Introduction
The formation of bone in the embryo and during adult
fracture repair and remodeling involves the progeny of cells known
as mesenchymal stem cells (MSCs). These cells continuously undergo
self-replication, while a number become committed to mesenchymal
cell lineages, such as bone, cartilage, tendon, ligament and
muscle. The differentiation of these cells within each of the
mesenchymal cell lineages is a complex multistep pathway that
involves discrete cellular transitions and is similar to that which
occurs during hematopoiesis. The progression of the cells between
stages depends on the presence of specific bioactive factors,
nutrients and other environmental cues, which coordinate to elicit
the entire differentiation process (1). MSCs have self-renewal capacity without
differentiation in long-term culture. Under certain conditions,
MSCs can differentiate into adipocytes, chondrocytes, astrocytes,
tenocytes, cardiomyocytes, hepatocytes, neurons and muscle,
endothelial and endodermal cells (2)
MSCs have generated considerable attention and shown promise as a
potential source of cells for cell-based therapeutic strategies,
primarily owing to their intrinsic ability to self-renew and
differentiate into functional cell types that constitute the tissue
in which they exist. MSCs are considered a readily accepted source
of stem cells, since such cells have already demonstrated efficacy
in multiple types of cellular therapeutic strategies, including
applications in treating children with osteogenesis imperfecta
(3), hematopoietic recovery
(4) and tissue regeneration
strategies (5). An osteoblast is a
bone-forming cell that arises from MSCs. These cells are known to
exist in the periosteum and bone marrow, but their population is
extremely small. Culture-expanded MSCs have the in vitro
capacity to differentiate into osteoblasts and, notably, the
cultured osteoblast can form extracellular matrix in culture
(6).
Despite the significant interest in MSCs, there
remains no established protocol for the isolation and expansion of
the cells in culture. In the majority of experiments, isolated MSCs
from bone marrow mononuclear cells (MNCs) were determined based on
their tight adherence to tissue culture plastic (7,8). These
isolated cells were initially heterogeneous, and difficult to
distinguish from other adherent cells. None of the several methods
that have been developed to prepare more homogenous populations
(7) have thus far earned wide
acceptance. In the present study we aimed to slightly modify the
method by Friedenstein et al (8) and successfully differentiate MSCs into
bone cells. Several types of materials, including allograft,
xenograft and synthetic biomaterials, are currently used for bone
replacement therapy, but the future of bone reconstruction lies in
the use of stem cells for bone development. The aim of the present
study was to analyze the rapid growth and osteogenic
differentiation of MSCs isolated from human bone marrow.
Materials and methods
Bone marrow MSC isolation and primary
culture
Human bone marrow was obtained with the informed
consent of patients at the Hospital Universiti Sains Malaysia
(Kubang Kerian, Malaysia). The marrow material was aspirated from
the iliac crest and collected in a 50-ml centrifuge tube containing
citrate phosphate buffer (pH 7; Sigma-Aldrich, St. Louis, MO, USA)
with anticoagulant and processed within 15 h of collection. The
bone marrow was flushed with the primary culture media, which
contained Dulbecco's Modified Eagle's Medium (DMEM; Gibco-BRL,
Grand Island, NY, USA), 10% fetal bovine serum (FBS; HyClone,
Logan, UT, USA) and 2% antibiotics (100 U/ml penicillin and 100
U/ml streptomycin). Nucleated cells were collected by density
gradient centrifugation onto a Percoll solution (density, 1.073
g/ml; Sigma-Aldrich). The cells were seeded into a 50-ml cell
culture flask and incubated at 37°C in 5% CO2. The media
was first replaced after 48 h when the cells reached confluence and
subsequently twice a week. Continuous passage was performed in
order to harvest relatively pure MSCs. The present study was
approved by the Institutional Ethical Committee of the Universiti
Putra Malaysia (Serdang, Malaysia).
Characterization of bone marrow
MSCs
The third-passage MSCs were characterized with
respect to the expression of surface antigens. The cells were
seeded at 3.1×103/ml in two-well chamber slides in 1 ml
MSC growth medium until cells became confluent. The cells grown on
slides were fixed with 4% formaldehyde for 30 min and then
incubated in 1 ml 1:5 diluted mouse anti-human cluster of
differentiation 105 (CD 105; DakoCytomation, Glostrup, Denmark).
