Introduction
At present, there are two scanning modes for
computed tomography coronary angiography (CTCA); prospective and
retrospective electrocardiogram (ECG)-gated scanning. Retrospective
ECG-gated spiral scanning requires higher doses of radiation than
prospective scanning (1,2). Prospective sequential scanning is able
to effectively reduce the radiation dose required for a narrow
scanning window, which is increasingly used in CTCA examinations
(3–5). However, research is mostly focused on
low-dose adaptive sequential sequencing (6). There are a limited number of studies
that investigated how radiation doses may be optimized according to
changes in the heart rate in ECG pulsing windows of prospective
sequential CTCA scanning. Thus, further research is required into
methods of reducing the radiation dose of a CTCA scan, while
ensuring the image quality of the coronary artery remains
sufficient. This is particularly important for overweight [body
mass index (BMI) of >24] patients who typically require higher
radiation doses in order to obtain high quality images. In the
present study, overweight patients were examined using ECG-gated
automatic tube current modulation (ATCM) technology in prospective
sequential scanning. The dose and exposure times were adjusted
according to changes in the heart rate, and the feasibility of the
radiation dose and imaging of the coronary arteries were
compared.
Materials and methods
Patients
Between March and August 2013, patients suspected of
having coronary heart disease were recruited to undergo a CTCA
examination in the Fifth Affiliated Hospital of Xinjiang Medical
University (ürümqi, China). A total of 40 patients were recruited,
of which 12 were female and 28 were male. Patient age ranged
between 32 and 65 years, with an average age of 55.6 years. The BMI
scores ranged between 25.6 and 30. Patients were divided randomly
into two groups. Group A consisted of 20 patients, 14 male and 6
female, with an age range of 32–65 years (mean age, 52.8 years) and
a mean BMI of 27.8±2.84. For group A patients with heart rates
<70 bpm, the scanning range was 20–80% R-R interval and the
patients received a full dose of X-rays for 60–80% of the R-R
interval. In the group A patients with heart rates >70 bpm, the
scanning range was 20–80% R-R interval and the patients received a
full radiation dose for 35–55% of the R-R interval. For group B
patients (male, 17; female, 3; age range, 33–62 years; average age,
57.6 years; average BMI, 28.08±1.96) with any heart rate, the
scanning range was 20–80% of the R-R interval and patients received
full-dose radiation for the entire scan. The two groups presented
stable heart rates prior to examination. Image quality and
radiation dose were compared between the two groups.
Patients provided written consent prior to all
procedures. Patients with severe liver/kidney dysfunction, allergy
to iodine contrast agent, decompensated cardiac insufficiency or
those that were unable to hold their breath were excluded from the
study.
Equipment and scanning method
Patients underwent respiratory training prior to
scanning of the entire heart region by ECG-gated detection, using a
second-generation dual-source computed tomography scanner (SOMATOM
Definition Flash; Siemens Healthcare, Munich, Germany). Monitoring
levels were set at 1–2 cm under the trachea bifurcation, and the
region of interest was selected in the aortic arch. Bolus tracking
was used to initiate the automatic scan once the trigger threshold
of the 180 HU was reached (delay, 8 sec). An injection of 70–90 ml
iopamidol (iodine content, 370 mg/ml; Shanghai Bracco Sine
Pharmaceutical Corp. Ltd., Shanghai, China) was administered at a
rate of 6 ml/sec. Scanning parameters were as follows: Tube
rotation speed, 0.28 r/sec; detector area, 128×0.6 mm; voltage, 120
kV; reconstruction interval, 0.5 mm; and reconstruction thickness,
0.75 mm. The tube current-time product was automatically set
according to the patient BMI.
Image quality analysis
Image data were postprocessed by two experienced
physicians using a double-blind method. Coronary arteries were
divided into 15 segments, following the improved coronary artery
segmentation techniques of the American Heart Association (7). The image quality evaluation standards
were divided into three grades as follows: Grade I, coronary artery
has no artifacts and the contour is clear; grade II, local coronary
arteries have artifacts or vasculature is unclear; and grade III,
coronary vascular outline is unclear, or the middle segment or the
majority of the segments have artifacts. Grade I and II images were
sufficient for evaluation and diagnosis, while grade III images
were of insufficient quality.
