation occurred in one patient
3-h after hospitalization and decompressive craniectomy was
performed. The other seven patients were subjected to systemic
anticoagulation with heparin following definite diagnosis, however,
progressive aggravation or no improvement of symptoms was observed
within 24 h. Interventional treatment was provided with general
anesthesia. Vessel sheaths were inserted in the left femoral vein
and right femoral artery. Arterial catheterization with a 5 F
catheter was performed in the cerebral artery. The procedure
confirmed the location of thrombosis and was utilized for the
arterial administration of thrombolytic drugs in addition to the
evaluation of the sinus thrombolytic effect. A 6 F Envoy support
catheter (Cordis Neurovascular, Inc., Miami Lakes, FL, USA) was
inserted through the femoral vein. The support catheter was placed
in the left or right sigmoid sinus with the aid of a 0.35 loach
guidewire based on the location of the lesion. A Prowler 14
microcatheter (Cordis Neurovascular, Inc.) guided by an Essence 14
micro guidewire (Cordis Neurovascular, Inc.) penetrated the
thrombosis. If the thrombus was in the superior sagittal sinus or
transverse sinus, the Trensend 300 Floppy exchange guidewire
(Boston Scientific Target, Bayside Parkway, Fremone, CA, USA) was
selected and placed in the dilated sacculus after being expanded in
advance. By contrast, if the thrombus was in the straight sinus, a
microcatheter, with which the rt-PA (Actilyse; BoehringerIngelheim
Pharmaceuticals, Ingelheim, Germany) was administered, was directly
placed in the distal end of the thrombus. Following thrombolysis,
the support catheter was removed, whereas the microcatheter
remained. The arterial catheter and sheath were removed. Patients
were administered 15 mg rt-PA via the microcatheter and 5 mg rt-PA
via the arterial catheter. Heparinization was continued and the
activated partial thromboplastin time (APTT) was controlled to
twice that of the normal level following surgery. Three to five
days after surgery, 20 mg rt-PA was administered daily via the
microcatheter. The microcatheter and vessel sheath were removed
when the symptoms improved. When the patients were conscious,
warfarin was administered sequentially for one year to adjust the
international normalized ratio between 2.0 and 3.0 and the
provision of heparin was discontinued.
Results
Patients
One patient succumbed to transforaminal herniation
that occurred prior to thrombolysis. Although spontaneous breathing
resumed following decompressive craniectomy, the bilateral pupils
dilated during thrombolysis and surgery was terminated. The other
seven patients recovered well. Consciousness recovered between two
and five days after surgery and muscle strength recovered between
six and ten days following surgery. One patient remained afflicted
