Introduction
Rosai-Dorfman disease, also known as sinus
histiocytosis with massive lymphadenopathy, is a rare, idiopathic,
histiocytic proliferation disorder originally defined by Rosai and
Dorfman in 1969 (1). This disorder
commonly presents with bilateral painless lymphadenopathy in the
neck and is also associated with leukocytosis, fever, high
erythrocyte sedimentation rate and polyclonal
hypergammaglobulinemia (2). Between
25 and 40% of patients experience extranodal involvement,
particularly on the skin (2,3), ~3% of which is limited exclusively to
the skin (4), and is known as
cutaneous Rosai-Dorfman disease (CRDD). To date, there have been
~100 reported cases of CRDD in the literature (5). Clinical presentation and therapeutic
options of CRDD vary, and the etiology of the disease is still
unknown. The clinical manifestations include single or multiple
yellow-red to brown or purple papules, nodules and/or plaques, with
the face being the most frequently affected site. The histological
characteristics include varying numbers of polymorphous histiocytes
embedded in a mixed inflammatory infiltrate composed of
lymphocytes, plasma cells and/or neutrophils. The typical
histiocytes have abundant lightly eosinophilic cytoplasm and
vesicular nuclei and are positive for S-100 and cluster of
differentiation (CD)68 but negative for CD1a. The present case
report describes a case of pure CRDD in a middle-aged man.
Case report
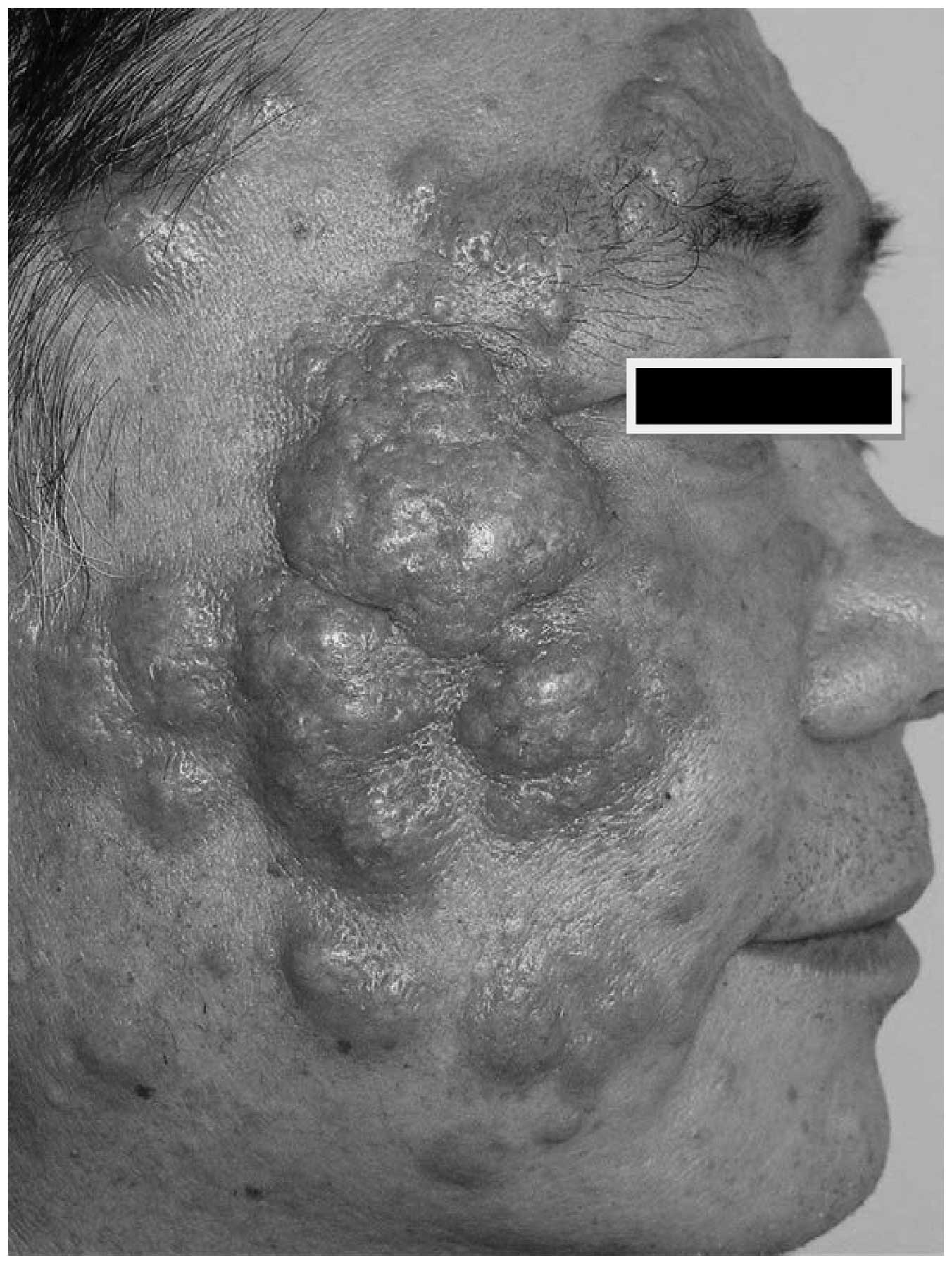
A 52-year-old man presented with an 8-month history
of multiple lesions on his face. The initial lesions comprised
several asymptomatic red papules on his cheeks and forehead, the
number of which slowly increased over time. Physical examination
revealed clustered or satellite firm, yellowish-red papules and
nodules, a number of which had coalesced into plaques exhibiting
telangiectasia and an irregular surface (Fig. 1). No fever, malaise, reduced
appetite, weight loss or lymphadenopathy was observed. Detailed
laboratory analyses, including complete blood count, biochemical
tests and serum lipoprotein profile were all in normal range.