Calculation of X-ray radiation
dose
The method used for calculating the effective X-ray
radiation dose of the CTCA scans was as follows (8): Effective radiation dose (ED) =
dose-length product (DLP) × conversion coefficient of the examined
position (K). For example, ED = DLP (mGy·cm) × 0.017
[mSv/(mGy·cm)], when chest conversion coefficient is K=0.017
[mSv/(mGy·cm)].
Statistical analysis
Using SPSS software, version 13.0 (SPSS, Inc.,
Chicago, IL, USA), the χ2 test was conducted for image
quality evaluation of the coronary arteries and the t-test was used
for the two independent samples. P<0.05 was considered to
indicate a statistically significant difference.
Results
General patient data
Patients underwent a routine sequence examination in
addition to optimized ECG tube-current modulation. No adverse
reactions were observed. The BMI values in groups A and B were
27.8±2.84 and 28.08±1.96 kg/m2, respectively, and no
significant difference was observed between the groups (P>0.05;
Table I).
 | Table I.Comparison of statistical results of
the image quality between groups A and B. |
Table I.
Comparison of statistical results of
the image quality between groups A and B.
| Group | n | BMI
(kg/m2) | CTDIvol (mGy) | DLP (mGy·cm) | ED (mSv) |
|---|
| A | 20 | 27.8±2.84 | 28.82±18.00 | 406.2±163.3 | 6.91±2.78 |
| B | 20 | 28.08±1.96 | 51.86±10.63 | 613.3±197.5 | 10.43±3.36 |
| Value t or t | N/A | 1.159 | 8.975 | 7.575 | 7.575 |
| P-value | N/A | 0.249 | 0.000 | 0.000 | 0.000 |
Image quality analysis
There were 505 and 494 coronary artery segments in
groups A and B, respectively. The number of patients with an image
quality score of grade I in groups A and B was 406/505 (80.4%) and