with an affective disorder, one patient developed mild diplopia and
one patient developed a fine movement disorder of the upper limbs
upon discharge from the hospital. The modified Rankin Scale scores
improved three months following surgery with six patients having a
score of 0 and one patient having a score of 1. Reexaminations with
MRI and MRV occurred for 3–15 months. The sinuses of five patients
were completely recanalized and the sinuses of two patients were
partially recanalized. Follow-up lasted for 3–24 months and no
recurrence was observed.
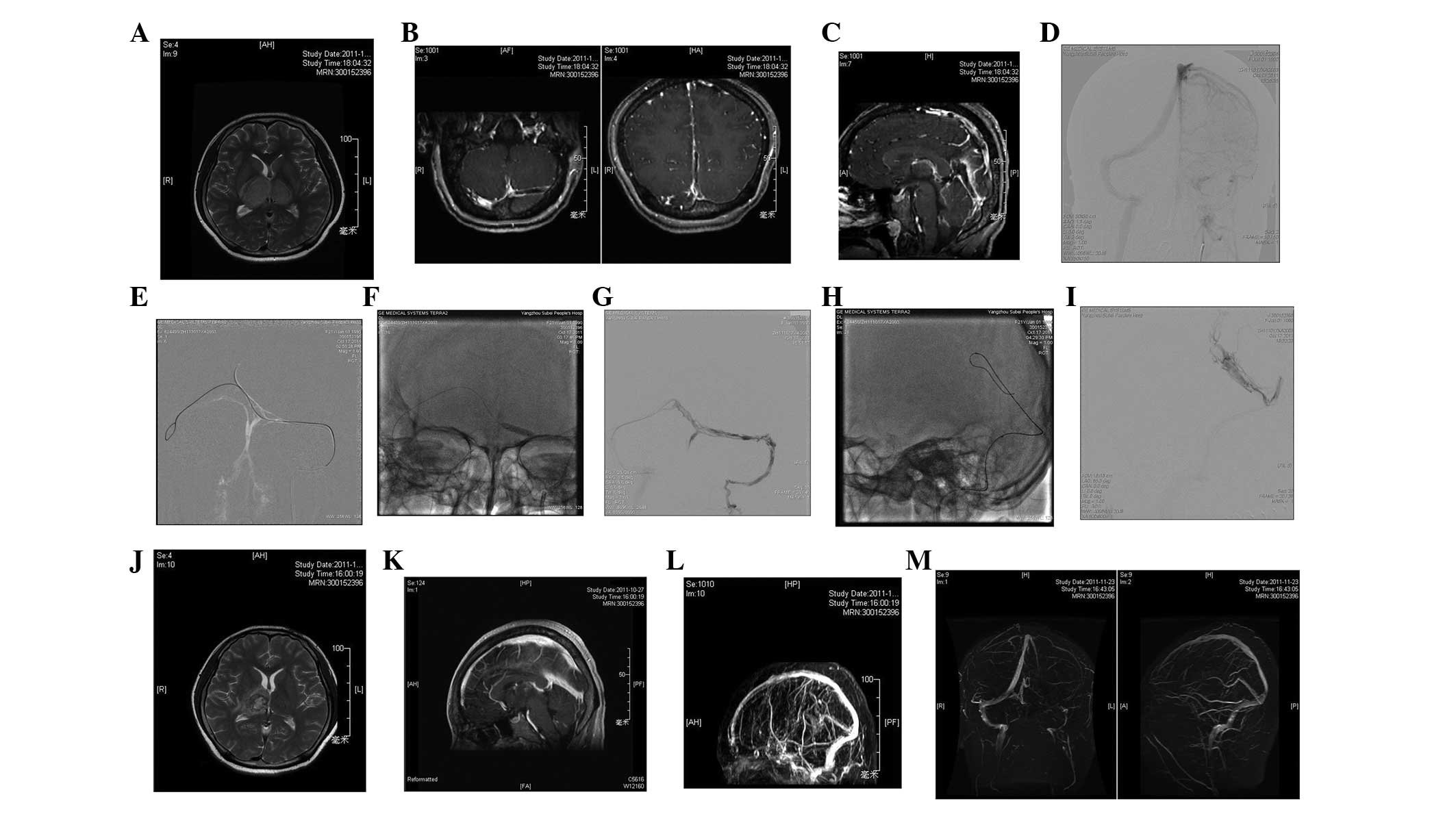
Typical case 1 (female, 47
years-old)
Sudden headache and vomiting occurred 2 days prior
to hospitalization. Heparinization was performed following
admission. However, the disease was progressively aggravated. Minor
epilepsy was observed three times and the GCS score was 9. CT
examination revealed that the left parietal lobe was infarcted and
hemorrhage was identified at the junction of the right temporal and
occipital lobes (Fig. 1A and B).
MRI revealed that thrombi existed in the superior sagittal sinus
and straight sinus (Fig. 1C). In
addition, DSA showed that the superior sagittal sinus and straight
sinus was not phanerous due to thrombosis or congenital dysplasia.
The cortical veins were connected to the sigmoid sinus through the
sylvian vein, cavernous sinus, pterygoid plexus and vein of Labbé
(Fig. 1D). The sacculus expanded
during surgery (Fig. 1E). The
microcatheter was left in the superior sagittal sinus for 3 days
after surgery. On day 2 following surgery, the awareness of the
patient improved significantly, simple verbal exchanges became
possible and right side muscle strength was at level 3, according
to the Oxford Scale. On day 8 following surgery, the patient was
conscious, speech was fluent and muscle strength was at level 5.
DSA revealed that the superior sagittal sinus, straight sinus and
left transverse sinus were well-developed at day 11 following
surgery (Fig. 1F). After one year,
the patient exhibited no neurological deficit and MRV demonstrated
that the superior sagittal sinus and straight sinus had recovered
well (Fig. 1G).
Typical case 2 (female, 21
years-old)
Headache with left limb weakness lasted for 5 days
and unconsciousness lasted for 1 day prior to hospitalization.
Physical examination revealed the GCS score to be 7. The patient
had aphonia and both eyes gazed to the right side. The left
nasolabial fold became shallow and MRI revealed that the bilateral
thalami were infarcted, particularly on the right side (Fig. 2A). Enhanced imaging showed that
thrombi existed in the straight sinus, left transverse sinus and
superior sagittal sinus (Fig. 2B and
C). DSA revealed that the left transverse sinus and straight
sinus did not develop (Fig. 2D).
