Introduction
Primary brain tumors have a high incidence rate, and
tumor growth is invasive with an obscure boundary (1). Although brain tumors can be resected
through various treatment methods, including surgery, radiotherapy
and chemotherapy, disease progression is unable to be effectively
controlled. In addition, the prognosis of patients with a brain
tumor is usually poor, with a short survival time and severe
sequelae (2).
Magnetic resonance imaging (MRI)-navigated
argon-helium cryoablation is a new advanced technology. MRI is
known to have good tissue resolution and a multiplanar imaging
capability. In particular, the temperature-sensitive
characteristics of MRI, which enable the clear and real-time
display of the size and range of the ice ball (which destroys the
tumor cells), has resulted in this imaging technique becoming the
focus in clinical cryotherapy against multiple-system tumors, with
satisfactory results previously achieved (3–7).
Although MRI has an unparalleled advantage in nervous system
imaging compared with other methods (8), there are a limited number of domestic
and foreign studies investigating MRI-navigated cryotherapy for the
treatment of brain tumors.
In the present study, a rabbit VX2 brain tumor model
was established that was suitable for MRI imaging and
interventional therapy. The model was used for the preliminary
study of MRI-navigated argon-helium cryoablation therapy against
the brain tumor.
Materials and methods
Animals
In total, 24 New Zealand white rabbits were provided
by the Department of Experimental Animals at the Quality Control
Center of Shandong Lukang Pharmaceutical Group Co., Ltd. (Jining,
China). The rabbits were male or female and weighed between 2.2 and
3.4 kg. A total of 2 of the rabbits succumbed in normal captivity
for unexplained reasons. The study was conducted in strict
accordance with the recommendations in the Guide for the Care and
Use of Laboratory Animals of the National Institutes of Health. In
addition, the animal use protocol was reviewed and approved by the
Institutional Animal Care and Use Committee of Jilin Provincial
People's Hospital (Jilin, China).
Tumor cells
Following resuscitation, the VX2 tumor cells
(presented by Professor Chengli Li of the Shandong Medical Imaging
Research Institute, Jinan, China) were conventionally
adherence-cultivated in RPMI 1640 complete medium, which contained
20% fetal bovine serum, 50 IU/ml penicillin, 50 µg/ml streptomycin
and 300 µg/ml glutamine. Next, logarithmically-growing VX2 tumor
cells were obtained for digestion with 0.25% trypsin. The cell
samples were subsequently centrifuged at 377 × g for 5 min, after
which the supernatant was discarded. Following washing with
Dulbecco's modifed Eagle's medium (DMEM), the precipitate was
diluted with DMEM to form a cell suspension liquid with a
concentration of 1×106. Cell viability was assessed
using a trypan blue assay, and the survival rate of the inoculated
tumor cells was required to be >90%. A 1-ml syringe was used to
transfer 0.5 ml cell suspension liquid into the rabbit bilateral
posterior thigh muscle for subcultivation.
Establishment of the brain tumor
model
Anesthesia was induced using 20 mg ketamine and 0.5
mg midazolam via intramuscular injection (9).
Acquisition of tumor tissue was performed as
follows. The rabbit VX2 solid tumor in the hind legs was resected
under sterile surgical conditions, the outer layer of fat was
removed and the blood was washed away with Hank's solution. Next,
the solid tumor was cut open and the inner rotten porridge-like
necrotic tissues were removed to leave the red-white meat-like
fresh tissue that had a greater peripheral vascular component and
grew vigorously. The tissue was subsequently cut into 1.5-mm
sections with a scalpel, while a sterile gelatin sponge was cut
into 1.5×3 mm-length strips. The tumor blocks and gelatin sponge
strips were then implanted into a 18 G sterile needle (Suzhou Antai
Medical Devices Co., Ltd., Suzhou, China) for future use.
In the cultivation method, the rabbit was firstly
anesthetized and fixed in the prone position. Following the removal
of top hair and disinfection, a 2–3 cm incision was made on the
lateral canthus of the eyes and upwards along the median sagittal
plane. The periosteum was subsequently separated and a 16 G bone
driller (Shenyang Pusiman Medical Instrument Co., Ltd., Shenyang,
China) was applied at a distance 5 mm to the right of the sagittal
suture and 5 mm after the coronal suture. The aforementioned tumor
block prepared in the 18 G puncture needle was punctured through
the hole in the bone into a depth of ∼7 mm. The needle was fixed,
and the needle core was used to implant the tumor block and the
gelatin sponge into the right frontal lobe. The needle was slowly
withdrawn and the hole in the bone was sealed with bone wax.
Finally, the scalp was sutured.