391/494 (79.1%), respectively. In total, 81/505 (16.0%) patients in
group A and 82/494 (16.6%) patients in group B received an image
quality score of grade II. With a grade III image quality score,
there were 18/505 (3.6%) patients in group A and 21/494 (4.3%) in
group B, and no significant difference was identified between the
groups. The assessment rates of groups A and B were 96.4 and 95.7%,
respectively (P=0.57; Table II).
Grade III-quality images were frequently acquired from the middle
and distal artery segments. A single patient in group A exhibited
heart rate fluctuations that caused the scanning acquisition period
to fall out of the full-dose exposure area, increasing image noise.
Although the phase was reconstructed, vessel artifacts
appeared.
 | Table II.Assessment of image quality for
coronary artery CTA segments in groups A and B. |
Table II.
Assessment of image quality for
coronary artery CTA segments in groups A and B.
| A | B | Total | Assessment Ratio
(%) |
|---|
|
|
|
|
|---|
| Coronary artery
segments | I | II | III | I | II | III | A | B | A | B |
|---|
| RCA (proximal) | 33 | 7 | 0 | 37 | 3 | 0 | 40 | 40 | 100 | 100 |
| RCA (middle) | 29 | 8 | 3 | 30 | 8 | 2 | 40 | 40 | 92.5 | 95 |
| RCA (distal) | 28 | 7 | 2 | 31 | 6 | 2 | 37 | 39 | 94.6 | 94.9 |
| PDA (right) | 19 | 9 | 0 | 19 | 10 | 1 | 28 | 30 | 100 | 96.7 |
| LM | 37 | 3 | 0 | 37 | 3 | 0 | 40 | 40 | 100 | 100 |
| LAD (proximal) | 36 | 4 | 0 | 35 | 5 | 0 | 40 | 40 | 100 | 100 |
| LAD (middle) | 34 | 4 | 2 | 32 | 6 | 2 | 40 | 40 | 95 | 95 |
| LAD (distal) | 23 | 12 | 2 | 28 | 9 | 3 | 37 | 40 | 94.6 | 92.5 |
| D1 | 29 | 7 | 2 | 25 | 8 | 1 | 38 | 34 | 94.7 | 97.1 |
| D2 | 13 | 2 | 2 | 8 | 3 | 1 | 17 | 12 | 88.2 | 91.7 |