The cells were subsequently rinsed gently with Tris buffered saline
(TBS) and replaced in fresh TBS. Sufficient link solution
(biotinylated anti-rabbit, anti-mouse and anti-goat immunoglobulins
in phosphate-buffered saline containing stabilizing protein and
0.015 mol/l sodium azide; DakoCytomation, Glostrup, Denmark) was
applied to cover the cells, which were incubated for 15 min. The
cells were rinsed with TBS and streptavidin-alkaline phosphatase
(ALP) solution was applied to cover the cells, which were incubated
for a further 10 min. Following this time period, the cells were
counterstained with hematoxylin for 1 min and observed under the
microscope (Eclipse Ti, Nikon, Melville, NY, USA). The positive MSC
lines were obtained from the American Type Culture Collection
(Rockville, MD, USA) and used as a positive control. For the
negative control, the MSCs were not incubated with CD 105.
Cell seeding and culture in vitro
MSC cultures were seeded into a culture plate at a
density of 3.1×103/ml. Subsequent to adding the cell
suspension with osteogenic differentiation media (DMEM supplemented
with 10% FBS, 10 mm β-glycerol phosphate, 0.1 µM dexamethasone and
100 µM ascorbate-2-phosphate) to the cell culture plate, the plates
were incubated for 4 h for cell attachment. The media was removed
and the adherent cells were cultured in fresh osteogenic medium at
37°C in 5% CO2 for three weeks in vitro. The
culture media were replaced twice a week.
Osteogenic differentiation of
MSCs
ALP assay
ALP is a vital marker enzyme of the early stages of
osteogenic differentiation. After one week of osteogenic
differentiation culture, the plate was placed at −70°C for 20 min
and then was transferred to a 37°C room for 15 min to lyse the cell
membranes. Serial dilution of p-nitrophenol standard was
prepared at the concentration of 3.125 µg/ml (Table I) and a volume of 100 ml was
distributed into the appropriate wells. A total of 50 µl substrate
solution was added to all sample wells, and the plate was covered
and mixed well for 2 min on the Titertek Plate Shaker
(Titertek-Berthold, Pforzheim, Germany). Absorbance was read
immediately at 405 nm with a reference wavelength of 630 nm on the
ELISA Reader (Sunrise™; Tecan Group Ltd., Mannedorf,
Switzerland).
 | Table I.Serial dilution of
p-nitrophenol standard (200 µg/ml) for concentrations of
0–200 µg/ml. |
Table I.
Serial dilution of
p-nitrophenol standard (200 µg/ml) for concentrations of
0–200 µg/ml.
| Serial dilution
standard p-nitrophenol | Volume of 200 µg/ml
solution (µl) | Volume of distilled
water (µl) | Concentration
(µg/ml) |
|---|
| A |
0.000 | 200.0 |
0.000 |
| B |
3.125 | 196.9 |
3.125 |
| C |
6.250 | 193.8 |
6.250 |
| D |
12.500 | 187.5 |
12.500 |
| E |
25.000 | 175.0 |
25.000 |
| F |
50.000 | 150.0 |
50.000 |
| G | 100.000 | 100.0 | 100.000 |
| H | 200.000 |
0.0 | 200.000 |
Matrix mineralization staining
Von Kossa staining was used to identify the matrix
mineralization after three weeks in osteogenic induction culture.
In brief, 1 ml 5% silver nitrate was added to the culture plate and
the cells were exposed to 100 W lamp light for 60 min. The slide
was rinsed and placed in 0.5% hydroquinone for 2 min and then
washed with distilled water. A total of 1 ml 5% sodium thiosulfate
solution was added for 2 min and rinsed with distilled water. The
slide was stained with Biebrich Scarlet-Acid Fuchsin and observed
under the microscope for mineralized extracellular matrix.
Statistical analysis
All experimental analyses were performed in
triplicate (n=3). Data are expressed as the mean ± standard
deviation. P<0.05 was considered to indicate a statistically
significant difference.