Grouping, treatment and
observation
The brain tumor model was prepared in two stages. In
the first stage, eight rabbits received the brain tumor block
implantation and were subsequently divided into groups A and B,
with four rabbits in each group. Under the guidance of an
interventional MRI System (10,11) (0.3
T open MRI scanner with iPath200 optical tracking guidance system
and foldable multifunctional coil; XinAoMDT Technology Co., Ltd.,
Langfang, China), cryoablation using a CRYO-HITTM argon-helium
knife with MRI compatibility (7)
(1.47 mm probe; Galil Medical, Inc., Jerusalem, Israel) was
performed once the tumor diameter had reached ∼0.8 cm (∼15 days
after the tumor tissue implantation). In group A, two cycles of
argon-helium freezing-heating ablation was performed, with 5 min
freezing and then heating to 40°C in each cycle (12). The group B rabbits also underwent two
cycles of freezing-heating ablation; however, 10 min freezing and
then heating to 40°C was applied in each cycle. The second stage of
tumor model preparation was performed according to the optimal
ablation conditions determined from the first stage. In the second
stage, a total of 14 rabbits underwent brain tumor implantation,
which were divided into groups C and D, with seven rabbits in each
group. MRI scanning was performed 10 days after the tumor block
implantation, followed by five-day interval scanning until the
tumor grew to a diameter of 0.8 cm. Subsequently, the rabbits in
group C underwent argon-helium cryoablation, with the conditions
decided under the optimal condition of the first stage (group B).
Postoperative MRI scanning was performed once a week. The group D
rabbits were used as controls. They did not receive any treatment
and only underwent MRI scanning once every five days. The tumor
volume (mm3) was calculated according to the following
formula (13): V = (4/3 × π × L × W
× H) × 1/8, where L, W and H were the maximum anteroposterior
diameter, width and height, respectively, of the tumor, as measured
by enhanced MRI. Routine enhanced MRI scanning was performed prior
to the sacrifice of the rabbits, after which the tumor specimens
were obtained.
MRI-navigated argon-helium
cryoablation therapy for the VX2 brain tumor
MRI scanning was initiated at day 10 after the
implantation of the VX2 tumor blocks into the New Zealand rabbits,
followed by three-day interval scanning. A total of 0.8 ml/kg
gadolinium (Gd)-diethylene triamine pentaacetic acid (DTPA; Bayer
Schering Pharma AG, Berlin, Germany) was injected through the ear
vein for further observation. When the tumor grew to a diameter of
∼0.8 cm, MRI-navigated argon-helium cryoablation was performed. The
top hair of the rabbits was removed again, after which the rabbits
were anesthetized and fixed on a special-crafted fixer for MRI
interventional pre-scanning. In the pre-scanning images, the tumor
center was set as the target. Following disinfection and sterile
sheet paving, the scalp was re-cut along the last surgical incision
and the periosteum was separated. The argon-helium probe was
inserted through the tumor block implantation hole for
freezing-heating ablation. Intraoperative real-time scanning was
performed to monitor the entire ablation process.
Histopathological examination
Group A and B rabbits underwent MRI scanning at the
following time points: Immediately following ablation and at days 7
and 14 after treatment. After each scanning procedure, one rabbit
from each group underwent left ventricular perfusion with 4%
paraformaldehyde. The rabbit was dissected and the brain tissue was
fixed in 4% formaldehyde solution. After one day, the brain was cut
into 2-3-mm continuous coronal slices for general observations of
the lesion size, shape and edge following ablation. The typical
slice was subsequently embedded in paraffin and stained with
hematoxylin and eosin (HE) to observe the histological changes of
the ablation zone. A similar method was performed to the rabbits in
group D for the collection of general specimens and the
pathological examination of the moribund rabbits. The tumor volume
was calculated according to the following formula: V =
a2 × b/2, in which a represented the long tumor diameter
and b represented the short tumor diameter, with the unit set as
mm3.
Statistical analysis
SPSS 16.0 statistical software (SPSS, Inc., Chicago,
IL, USA) was used for statistical analysis. The counting data were
analyzed using the t-test, while survival analysis was conducted
using Kaplan-Meier survival curves. The log-rank test was used to
assess survival distribution between groups C and D, while
correlation analysis was performed using Pearson's method.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Situation of the tumor
implantation
Among the eight New Zealand white rabbits that
received the tumor block implantation during the first stage, one
rabbit in group A exhibited a brain abscess caused by postoperative
intracranial infection (MRI scan revealed a ring-like enhancement
lesion and the pathological examination confirmed the abscess). An
additional rabbit in group B died as a result of contrast agent
pollution-induced sepsis during the MRI scanning. Thus, there were
six remaining experimental animals. In the second stage of tumor
model assessment, MRI scanning revealed that a tumor had grown in
the 14 rabbits. The overall rate of tumorigenicity was 90.91%, and
the follow-up MRI scanning revealed that none of the tumors
exhibited spontaneous shrinkage or disappearance.