| LCX (proximal) | 37 | 3 | 0 | 33 | 7 | 0 | 40 | 40 | 100 | 100 |
| LCX (distal) | 36 | 2 | 1 | 29 | 4 | 3 | 40 | 36 | 97.5 | 91.7 |
| OM | 27 | 6 | 2 | 30 | 4 | 3 | 35 | 37 | 94.3 | 91.9 |
| PL | 21 | 6 | 2 | 16 | 5 | 3 | 29 | 26 | 93.1 | 88.5 |
| PDA (left) | 4 | 1 | 0 | 1 | 1 | 0 | 5 | 2 | 100 | 100 |
| Total | 406 | 81 | 18 | 391 | 82 | 21 | 506 | 496 | 96.3 | 96.4 |
| χ2 |
|
|
|
|
|
|
|
| P=0.57 |
Calculation of the X-ray radiation
dose
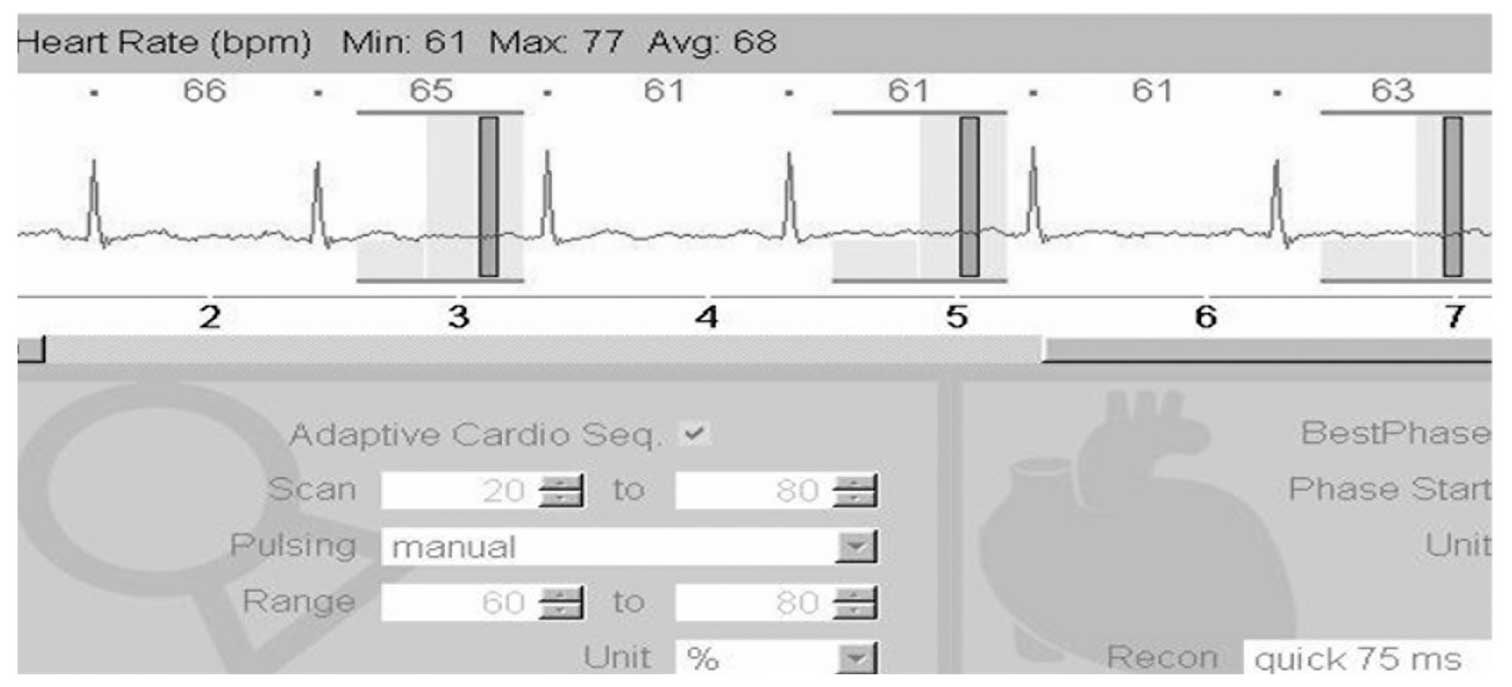
In group A patients with heart rates <70 bpm
(Fig. 1), the scanning range was
20–80% of the R-R interval and patients received full-dose
radiation for 60–80% of the R-R interval. For group A patients with
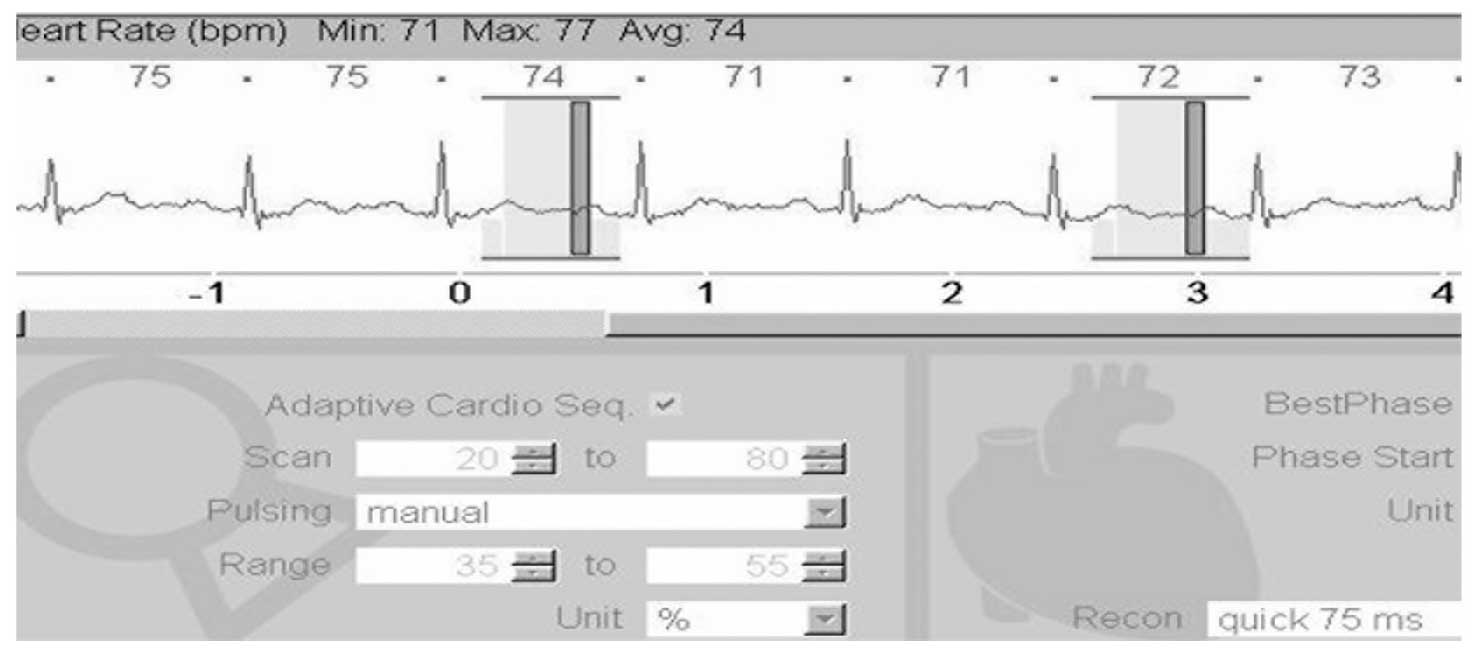
heart rates >70 bpm (Fig. 2), the
scanning range was 20–80% of the R-R interval and patients received
full-dose radiation for 35–55% of the R-R interval. In group A,
patients received an X-ray dose that was 20% of the full dose for
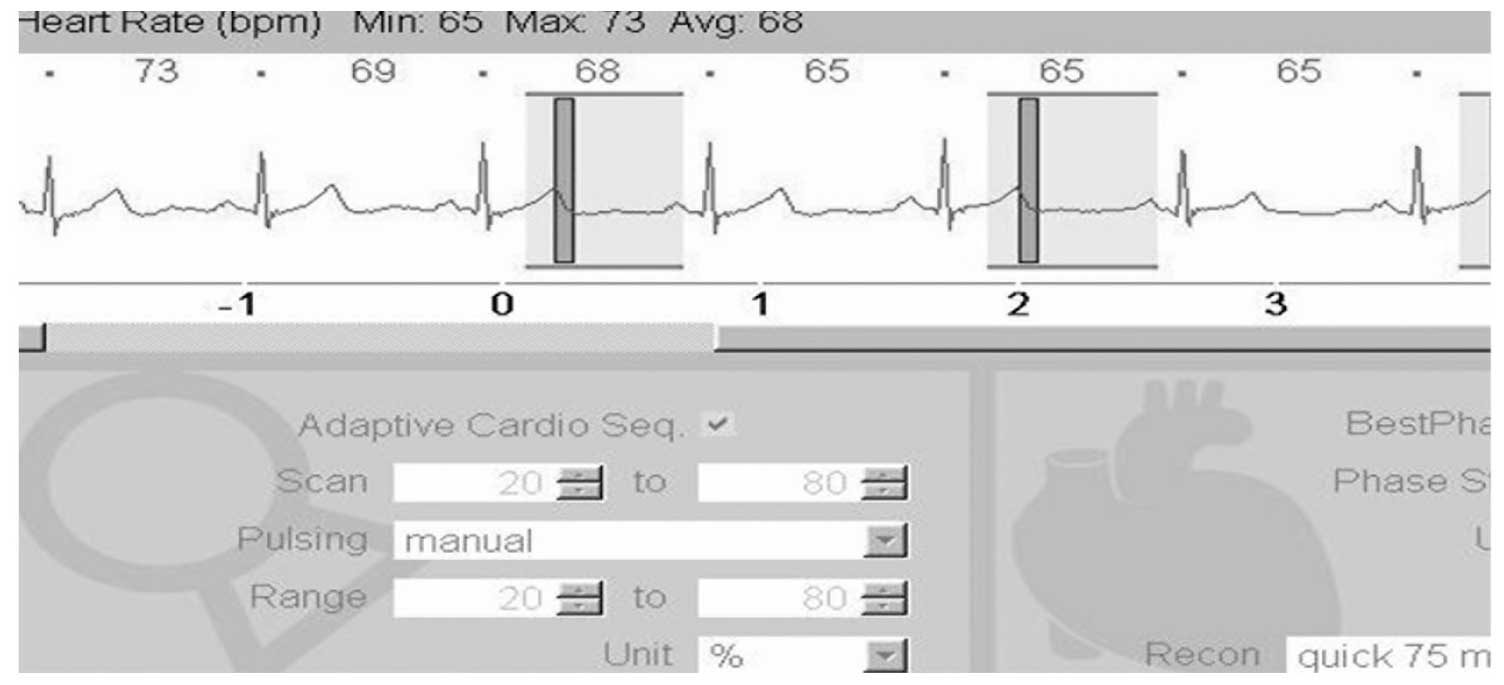
20–35% and 55–80% of the R-R interval. In group B, the scanning
range was 20–80% of the R-R interval and patients received a full
radiation dose for the entire scan (Fig.
3). In the present study, the computed tomography dose index
volume (CTDIvol) of group A was 55.57% of that in group B, and the
DLP and ED were 66.23 and 66.25% of the group B values,
respectively (Table I). No
significant difference in image quality was observed between the
groups. For patients with a high BMI, selecting a different total
dose exposure window according to different heart rates appeared to
reduce the required radiation dose.
In group A, the CTDIvol was 28.82±18.00 mGy, the DLP
