Introduction
Osteoarticular tuberculosis (TB), an uncommon form
of extrapulmonary TB, comprises 1–6% of all TB cases and 10–15% of
all extrapulmonary TB cases (1–4). The
most frequent sites of osteoarticular TB are the spine, hip and
knee. Multifocal skeletal TB is rare and accounts for 10% of all
osteoarticular TB cases (5).
The diagnosis of multifocal osteoarticular TB is
often delayed due to the clinical and radiological resemblance of
the disease to numerous malignant and bone diseases (6,7). The
consequences of considerable diagnostic delays in multifocal
osteoarticular TB can prove critical for patients, since such
delays may lead to the spread of the infection from the bone to the
adjacent joints and surrounding soft tissue, causing significant
functional disabilities (8,9). The present study describes the case
report of a patient that presented with multifocal extremity pain
and swellings and, following several TB modalities, was diagnosed
with multifocal osteoarticular TB. The patient responded well to
anti-TB medication.
Case report
A 19-year-old Chinese male presented with multifocal
painful swellings of his extremities, particularly around the
ankles and the interphalangeal and intermetatarsal joints. The
patient had been suffering from the painful swelling for ~3 years
and with sinus discharge in certain areas for ~1 year.
Three years ago, the patient felt pain around his
left ankle and several interphalangeal joints of the left foot.
Subsequently, some of the lesions began to fester. Similar lesions
also appeared symmetrically on the left and right hand and right
foot. The patient had a history of pulmonary TB that had been
diagnosed 6 years prior to these events; however, the district
hospital had confirmed that the condition was cured after 6 months
of medication (a 2-month treatment with isoniazid, rifampin and
pyrazinamide and a 4-month treatment with isoniazid plus
rifampin).
Whilst the patient presented with decreased
appetite, he had no history of significant weight loss, night
sweats or chronic cough, and he had not taken any immunosuppressive
or steroid drugs. The most recent computerized tomography (CT)
scans of the patient's chest were normal. In addition, no family
members of the patient had presented with the same pattern of
symptoms. The patient weighed 50 kg and appeared to be
malnourished.
Upon physical examination, the proximal
interphalangeal joint of the patient's thumb, index, middle and
little finger of the right hand, thumb of the left hand and right
and left feet were swollen. Ulcers were visible on both of the
patient's thumbs and on the left foot. The patient was in pain and
had difficulty moving his extremities. Laboratory blood-test
results showed normal peripheral blood count values and raised
erythrocyte sedimentation rate (75 mm at the end of 1 h). The
enzyme-linked immunosorbent assay was negative for human
immunodeficiency virus and the radiographs of the thoracolumbar
spine, chest and pelvis were normal. The plain radiograph showed
soft tissue swelling at the proximal interphalangeal and
intermetatarsal joints of the aforementioned digits, as well as
narrowing of the joints, and several digits presented with
sclerosis and osteopenia (Fig. 1).
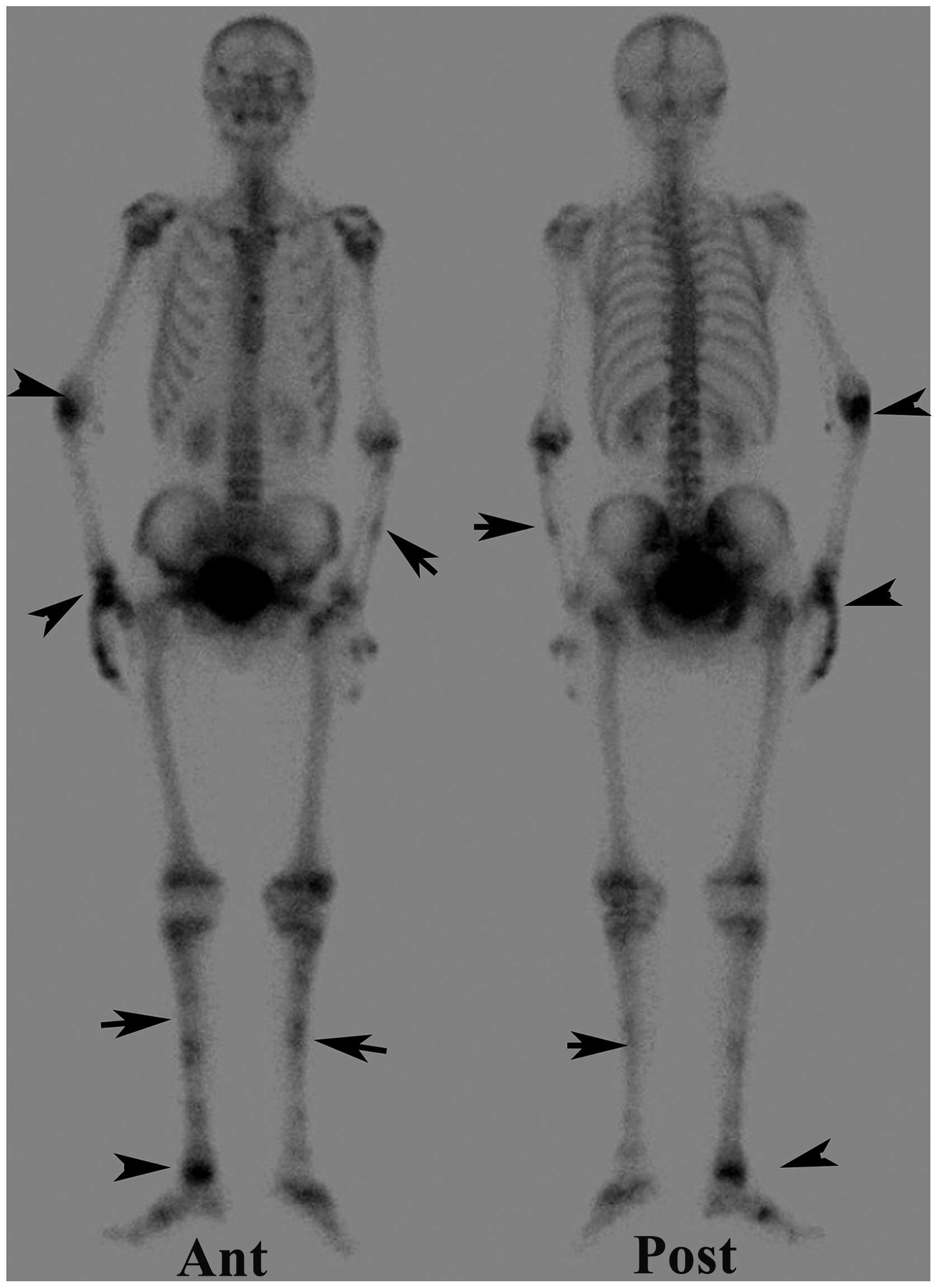
The whole body 99mTc-methylene diphosphonate (MDP) bone