MRI results
At day 10 following the tumor block implantation,
the lesions were observed to be round or oval, with a maximum
average diameter of 4.4±1.1 mm. The T1-weighted images (WIs)
exhibited a slightly lower or equal signal, while the T2WI and
fluid-attenuated inversion recovery (FLAIR) scans exhibited a
slightly hyperintense signal with clear edges and without evident
peripheral edema. Following an injection of gadolinium (Gd)-DTPA,
the scanning results revealed that the tumor exhibited marked
homogeneous enhancement. When the tumor was >1.2 cm, the lesion
center exhibited necrosis, and the T1WI and T2WI revealed a
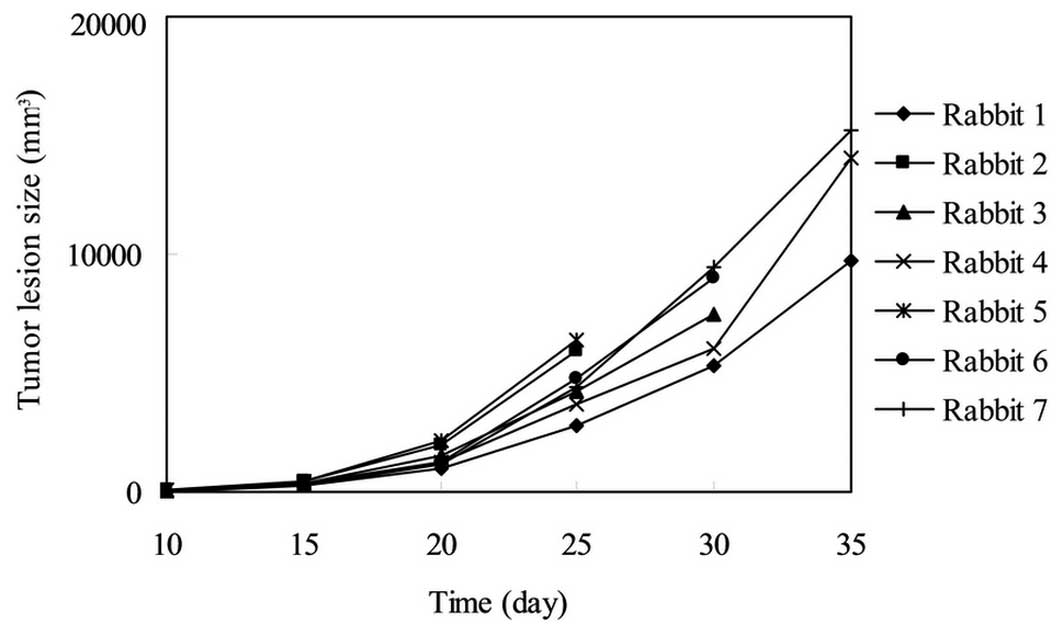
centered low signal. The association between the tumor lesion size
and the various time points of MRI scanning in the rabbits from
group D was analyzed, as shown in Table
I and Fig. 1.
 | Table I.Association between the tumor lesion
size (mm3) and the time point of magnetic resonance
imaging scanning in the group D rabbits. |
Table I.
Association between the tumor lesion
size (mm3) and the time point of magnetic resonance
imaging scanning in the group D rabbits.
| Rabbit | Day 10 | Day 15 | Day 20 | Day 25 | Day 30 | Day 35 |
|---|
| No. 1 | 39.56 | 298.68 |
991.85 | 2755.18 | 5326.40 | 9731.16 |
| No. 2 | 57.48 | 405.70 | 1972.54 | 5902.11 | |
| No. 3 | 44.83 | 349.74 | 1545.77 | 4217.93 | 7485.54 |
|
| No. 4 | 45.68 | 320.14 | 1236.81 | 3704.25 | 5993.47 | 14038.98 |
| No. 5 | 47.37 | 450.79 | 2200.32 | 6418.57 |
|
|
| No. 6 | 40.94 | 302.15 | 1243.08 | 4767.54 | 8994.66 |
|
| No. 7 | 45.35 | 311.43 | 1194.93 | 4438.19 | 9447.08 | 15249.82 |
During MRI-navigated and monitored cryoablation, the
ice ball was exhibited as an oval-shaped signal deletion region
with a clear boundary in all the imaging scans. Following
cryoablation, the group B rabbits exhibited more typical MRI scan
evolutions. On postoperative day 7, the ablation zone in the T1WI
exhibited an equal signal, with a diameter slightly larger compared
with the previous measurement, which was surrounded by a ring-like
enhancement. The ablation zone in the T2WI exhibited an
inhomogeneous hyperintense signal, which was surrounded by an
incomplete hypointensity hemosiderin ring. The outer edge of the
hemosiderin ring exhibited irregular flaky edema. At day 14 after
the ablation, the ablation zone in the T1WI continued to show an
equal signal surrounded by a homogeneous enhancement ring, while
the diameter had decreased to almost to the size of the ice ball.