The microcatheter was placed in the straight sinus via the left
transverse sinus and the sacculus expanded during surgery (Fig. 2E–H). Awareness improved at day 2
following surgery, but the patient developed hypersomnia and
aphasia. At day 3 after surgery, the patient regained consciousness
and was able to have simple verbal exchanges. Left side muscle
strength was at level 3 and right side muscle strength was at level
4. At day 9 following surgery, the patient’s speech was fluent,
right side muscle strength was at level 5 and left side strength
was at level 4+. MRI and MRV examinations at week 2 following
surgery revealed that the disease was in remission and the superior
sagittal sinus and straight sinus had recanalized (Fig. 2I–K). At week 6 after surgery, the
patient’s muscle strength recovered and MRV showed that the
straight sinus had recanalized, whereas the left transverse sinus
was closed (Fig. 2L and M).
Discussion
Although the prognosis of CVST has improved
significantly through the administration of heparin, certain
patients with CVST continue to show poor treatment effects. An
appropriate treatment approach at the right time remains to be
established.
Ideal treatment should aim to prevent further
formation of thrombi, recanalize the venous sinus and establish
collateral circulation. In the present study, symptomatic
treatment, heparinization, thrombolysis and interventional means
were employed. Heparin therapy was provided once intracranial
venous sinus thrombosis had been diagnosed. The efficacy and safety
of unfractionated heparin or low molecular weight heparin for CVST
treatment have already been confirmed by a number of studies and
has been shown to not increase the risk of rebleeding for CVST with
intracranial hemorrhage (3,5,11–15).
The dosage of heparin, which may control the APTT level to twice
that of the normal level, was appropriate. However, antiepileptic,
reduction of intracranial pressure and symptomatic supportive
treatment should also be provided. A previous study of 624 patients
demonstrated that although anticoagulant therapy was provided, 21%
of the patients exhibited a poor prognosis and the mortality rate
was 8.2%. In addition, the coma patients exhibited a mortality rate
of 38% (7). Therefore, if the
effect of heparin treatment is not evident or if symptoms become
aggravated, more active treatment should be considered,
particularly for patients with severe CVST in the following four
situations: i) intracranial hematoma; ii) coma; iii) mental
symptoms; and iv) intracranial deep vein thrombosis (1). Deep vein thrombosis often leads to
rapid deterioration in patient condition. In the present study,
there were six patients whose thrombus involved the straight sinus
and basal vein. Patients with severe CVST required active surgical
intervention. Based on the results of the present study, we
hypothesized that a more active therapeutic approach should be
applied when consciousness disturbance worsens in the first 24-h
after the adoption of intravenous heparinization.
At present, common treatment methods include
intravenous thrombolysis, arterial thrombolysis, local sinus
thrombolysis via a microcatheter, local mechanical thrombectomy in
the venous sinus and sinus stent or a combination of the
aforementioned methods (16–20).
A decompressive craniectomy should be performed on patients with
severe high intracranial pressure and cerebral hernia (21–23).
In the present study, these patients were treated mainly by local
thrombectomy combined with local rt-PA thrombolysis in the sinus
via a microcatheter. The microcatheters were left for continuous
local thrombolysis for 3–5 days after surgery. In the seven
patients that survived, the venous sinuses of five patients were
completely recanalized and those of the two patients that were
partially recanalized, the symptoms improved. The results revealed
that the lesion of severe patients involved multiple venous sinuses
and that treatment should be combined with CT and MRI results
(3,24). The criminal sinus was first
analyzed and mechanical thrombectomy was then performed. A micro
guidewire was passed through the thombosis repeatedly to
mechanically loosen the thrombosis and the sacculus was employed to
expand the thrombus. Microcatheters were then placed in the
thrombus and were pulled back from the distal end during
thrombolysis. Finally, the microcatheters were placed in the
criminal sinus for long-term thrombolysis. Complete recanalization
was not required during surgery due to the long formation time of
venous sinus thrombosis. Heparinization with continuous local
thrombolysis may continue to recanalize the sinus gradually
provided that a blood flow exists in the venous sinus.
Therefore, local thrombectomy combined with local
rt-PA thrombolysis in the sinus via a microcatheter, administered
as early as possible, is a safe and effective method of treatment
for patients with severe CVST. However, this conclusion requires
the support of random double-blind controlled trials with a large
sample size.