was 406.2±163.3 mGy·cm and the average ED of radiation was
6.91±2.78 mSv. In group B, the CTDIvol was 51.86±10.63 mGy, the DLP
was 613.3±197.5 mGy·cm and the average ED of radiation was
10.43±3.36 mSv. Significant differences in CTDIvol, ED, DLP and ED
average were observed between the groups (P<0.05). The
assessment of image quality for coronary artery CTA segments
indicated that there was no significant difference in image quality
between the groups.
Discussion
CTCA imaging is used widely in clinical practice,
however high radiation doses are potentially harmful and their
effects are under increasing investigation (9). The American Food and Drug
Administration Commission issued a statement by the American Heart
Committee, stating that a 10 mSv dose of CT radiation may cause
1/2,000 patients to develop a malignant tumor (10). Davis et al (11) demonstrated that a higher radiation
dose increased the risk of testicular cancer and glioma in patients
that underwent CT scans. Therefore, doctors and imaging technicians
aim to maintain the quality of coronary artery imaging during CTCA
scanning, whilst also limiting the harm caused to the body by
excessive X-ray radiation. It is important to design optimized
scanning procedures in order to ensure that high quality coronary
artery images are obtained using the lowest possible radiation
dose. Current methods of controlling dual-source CT radiation dose
include automatic mA modulation, variable and intelligent filtering
technology, prospective gating control scan mode and
phase-selective exposure technology. A report by the American Heart
Association concluded that gating scanning technology was the most
promising of these technologies (12).