The ablation zone in the T2WI revealed a homogeneous hyperintense
signal, surrounded by a uniform-thickness isointensity ring, and
the peripheral edema had almost disappeared. The ablation zones in
the T1WI and T2WI from the rabbits in group A on postoperative days
7 and 14 all showed heterogeneous signals, while the peripheral
ring shadow was irregular and continuous.
General specimen and pathological
results
General morphological observations revealed the
rabbit brain VX2 tumors were round, without an envelope and a
slightly blurred boundary contour. In addition, the incisal surface
was pale red to dark red. The HE staining results revealed that the
tumor cells grew actively, were arranged densely and were palisade
or coral-like shaped. The boundary between the tumor and normal
tissues exhibited infiltration of tumor cells towards the adjacent
brain parenchyma; therefore, the boundary exhibited a certain
degree of blurring. The blood vessels were rich within the tumor,
with small flaky necrosis observed occasionally in the center. The
tumor volumes calculated from the MRI scanning of the group D
rabbits are shown in Table II.
 | Table II.Tumor volume calculations
(mm3) from MRI scanning and the general pathological
volume of the tumors in the group D rabbits. |
Table II.
Tumor volume calculations
(mm3) from MRI scanning and the general pathological
volume of the tumors in the group D rabbits.
| Measurement
volume | No. 1 | No. 2 | No. 3 | No. 4 | No. 5 | No. 6 | No. 7 |
|---|
| MRI | 11045.7 | 6532.3 | 8420.7 | 14039.0 | 6419.0 | 10194.3 | 15249.8 |
| General specimen | 10011.4 | 5896.9 | 7537.3 | 12430.8 | 5792.4 |
8978.6 | 12243.7 |
The data revealed that the volumes calculated from
the general specimen measurement were slightly less compared with
volume calculated from MRI scanning. However, the paired t-test
revealed that there was no statistically significant difference
between the two measurement protocols (t=4.094; P=0.006). Pearson's
correlation analysis revealed that the aforementioned two exhibited
a significant correlation (r=0.99; P<0.01).
Brain samples from the rabbits, obtained from the
immediate sacrifice following cryoablation, revealed that the
ablation zone was clear, with a sharp dark brown edge. In addition,
pathological examination revealed that the tumor cells in the brain
specimens from the group A rabbits exhibited slight swelling when
compared with the surrounding normal nerve cells; however, the
changes were not significant. The majority of tumor cells in the
group B rabbits were markedly swollen, and a few tumor cells had
ruptured. On days 7 and 14, pathological examinations revealed that
the ablation zone of the group B rabbits exhibited pale amorphous
necrotic tissue, surrounded by cellular edema and inflammatory cell
infiltration. The new capillaries were rich, and the glial cells
had undergone proliferation. The pathological performance of the
group A rabbits was not as typical as those in group B. Living
tumor cells existed near the edema zone, with neovascularization
and inflammatory cell infiltration observed among the tumor cells.
The range of coagulation necrosis exhibited by pathology was
consistent with that demonstrated in MRI-navigated
cryoablation.
Survival analysis
Rabbits in group D exhibited appetite loss, mental
malaise and lethargy, with the activity levels reducing by day 18
after the brain tumor was implanted. In addition, the rabbits
gradually lost weight by day 21, and at day 25, the rabbits
presented with symptoms of lateral limb paralysis or the body
exhibited tetanic bending towards the contralateral side.