References
|
1
|
Agostoni E, Aliprandi A and Longoni M:
Cerebral venous thrombosis. Expert Rev Neurother. 9:553–564. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
van den Bergh WM, van der Schaaf I and van
Gijn J: The spectrum of presentations of venous infarction caused
by deep cerebral vein thrombosis. Neurology. 65:192–196. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bousser MG and Ferro JM: Cerebral venous
thrombosis: an update. Lancet Neurol. 6:162–170. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kimber J: Cerebral venous sinus
thrombosis. QJM. 95:137–142. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Furie KL, Kasner SE, Adams RJ, et al:
Guidelines for the prevention of stroke in patients with stroke or
transient ischemic attack: a guideline for healthcare professionals
from the american heart association/american stroke association.
Stroke. 42:227–276. 2011. View Article : Google Scholar
|
|
6
|
Wasay M, Bakshi R, Bobustuc G, et al:
Cerebral venous thrombosis: analysis of a multicenter cohort from
the United States. J Stroke Cerebrovasc Dis. 17:49–54. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ferro JM, Canhão P, Stam J, Bousser MG and
Barinagarrementeria F; ISCVT Investigators. Prognosis of cerebral
vein and dural sinus thrombosis: results of the International Study
on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke.
35:664–670. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Borhani Haghighi A, Edgell RC, Cruz-Flores
S, et al: Mortality of cerebral venous-sinus thrombosis in a large
national sample. Stroke. 43:262–264. 2012. View Article : Google Scholar
|
|
9
|
Guo XB, Guan S, Fan Y and Song LJ: Local
thrombolysis for severe cerebral venous sinus thrombosis. AJNR Am J
Neuroradiol. 33:1187–1190. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rahman M, Velat GJ, Hoh BL and Mocco J:
Direct thrombolysis for cerebral venous sinus thrombosis. Neurosurg
Focus. 27:E72009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Einhäupl K, Stam J, Bousser MG, et al:
EFNS guideline on the treatment of cerebral venous and sinus
thrombosis in adult patients. Eur J Neurol. 17:1229–1235. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Saposnik G, Barinagarrementeria F, Brown
RD Jr, et al: Diagnosis and management of cerebral venous
thrombosis: a statement for healthcare professionals from the
American Heart Association/American Stroke Association. Stroke.
42:1158–1192. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Einhäupl KM, Villringer A, Meister W, et
al: Heparin treatment in sinus venous thrombosis. Lancet.
338:597–600. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
de Bruijn SF and Stam J: Randomized,
placebo-controlled trial of anticoagulant treatment with
low-molecular-weight heparin for cerebral sinus thrombosis. Stroke.
30:484–488. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Coutinho JM, de Bruijn SF, deVeber G and
Stam J: Anticoagulation for cerebral venous sinus thrombosis.
Stroke. 43:e41–42. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chow K, Gobin YP, Saver J, Kidwell C, Dong
P and Viñuela F: Endovascular treatment of dural sinus thrombosis
with rheolytic thrombectomy and intra-arterial thrombolysis.
Stroke. 31:1420–1425. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Frey JL, Muro GJ, McDougall CG, Dean BL
and Jahnke HK: Cerebral venous thrombosis: combined intrathrombus
rtPA and intravenous heparin. Stroke. 30:489–494. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Smith AG, Cornblath WT and Deveikis JP:
Local thrombolytic therapy in deep cerebral venous thrombosis.
Neurology. 48:1613–1619. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Renowden SA, Oxbury J and Molyneux AJ:
Case report: venous sinus thrombosis: the use of thrombolysis. Clin
Radiol. 52:396–399. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kim SY and Suh JH: Direct endovascular
thrombolytic therapy for dural sinus thrombosis: infusion of
alteplase. AJNR Am J Neuroradiol. 18:639–645. 1997.PubMed/NCBI
|
|
21
|
Théaudin M, Crassard I, Bresson D, et al:
Should decompressive surgery be performed in malignant cerebral
venous thrombosis?: a series of 12 patients. Stroke. 41:727–731.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zuurbier SM, Coutinho JM, Majoie CB, Coert
BA, van den Munckhof P and Stam J: Decompressive hemicraniectomy in
severe cerebral venous thrombosis: a prospective case series. J
Neurol. 259:1099–1105. 2012. View Article : Google Scholar :
|
|
23
|
Ferro JM, Crassard I, Coutinho JM, et al:
Decompressive surgery in cerebrovenous thrombosis: a multicenter
registry and a systematic review of individual patient data.
Stroke. 42:2825–2831. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zubkov AY, McBane RD, Brown RD and
Rabinstein AA: Brain lesions in cerebral venous sinus thrombosis.
Stroke. 40:1509–1511. 2009. View Article : Google Scholar : PubMed/NCBI
|