Abdominal ultrasound and chest X-ray were also negative. All of the
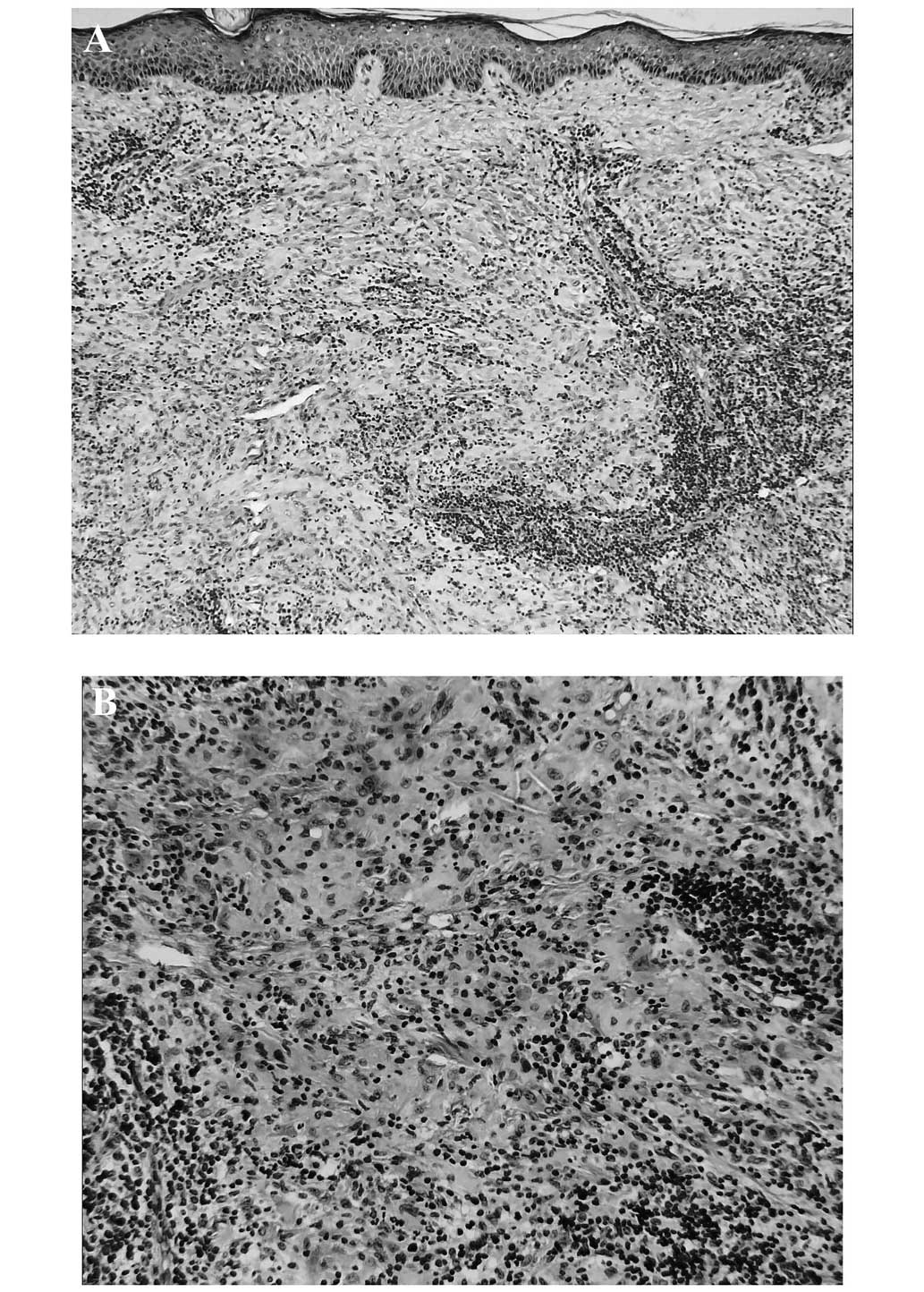
above showed that there was no systemic involvement. A biopsy
specimen from a red papule showed a dense, dermal infiltrate, which
was predominantly composed of large histiocytes with vesicular