Furthermore, the rabbits were restless, anxious and showed a number
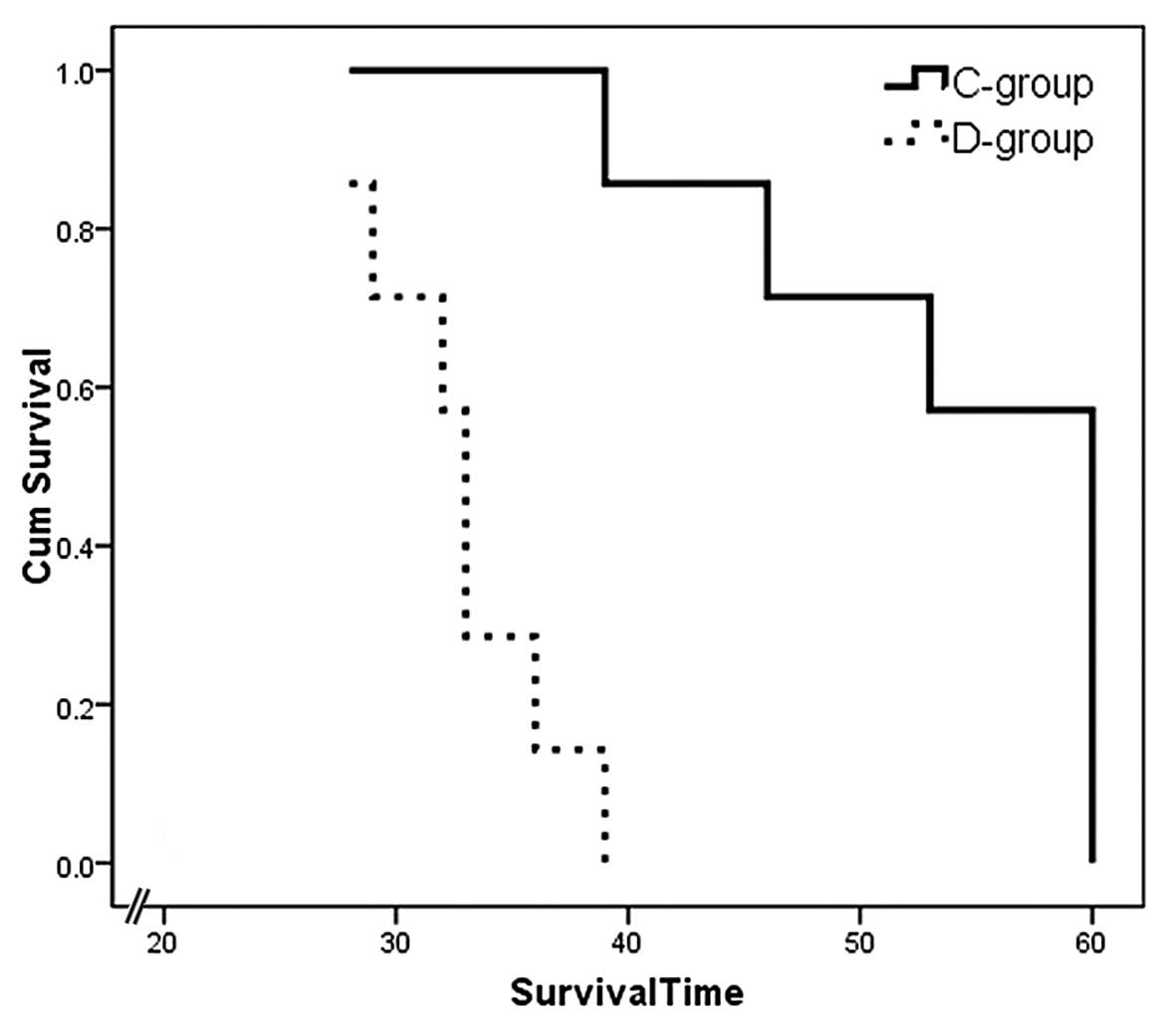
of signs of aggression. The average survival time of the rabbits
was 32.86±3.80 days (Fig. 2).
The seven rabbits in group C all successfully
underwent cryoablation therapy. Following surgery, two rabbits
exhibited mild hemiparesis and one rabbit had right-eye
conjunctival hyperemia. Furthermore, three rabbits died on
postoperative days 39, 46 and 53. The remaining rabbits were
observed for 60 days to obtain censored data (Table III).
 | Table III.Comparison of the survival times of
the rabbits in groups C and D (days). |
Table III.
Comparison of the survival times of
the rabbits in groups C and D (days).
| Group | No. 1 | No. 2 | No. 3 | No. 4 | No. 5 | No. 6 | No. 7 |
|---|
| C | 60a | 53 | 60a | 39 | 46 | 60a | 60a |
| D | 39 | 28 | 33 | 36 | 29 | 33 | 32 |
The Kaplan-Meier survival curve method was used to
statistically analyze the survival times of the rabbits. The
results revealed that the survival times of the rabbits in group C
were significantly longer compared with the rabbits in group D,
with the difference statistically significant (P<0.05). The
survival function graph is shown in Fig.