BMI is the internationally recognized system for
assessing the degree of obesity in overweight patients. In the case
of obese patients, the required X-ray penetration increases with
the volume of subcutaneous fat and muscle thickness, therefore the
necessary radiation dose may also increase (13). The smaller the radiation dose, the
worse the image quality. When BMI is high, an increased tube
current is required to ensure image quality (14). However, by using tube current
modulation in dual-source CT scanning, the tube current may be
automatically adjusted as required, which reduces the X-ray
radiation dose administered to patients. In the present study,
varying tube currents were administered at different ECG periods.
The radiation dose administered in group A following optimization
(6.91±2.78) was significantly lower when compared with group B
(10.43±3.36) without optimization, with no significant difference
in image quality (Figs. 1–3).
Arnoldi et al (15) demonstrated that when using
prospective scanning, the required radiation dose is 2.8 mSv, which
is markedly lower than the retrospective scanning dose of 18.4 mSv.
A prospective series scan is a step-axis scanning mode, which
reduces the rate of scan overlap and is therefore able to
significantly reduce the necessary radiation dose. However, the
radiation dose for patients with a high BMI remains greater
compared with patients with a normal BMI, despite the use of
routine sequence scanning.
ECG-ATCM scanning is based on the average heart rate
prior to the scan, which is used to select a time window in the
optimum phase of the cardiac cycle for full-dose exposure. The
diastolic period is an important phase of the cardiac cycle and the
tube current was full during this period. In addition, tube current
was reduced during the systole period and decreased for the
remaining period of the scan, with 20% of the full-dose exposure
administered in the other heart regions (16,17).
Araoz et al (18) previously
reported that the scanning range of dual-source CT is 65–70% of the
R-R interval for a heart rate ≤70 bpm and 35–40% of the R-R
interval for a heart rate >70 bpm.
In the sequence scanning of the present study, for
group A patients with a high BMI and a heart rate ≤70 bpm, the
scanning range was 20–80% of the R-R interval, and patients
received full-dose radiation for 60–80% of the R-R interval. For
group A patients with heart rates >70 bpm, the scanning range
was 20–80% R-R of the interval, with patients receiving a full
X-ray dose for 35–55% of the R-R interval and a 20% X-ray dose for
the remainder of the scanning period (20–35% and 55–80% of the R-R
interval). In this manner, the required radiation dose may be
further reduced. There are drawbacks to this prospective scanning
technology, as the data was obtained from only part of the full
heartbeat cycle. It cannot undergo ECG editing and cannot evaluate
the heart function, particularly in cases of patients with an
irregular heartbeat, which may result in a failed scan.
In conclusion, dual-source CT is able to produce
high quality coronary artery images (19,20),
while exposing patients to relatively low radiation doses. ATCM and
alternative technologies, including pitch-heart rate automatic
matching, facilitate significant reductions in the radiation dose
of CTCA examination compared with standard CTCA. Furthermore, the
use of ECG-ATCM in prospective sequence scanning permits the
selection of different total dose exposure windows based on patient
heart rate. This selectivity may significantly reduce the required
radiation dose in overweight patients. In order to obtain
satisfactory image quality, doctors and imaging technicians require
an extensive understanding of the hazards of ionizing radiation and
should aim to achieve low-dose scanning to reduce the exposure of
patients to hazardous radiation.
References
|
1
|
Shah DJ, Sachs RK and Wilson DJ:
Radiation-induced cancer: a modern view. Br J Radiol.
85:e1166–e1173. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sodickson A, Baeyens PF, Andriole KP, et
al: Recurrent CT, cumulative radiation exposure, and associated
radiation-induced cancer risks from CT of adults. Radiology.