scan revealed multiple abnormal foci in the extremities (Fig. 2). Magnetic resonance imaging (MRI) of
both feet revealed pathological signal intensity changes inside the
bones, along with marginal enhancement following contrast injection
(Fig. 3).
The biopsy of the second left toe lesion showed a
granulomatous lesion with necrosis (including Langhans giant cell
and epithelioid cell central caseation), which was suggestive of
TB; however the acid-fast stain (Ziehl-Neelsen) showed no acid-fast
bacilli (AFB). The diagnosis of TB was confirmed by the polymerase
chain reaction (PCR). Anti-TB medication was then prescribed,
consisting of isoniazid, rifampin, streptomycin and ethambutol.
Compared with the previous prescription of the patient, which
consisted of three types of medicine, the new regimen comprised
four types, including two new drugs that were added in case of drug
resistance. After 3 months of treatment, the lesions gradually
healed and the pain and swelling subsided. At present, 2 years
after the treatment, the patient can stand on his own feet without
any symptoms of pain or swelling.
Discussion
To the best of our knowledge, this is the first
reported case of multifocal osteoarticular TB affecting all the
extremities, predominantly the bones. Although no AFB were
detected, positive PCR results for Mycobacterium
tuberculosis confirmed the diagnosis. Furthermore, the response
of the patient to anti-TB medication revealed strong evidence of TB
infection.
Multifocal skeletal TB most often affects the spine,
whereas tuberculous arthritis affects the weight-bearing joints and
extraspinal tuberculous osteomyelitis affects the skeletal system,
excluding the spine (10). The
preference of TB for large joints and the spine can be explained by
the rich vascular supply of the vertebra and the growth plates of
the long bones, in conjunction with the hematogenous spread of TB
(11–14). In the present study, TB was observed
in the long and short bones and the small joints of the
extremities, while the weight-bearing joints, such as the hips and
knees, remained healthy. The exact physiological mechanisms of TB
remain unclear and direct inoculation cannot completely explain the
symmetry of the afflictions. The presence of lesions in atypical
positions cannot exclude a diagnosis of TB.
Osteoarticular TB is a major cause of morbidity.
Diagnosis of multifocal skeletal TB is frequently delayed due to
its rarity and the considerably vague nature of its symptoms.
Furthermore, it is difficult to differentiate multifocal skeletal
TB from other bone lesions based on clinical or radiological
findings alone (15). In the present
study, lytic lesions were observed in the plain radiographs of the
extremities of the patient, and multiple MDP foci of varied
intensity were identified on the bone scans. Several bone diseases,
including Ollier's disease and Maffucci syndrome, were initially
considered as potential diagnoses. The high-intensity MDP foci
surrounding the right wrist, ankle and interphalangeal and
intermetatarsal joints may have been partly due to the fact that
the left side of the patient's body was affected first, with the
right side consequently becoming weight-bearing and functionally
compensating. Another possible explanation is that the infection on
the right side was more active.