2.
Discussion
Establishing animal tumor models has important
significance towards understanding the mechanisms underlying
tumorigenesis, tumor development, tumor prevention and treatment.
Rabbit VX2 cancer models of the liver, kidney, lung and bone have
been studied maturely, and have been widely applied for use in
tumor imaging, physiological and pathological studies, as well as
in the efficacy evaluation of interventional treatment (14). However, VX2 brain tumor animal models
have been rarely used in domestic and foreign studies, and the
tumor implantation method used is primarily the intracerebral
injection of tumor cell suspension (15,16). At
the start of the present study, a number of other methods had been
attempted; however, various shortcomings were observed. Firstly,
the concentration and amount of the injected tumor cells was not
easy to control. Secondly, tumor growth was more diffuse, with the
tumors growing along the needle tract. Thus, the meninges were
invaded earlier, which was associated with bleeding inside the
needle tract, causing the tumor cells to be flushed out. Finally,
the tumor size and shape were found to differ substantially between
models.
Based on the results of a previous study, the model
preparation method was improved (15). Firstly, the cell suspension was
replaced with a tumor block for implantation, as the block size can
be more easily quantified compared with the tumor cells. Secondly,
when the tumor block was implanted, a gelatin sponge was also
implanted into the needle tract, which prevented the tumor block
being flushed out or displaced due to the bleeding of the needle
tract. Furthermore, using a gelatin sponge guaranteed that the
tumor block was able to be fully implanted into the brain rather
than residing inside the needle, ensuring the success of the tumor
block implantation. Finally, following the implantation of the
tumor block, the needle was kept in position for 3–5 min, after
which it was slowly pulled out to reduce the bleeding and other
complications. In total, three rabbits out of the originally
prepared eight models, were randomly selected for immediate
postoperative MR scanning. The results revealed that the needle
tract exhibited minor bleeding; however, there were no
postoperative abnormal symptoms and signs, and no rabbit died
during the tumor block implantation, which demonstrated the safety
of the tumor block implantation method using the puncture
needle.
On postoperative day 10, normal and enhanced MRI
scanning was performed in each rabbit. With the exception of one
rabbit that exhibited abscess formation and presented with slight
ring enhancement (reason to be discussed), the remaining rabbits
exhibited tumor growth formation in the brain, with a tumor
formation rate of 90.91%. On postoperative day 10, the average
maximum cross-sectional diameter of the tumors was 4.4±1.1 mm. The
tumor sizes were predominantly uniform and the tumors were
regularly shaped, appearing as round or oval. These observations
demonstrate the successful establishment of the tumor model, which
may have significance in future experimental cancer research.
In a previous study (17), with regard to the MRI scans, the
tumors in the T1WI showed a slightly lower or equal signal, while
the tumors in the T2WI and FLAIR scans exhibited a slightly
hyperintense signal, with a clear edge and no surrounding edema.
Following the injection of Gd-DTPA, the signals all showed a
significant enhancement. When the tumor diameter is >1.2 cm, the
center of the tumor may exhibit necrosis (18). The general observations of the VX2
brain tumor specimens demonstrated consistency with the imaging
features, with only the volume slightly reduced compared with that
in the radiographic observations. This difference may have been
caused by the following two reasons. Firstly, due to the partial
volume effect, the MRI scans may exhibit a slightly larger tumor
diameter. Secondly, during the sampling, the 4% formaldehyde
perfusion fixation may cause a reduction in the lesion volume.
Tacke et al (18) considered
that after fixation, the median size of the specimen was 1.14 times
less compared with the measurement prior to fixation. Pathological
examination revealed that cell division was exuberant, and the
cells had slightly invaded towards the normal tissues. Furthermore,
angiogenesis was shown to be rich. With regard to imaging
observations, these pathological features primarily present as a
less clear boundary and marked enhancement of the tumor.
Hypothermia is known to significantly extend the
relaxation time in T1WIs, while decreasing the time in T2WIs. Thus,
when performing cryoablation, the ice ball may appear as a
sharp-edged hypointense signal in all MRI scanning sequences, which
is conducive to the real-time display of the ice ball formation in
MRI (19). According to the
comparative study of pathology and MRI in the group B rabbits, the
ice ball size and the tissue necrosis scope were consistent.