Results and Discussion
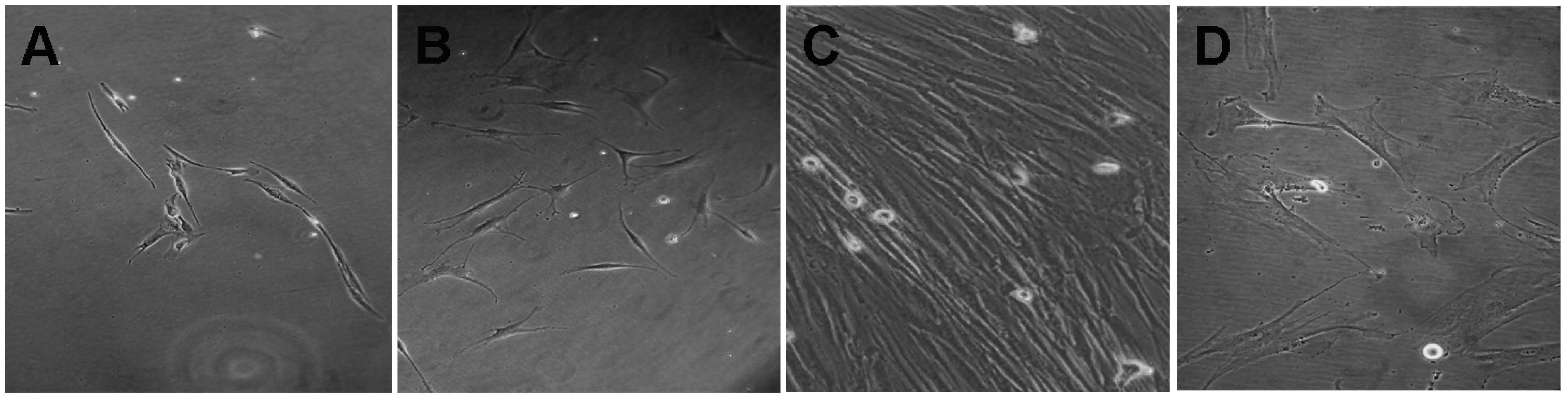
Cell adhesion and proliferation
MNC samples obtained from the human bone marrow were
cultured and maintained in MSC growth medium. The morphology of the
MSCs seeded for 24 h is shown in Fig.
1A. The results showed that the MSCs exhibited a
fibroblast-like morphology and could attach well onto the plates.
After 5 days, the adherent cells were composed of bipolar
fibroblast-like cells that could later be grown to confluence in
MSC growth medium (Fig. 1B and C).
An attempt was also made to culture the MNCs in DMEM-10% FBS
medium; however, in contrast to the parallel cultures growing in
MSC growth medium, cells growing in DMEM-10% FBS did not expand or
proliferate (Fig. 1D). Thus, MSC
growth medium successfully supported the in vitro expansion
of MSCs, as indicated by rapid proliferation and the appearance of
large, oval-shaped, fibroblast-like cells.
Characterization of MSCs by
histochemical staining
The use of bone marrow stem cells in gene and cell
therapy requires in vitro expansion and culture conditions
that preserve their differentiation and proliferative potential.
MSC-like cells are fibroblastoid and express a marker protein
typical of MSCs, CD 105. In this study, the cells were analyzed
using histochemical staining with primary antibodies against CD
105, based on the labeled streptavidin-biotin method. The MSC
surface marker reacted with the anti-CD 105 primary antibody,
resulting in a fuchsia stain (Fig.
2). The results showed that CD 105 was positively expressed,
and the purity of the third-passage MSCs was >95%. Subsequent to
cell sorting and expansion, the pure and uniform MSCs were stocked
as seeded cells for further study. The human bone marrow stem
cells, which exhibit a multi-lineage capacity, were differentiated
towards the osteogenic lineages using lineage-specific induction
factors. In the present study, the induction of human bone marrow
MSCs in osteogenic media in the presence of ascorbic acid,
β-glycerol phosphate and dexamethasone showed that the MSCs had a
multi-lineage potential. Dexamethasone is a synthetic
glucocorticoid shown to induce osteogenic differentiation in MSCs,
and β-glycerol phosphate promotes mineralized matrix formation by
acting as a potential source of phosphate ions (9). Ascorbic acid is a cofactor required for
the function of several hydroxylases. It has been shown that
ascorbic acid, together with β-glycerol phosphate and
dexamethasone, induces embryonic stem cells to differentiate into
mineralized osteoblasts in vitro (10).
Biochemical analysis of ALP
ALP activity is one of the most commonly used
markers for osteogenesis, since it reflects the proportion of
osteogenically differentiated cells. ALP activity was determined
from a p-nitrophenol standard curve. Incubation of human
MSCs under the osteogenic condition within one week resulted in a
marked increase in ALP activity. As shown in Fig. 3, increased ALP activity was observed
in human MSC cultures on day 2, with the increase peaking on day 7.
However, the activity then decreased between days 7 and 14. This
may have been a result of the cells reaching confluence earlier due
to rapid proliferation, which may have resulted in earlier
differentiation. Intercellular communication affects the expression
of differentiation markers in osteoblasts (11); therefore, a higher cell density
likely results in a higher degree of cell-cell interaction, and
thus a higher rate of differentiation.