251:175–184. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Husmann L, Valeta I, Gaemperli O, et al:
Feasibility of low-dose coronary CT angiography: first experience
with prospective ECG-gating. Eur Heart J. 29:191–197. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Buechel RR, Husmann L, Herzog BA, et al:
Low-dose computed tomography coronary angiography with prospective
electrocardiogram triggering: feasibility in a large population. J
Am Coll Cardiol. 57:332–336. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Achenbach S, Goroll T, Seltmann M, et al:
Detection of coronary artery stenoses by low-dose, prospectively
ECG-triggered, high-pitch spiral coronary CT angiography. JACC
Cardiovasc Imaging. 4:328–337. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Abada HT, Larchez C, Daoud B, et al: MDCT
of the coronary arteries: feasibility of low-dose CT with
ECG-pulsed tube current modulation to reduce radiation dose. AJR Am
J Roentgenol. 186:(Suppl 2). S387–S390. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Austen WG, Edwards JE, Frye RL, et al: A
reporting system on patients evaluated for coronary artery disease.
Report of the Ad Hoc Committee for Grading of Coronary Artery
Disease, Council on Cardiovascular Surgery, American Heart
Association. Circulation. 51:(4 Suppl). 5–40. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Alkadhia H, Stolzmanna P, Scheffel H, et
al: Radiation dose of cardiac dual-source CT: the effect of
tailoring the protocol to patient-specific parameters. Eur J
Radiol. 68:385–391. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nickoloff EL and Alderson PO: Radiation
exposures to patients from CT: reality, public perception, and
policy. AJR Am J Roentgenol. 177:285–287. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Budoff MJ, Achenbach S, Blumenthal RS, et
al: American Heart Association Committee on Cardiovascular Imaging
and Intervention; American Heart Association Council on
Cardiovascular Radiology and Intervention; American Heart
Association Committee on Cardiac Imaging, Council on Clinical
Cardiology : Assessment of coronary artery disease by cardiac
computed tomography: A scientific statement from the American Heart
Association Committee on Cardiovascular Imaging and Intervention,
Council on Cardiovascular Radiology and Intervention, and Committee
on Cardiac Imaging, Council on Clinical Cardiology. Circulation.
114:1761–1791. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Davis F, Ilyasova D, Rankin K, et al:
Medical diagnostic radiation exposures and risk of gliomas. Radiat
Res. 175:790–796. 2011. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Budoff MJ, Achenbach S, Blumenthal RS, et
al: American Heart Association Committee on Cardiovascular Imaging
and Intervention; American Heart Association Council on
Cardiovascular Radiology and Intervention; American Heart
Association Committee on Cardiac Imaging, Council on Clinical
Cardiology: Assessment of coronary artery disease by cardiac
computed tomography: a scientific statement from the American Heart
Association Committee on Cardiovascular Imaging and Intervention,
Council on Cardiovascular Radiology and Intervention, and Committee
on Cardiac Imaging, Council on Clinical Cardiology. Circulation.
114:1761–1791. 2006.
|
|
13
|
Slovis TL: CT and computed radiography:
the pictures are great, but is the radiation dose greater than
required? AJR Am J Roentgenol. 179:39–41. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Manowitz A, Sedlar M, Griffon M, et al:
Use of BMI guidelines and individual dose tracking to minimize
radiation exposure from low-dose helical chest CT scanning in a
lung cancer screening program. Acad Radiol. 19:84–88. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Arnoldi E, Johnson TR, Rist C, et al:
Adequate image quality with reduced radiation dose in prospectively
triggered coronary CTA compared with retrospective techniques. Eur
Radiol. 19:2147–2155. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Earls JP, Berman EL, Urban BA, et al:
Prospectively gated transverse coronary CT angiography versus
retrospectively gated helical technique: improved image quality and
reduced radiation dose. Radiology. 246:742–753. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Scheffel H, Alkadhi H, Plass A, et al:
Accuracy of dual-source CT coronary angiography: First experience
in a high pre-test probability population without heart rate
control. Eur Radiol. 16:2739–2747. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Araoz PA, Kirsch J, Primak AN, et al:
Optimal image reconstruction phase at low and high heart rates in
dual-source CT coronary angiography. Int J Cardiovasc Imaging.
25:837–845. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hamon M, Morello R, Riddell JW and Hamon
M: Coronary arteries: diagnostic performance of 16- versus
64-section spiral CT compared with invasive coronary angiography -
meta-analysis. Radiology. 245:720–731. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Paul JF, Amato A and Rohnean A: Low-dose
coronary-CT angiography using step and shoot at any heart rate:
comparison of image quality at systole for high heart rate and
diastole for low heart rate with a 128-slice dual-source machine.
Int J Cardiovasc Imaging. 29:651–657. 2013.PubMed/NCBI
|