MRI has a temperature-sensitive characteristic,
which can be used as a great advantage towards monitoring the
temperature and range of the ablation zone during cryoablation of
the brain tumor (12). The
argon-helium knife used in the present study was a new ultra-low
temperature freezing-heating therapeutic piece of equipment, which
used high-pressure argon and helium as the freezing and heating
medium, respectively, with the freezing principle conducted
according to the Joule-Thomson effect (18). The superconductive knife was a hollow
tubular probe, with the thinnest diameter of 1.47 mm. While the
knife was able to export the high-pressure argon at room
temperature (the freezing medium) or helium (the heating medium),
the thermocouple was mounted directly on the probe tip in order for
the temperature to be continuously monitored. During the surgery,
the high-pressure normal-temperature argon was firstly exported
from the probe tip, causing the target tissue temperature to
rapidly decrease to below −140°C in 10–20 sec (argon freezing is
able to reach a lowest temperature of −185°C). Subsequently,
assisted by the rapid expansion of helium at the probe tip, the
probe was rapidly heated to 30–50°C to completely destroy the tumor
cells (20). Since the freezing and
heating was limited to an inside range of 2 cm from the
superconductive cryosurgical probe tip, the needle bar had good
thermal insulation to prevent the occurrence of large damage to the
tissues on the puncture path.
Certain experiments have confirmed that through
using an intracranial glioma model, argon-helium cryoablation
therapy not only causes the necrosis of glioma cells that are in
the central area of the freezing zone, but also induces the
apoptosis of the surrounding tumor cells (19). In addition, the in situ dead
tumor tissues following cryoablation may become antigens, promoting
the anti-tumor immune response of the body (18), which highlights the advantages of
using argon-helium cryoablation therapy.
MRI-navigated interventional therapy is the perfect
combination of the latest imaging technology and minimally invasive
surgery, possessing incomparable advantages over X-ray, CT and
B-mode ultrasound. For example, MRI utilizes multi-parameter
imaging that exhibits high resolution towards the soft tissues,
enabling observations of lesions that other imaging methods are
unable to reveal. Furthermore, MRI has characteristics of arbitrary
planar imaging and temperature-sensitive imaging. In addition, MRI
is a form of functional imaging that uses safer contrast agents and
produces no ionizing radiation. The open magnet ensures that the
surgical procedure is more convenient. The navigation equipment and
the dedicated rapid imaging sequences enable real-time guidance and
monitoring throughout the operation. In addition, the flexible
multi-functional coil can be placed onto any appropriate area to
satisfy the surgical requests; thus, the image quality of the
surgical area is improved.
Argon-helium cryoablation was performed when the
rabbit VX2 brain tumor reached a diameter of 0.8 cm for the
following reasons. Firstly, an excessively small tumor diameter is
not conducive to the intraoperative identification of the tumor.
Secondly, the size of the ice ball is difficult to control to
within 1 cm, and if the tumor is too small, increased damage may be
caused towards the surrounding normal tissues. Finally, if the
tumor is too large, the tumor-bearing rabbit can often exhibit
anorexia and decreasing physical activity; therefore, tolerance
towards the surgery decreases. During the process of VX2 brain
tumor cryoablation, real-time dynamic scanning can be performed to
observe the formation of the ice ball. The size of ice ball is
largest after 4 min, where the diameter is 1.0 cm and completely
covers the lesion and slightly beyond the edge of the lesion. In
the second cycle, the ice ball size slightly increases, reaching a
diameter of 1.2 cm. This may be the result of vascular damage or
thrombosis formed in the ablation zone during the first cycle;
thus, in the second cycle, the energy lost during the ablation
reduces (21).
The average survival time of the rabbits in group D
was 33±4.3 days. When comparing the survival times between the
rabbits in groups C and D, a statistically significant difference
(P<0.05) was observed. This result indicated that the
argon-helium cryoablation therapy played a role in inactivating the
tumor tissues, and thus, significantly improved the survival times
of the tumor-bearing rabbits.
In conclusion, the present preliminary study
demonstrated that the puncture needle method may be used to obtain
a high success rate in the preparation of a VX2 brain tumor model.
The reproducibility was good, and the tumorigenicity was uniform,
safe and feasible; therefore, this method was determined to be
suitable for the requirements of pathology, imaging and
interventional treatment. In addition, MRI-navigated and real-time
monitored argon-helium cryoablation therapy was shown to be an
accurate, safe and feasible technique, with minimal invasion, for
the treatment of brain tumors. The technique was found to
significantly increase the survival times of the tumor-bearing
rabbits, while exhibiting little effect and sequelae on the
surrounding normal tissues.