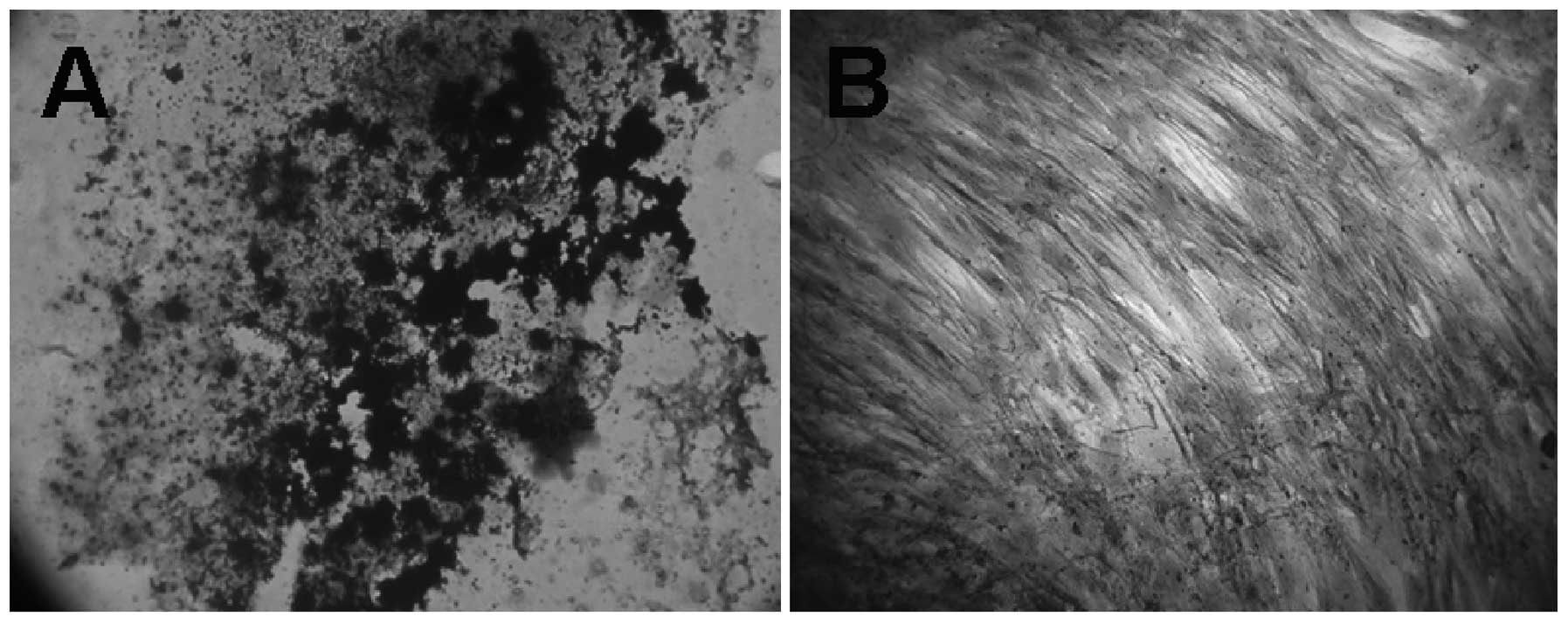
Von Kossa staining of osteogenic
differentiated MSCs
To confirm osteogenic differentiation, calcification
of the matrix was assessed in MSCs using the von Kossa Stain.
Calcification appeared as black regions within the cell monolayer.
Consistent with osteogenesis, several black regions, indicative of
calcified extracellular matrix, red regions, indicative of the
nucleus, and light pink regions, indicative of the cytoplasm, were
observed in human bone marrow stem cells treated for three weeks in
osteogenic medium (Fig. 4A). No
calcification (black region) was observed in the undifferentiated
MSCs (Fig. 4B), although red and
light pink regions, indicative of the nucleus and cytoplasm,
respectively, were observed. The three-week incubation period with
osteogenic-inducing culture medium resulted in an accumulation of
calcium deposits. Monolayer cultures of human bone marrow
MSC-derived osteogenic cells showed a positive reaction to von
Kossa staining, relative to the control monolayer MSC cultures that
were incubated with regular culture medium without the
osteoinductive supplement. Bone marrow has been reported to be the
most established, best-understood and most reliable source of
skeletal stem cells (12,13). These cells have already shown great
regenerative potential. During the 28-day assay period, MSCs
cultured with optimized osteogenic medium underwent a marked change
in cellular morphology. The cultures began to form multilayered
nodular structures, as the apparent result of coalescing cellular
aggregates, and nearly all cells of the nodular structures were
cuboidal, as shown in Fig. 5. The
induction of human MSCs using osteogenic medium was examined. The
results indicated that, in comparison with the MSC growth medium,
MSCs cultured in medium containing osteogenic supplements formed
cell clusters and mineral deposits. The majority of the cells that
attached to the plastic surface exhibited a fibroblast-like spindle
shape. The cells proliferated to form a uniform confluent cell
monolayer and became cuboidal in shape five days after changing
from the MSC growth medium to the osteogenic medium (Fig. 5). The cells began to coalesce between
days 14 and 28. Overall, this study may provide some useful
information on the effect of MSC growth medium and its stimulation
of rapid proliferation and osteogenic differentiation.