Signal changes on the MRI scans suggested low-grade
bacterial infection. MRI can be used to discriminate between
abscesses and granulation tissue, delineate soft-tissue mass and
identify the amount of bone destruction (16); however, MRI may not be appropriate
for whole-body imaging as it is expensive and time-consuming
(17). Bone scans, on the other
hand, play an important role in the diagnosis and evaluation of TB
(17,18), since they can detect unsuspected
osseous TB in patients without known systemic diseases,
particularly patients suffering from pain but without known
malignancies. Bone scans also help to determine the optimal biopsy
site and the most suitable area for insightful MRI imaging. Bone TB
should be considered among the differential diagnoses when positive
bone scans are observed in patients with unknown causes of bone
pain, particularly in patients who do not have a known history of
malignancy (17,19).
In conclusion, pain and swelling may be
presentations of osteoarticular TB infection. Bone and MRI scans
are imaging techniques that have proven to be useful in indicating
the extent of the disease, particularly in long bone lesions in the
early stage of the disease. Bone scans are also useful in
establishing those sites that could require further evaluation by
CT, MRI or biopsy.
Acknowledgements
This study was supported by the National Natural
Science Foundation of China (grant no. 81071184) and the Sector
Funds of the Ministry of Health of China (grant no. 201002002).
References
|
1
|
Houston A and Macallan DC: Extrapulmonary
tuberculosis. Medicine. 42:18–22. 2014. View Article : Google Scholar
|
|
2
|
Jutte PC, van Loenhout-Rooyackers JH,
Borgdorff MW and van Horn JR: Increase of bone and joint
tuberculosis in The Netherlands. J Bone Joint Surg Br. 86:901–904.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sandher DS, Al-Jibury M, Paton RW and
Ormerod LP: Bone and joint tuberculosis: Cases in Blackburn between
1988 and 2005. J Bone Joint Surg Br. 89:1379–1381. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hong L, Wu JG, Ding JG, Wang XY, Zheng MH,
Fu RQ, et al: Multifocal skeletal tuberculosis: Experience in
diagnosis and treatment. Med Mal Infect. 40:6–11. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tuli SM: Tuberculous
osteomyelitisTuberculosis of the Skeletal System. 3rd. Jaypee
Brothers Medical Publishers Ltd; New Delhi: pp. 174–183. 2004,
View Article : Google Scholar
|
|
6
|
Go SW, Lee HY, Lim CH, Jee WH, Wang YP,
Yoo IeR and Kang JY: Atypical disseminated skeletal tuberculosis
mimicking metastasis on PET-CT and MRI. Intern Med. 51:2961–2965.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Johnstone RH, Ardern DW and Bartle DR:
Multifocal skeletal tuberculosis masquerading as metastatic
disease. ANZ J Surg. 81:731–733. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Cheung PY, Ho KW, Lam YL and Shek TW:
Unusual presentations of osteoarticular tuberculosis in two
paediatric patients. BMJ Case Rep.
2012:bcr20120067142012.PubMed/NCBI
|
|
9
|
Dhillon MS and Tuli SM: Osteoarticular
tuberculosis of the foot and ankle. Foot Ankle In. 22:679–686.
2001.
|
|
10
|
Moore SL and Rafii M: Imaging of
musculoskeletal and spinal tuberculosis. Radiol Clin North Am.
39:329–342. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gardam M and Lim S: Mycobacterial
osteomyelitis and arthritis. Infect Dis Clin North Am. 19:819–830.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tuli SM: General principles of
osteoarticular tuberculosis. Clin Orthop Relat Res. 39:11–19. 2002.
View Article : Google Scholar
|
|
13
|
Magnussen A, Dinneen A and Ramesh P:
Osteoarticular tuberculosis: Increasing incidence of a difficult
clinical diagnosis. Br J Gen Pract. 63:385–386. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Scanzello CR and Goldring SR: The role of
synovitis in osteoarthritis pathogenesis. Bone. 51:249–257. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Marudanayagam A and Gnanadoss JJ:
Multifocal skeletal tuberculosis: A report of three cases. Iowa
Orthop J. 26:151–153. 2006.PubMed/NCBI
|
|
16
|
Teo HE and Peh WC: Skeletal tuberculosis
in children. Pediatr Radiol. 34:853–860. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zhang Y, Zhang Y and Ma J: The prospect of
incidental detection of unsuspected skeletal tuberculosis by bone
scintigraphy should not be overlooked. Clin Nucl Med. 32:435–439.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Trikha V, Gupta V, Rastogi S and Kumar R:
Tuberculosis of calcaneus: Assessing treatment response by Tc-99m
MDP scintigraphy. Clin Nucl Med. 29:5062004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bhardwaj V, Agrawal M, Suri T, Sural S,
Kashyap R and Dhal A: Evaluation of adequacy of short-course
chemotherapy for extraspinal osteoarticular tuberculosis using
99mTc ciprofloxacin scan. Int Orthop. 35:1869–1874. 2011.
View Article : Google Scholar : PubMed/NCBI
|