References
|
1
|
Katchy KC, Alexander S, Al-Nashmi NM and
Al-Ramadan A: Epidemiology of primary brain tumors in childhood and
adolescence in Kuwait. Springerplus. 2:582013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ziegler DS, Cohn RJ, McCowage G, et al:
Efficacy of vincristine and etoposide with escalating
cyclophosphamide in poor-prognosis pediatric brain tumors. Neuro
Oncol. 8:53–59. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lehotska V, Tothova L and Valkovic L: The
role of dynamic contrast-enhanced MRI in differentiation of local
recurrence and residual soft-tissue tumor versus post-treatment
changes. Bratisl Lek Listy. 114:88–92. 2013.PubMed/NCBI
|
|
4
|
Liu JG, Chen FL, Ge CL, Gong MY, Zuo HB
and Zhang JR: Cryosurgery for treatment of subcutaneously
xenotransplanted tumors in rats and its effect on cellular
immunity. Technol Cancer Res Treat. 10:339–346. 2011.PubMed/NCBI
|
|
5
|
Yang Y, Wang C, Lu Y, et al: Outcomes of
ultrasound-guided percutaneous argon-helium cryoablation of
hepatocellular carcinoma. J Hepatobiliary Pancreat Sci. 19:674–684.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Vasil'ev SA, Pesnia-Prasolov SB, Krylov
VV, et al: Cryodestruction in neurosurgery. Khirurgiia (Mosk).
2:105–108. 2013.[(In Russian)]. PubMed/NCBI
|
|
7
|
Bomers JG, Yakar D, Overduin CG, et al: MR
imaging-guided focal cryoablation in patients with recurrent
prostate cancer. Radiology. 268:451–460. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jaskólski DJ, Fortuniak J, Majos A, et al:
Magnetic resonance spectroscopy in intracranial tumours of glial
origin. Neurol Neurochir Pol. 47:438–449. 2013.PubMed/NCBI
|
|
9
|
Sun CJ, Li C, Yu JM, et al: Comparison of
64-slice CT perfusion imaging with contrast-enhanced CT for
evaluating the target volume for three-dimensional conformal
radiotherapy in the rabbit VX 2 brain tumor model. J Radiat Res.
53:454–461. 2012.PubMed/NCBI
|
|
10
|
Bahn D, de Castro Abreu AL, Gill IS, et
al: Focal cryotherapy for clinically unilateral low-intermediate
risk prostate cancer in 73 men with a median follow-up of 3.7
years. Eur Urol. 62:55–63. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gangi A, Tsoumakidou G, Abdelli O, et al:
Percutaneous MR-guided cryoablation of prostate cancer: initial
experience. Eur Radiol. 22:1829–1835. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Anayama T, Nakajima T, Dunne M, et al: A
novel minimally invasive technique to create a rabbit vX2 lung
tumor model for nano-sized image contrast and interventional
studies. PLoS One. 8:e673552013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
He Y, Tu HJ, Lei Z, et al: Experimental
study of apoptosis in C6 rat glioma model induced by cryotherapy.
Zhonghua Zhong Liu Fang Zhi Za Zhi. 12:1615–1618. 2005.[(In
Chinese)].
|
|
14
|
Song J, Li C, Wu L, et al: MRI-guided
brain tumor cryoablation in a rabbit model. J Magn Reson Imaging.
29:545–551. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mei LJ, Yang XJ, Tang L, Hassan AH,
Yonemura Y and Li Y: Establishment and identification of a rabbit
model of peritoneal carcinomatosis from gastric cancer. BMC Cancer.
10:1242010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Handal JA, Schulz JF, Florez GB, Kwok SC,
Khurana JS and Samuel SP: Creation of rabbit bone and soft tissue
tumor using cultured VX2 cells. J Surg Res. 179:e127–e132. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Anderson JK, Shingleton WB and Cadeddu JA:
Imaging associated with percutaneous and intraoperative management
of renal tumors. Urol Clin North Am. 33:339–352. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tacke J, Speetzen R, Adam G, et al:
Experimental MR imaging-guided interstitial cryotherapy of the
brain. AJNR Am J Neuroradiol. 22:431–440. 2001.PubMed/NCBI
|
|
19
|
Hu KW, Li QW, Zuo MH, Sun T and Jiang M:
Clinical observation on the combined treatment of 57 cases of
non-small cell lung cancer using argon-helium cryosurgery and C
hinese herbal medicine. Chin J Integr Med. 13:224–227. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mack MG and Vogl TJ: MR-guided ablation of
head and neck tumors. Neuroimaging Clin N Am. 14:853–859. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Xiao H, Liao Q, Cheng M, et al:
5-Amino-4-oxopentanoic acid photodynamic diagnosis guided
microsurgery and photodynamic therapy on VX 2 brain tumour
implanted in a rabbit model. Chin Med J (Engl). 122:1316–1321.
2009.PubMed/NCBI
|