Considerable evidence has definitively demonstrated
that MSCs exist in adult tissues or organs. Although the collection
of bone marrow is time consuming and painful, bone marrow has
relatively high numbers of MSCs and has high osteoblast potential.
The modified method utilized in the present study resulted in the
rapid proliferation of MSCs. These findings suggest that this
medium has promising potential for the further analysis of bone
tissue engineering of MSCs. To continue to take advantage of these
cells for cell and gene therapy applications, however, requires a
complete understanding of MSC culture maintenance and how the
differentiation of MSCs is regulated in vivo and in
vitro. Knowledge gained in these areas is likely to facilitate
the design of optimal in vitro conditions that incorporate
regimes targeted towards generating highly functional MSCs for
cell-based clinical application.
References
|
1
|
Price JS, Oyajobi BO and Russell RG: The
cell biology of bone growth. Eur J Clin Nutr. 48:Suppl 1.
S131–S149. 1994.PubMed/NCBI
|
|
2
|
Sanchez-Ramos J, Song S, Cardozo-Pelaez F,
et al: Adult bone marrow stromal cells differentiate into neural
cells in vitro. Exp Neurol. 164:247–256. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Horwitz EM, Gordon PL, Koo WK, et al:
Isolated allogeneic bone marrow-derived mesenchymal cells engraft
and stimulate growth in children with osteogenesis imperfecta:
Implications for cell therapy of bone. Proc Natl Acad Sci USA.
99:8932–8937. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Koç ON, Gerson SL, Cooper BW, et al: Rapid
hematopoietic recovery after coinfusion of autologous-blood stem
cells and culture-expanded marrow mesenchymal stem cells in
advanced breast cancer patient receiving high-dose chemotherapy. J
Clin Oncol. 18:307–316. 2000.PubMed/NCBI
|
|
5
|
Petite H, Viateau V, Bensaïd W, et al:
Tissue-engineered bone regeneration. Nat Biotechnol. 18:959–963.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ohgushi H, Miyake J and Tateishi T:
Mesenchymal stem cells and bioceramics: strategies to regenerate
the skeleton. Novartis Found Symp. 249:118–127. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hung SC, Chen NJ, Hsieh SL, et al:
Isolation and characterization of size-sieved stem cells from human
bone marrow. Stem Cells. 20:249–258. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Friedenstein AJ, Latzinik NW, Grosheva AG
and Gorskaya UF: Marrow microenvironment transfer by heterotopic
transplantation of freshly isolated and cultured cells in porous
sponges. Exp Hematol. 10:217–227. 1982.PubMed/NCBI
|
|
9
|
Shin H, Temenoff JS, Bowden GC, et al:
Osteogenic differentiation of rat bone marrow stromal cells
cultured on Arg-Gly-Asp modified hydrogels without dexamethasone
and beta-glycerol phosphate. Biomaterials. 26:3645–3654. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Carinci F, Pezzetti F, Spina AM, et al:
Effect of Vitamin C on pre-osteoblast gene expression. Arch Oral
Biol. 50:481–496. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Li Z, Zhou Z, Yellowley CE and Donahue HJ:
Inhibiting gap junctional intercellular communication alters
expression of differentiation markers in osteoblastic cells. Bone.
25:661–666. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Minguell JJ, Erices A and Conget P:
Mesenchymal stem cells. Exp Biol Med (Maywood). 226:507–520.
2001.PubMed/NCBI
|
|
13
|
Wexler SA, Donaldson C, Denning-Kendall P,
et al: Adult bone marrow is a rich source of human mesenchymal
‘stem’ cells but umbilical cord blood and mobilized adult blood are
not. Br J Haematol. 121:368–374. 2003. View Article : Google Scholar : PubMed/NCBI
|