nuclei and abundant pale pink cytoplasm embedded in aggregates of
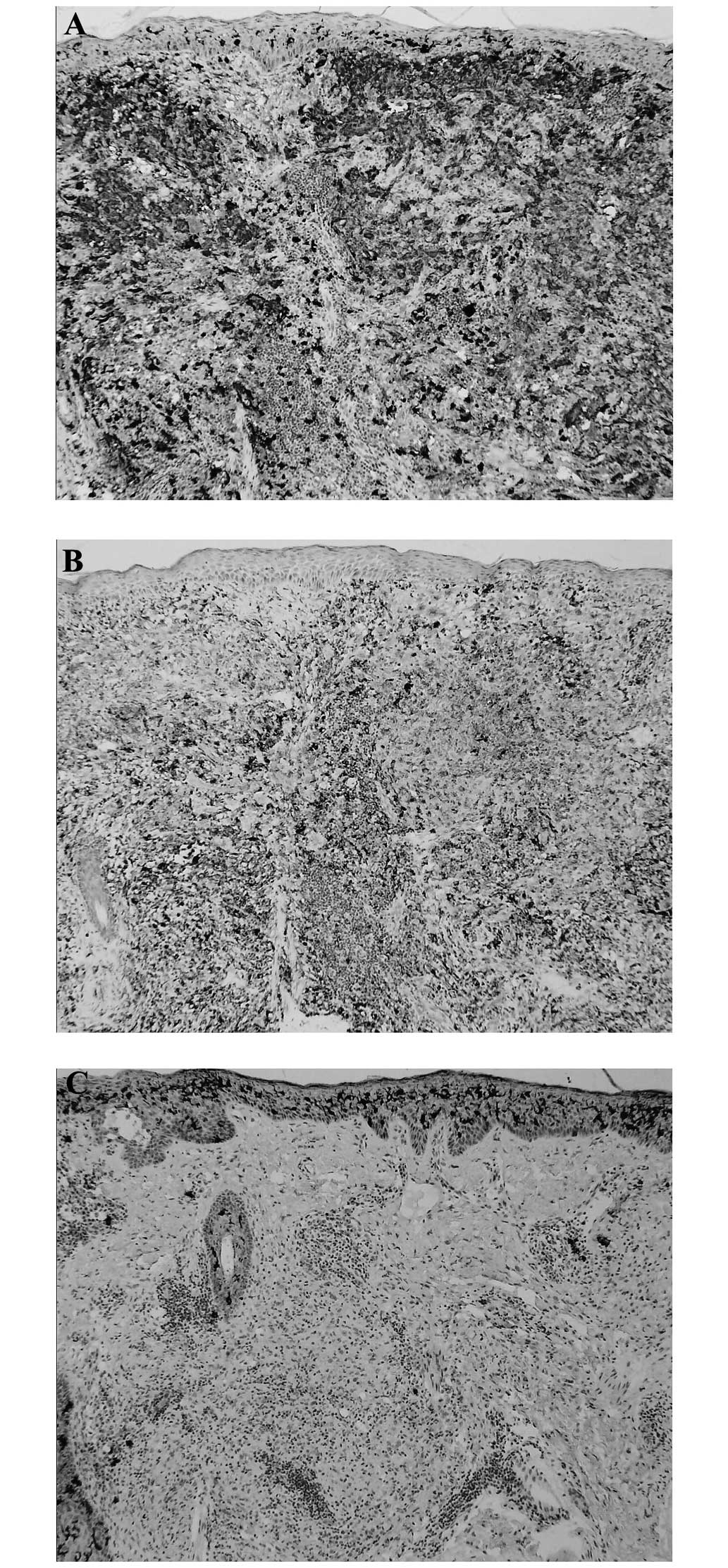
lymphocytes and scattered plasma cells and eosinophils (Fig. 2A and B). The histiocytes were
strongly positive for S-100 and CD68 (Fig. 3A and B), but negative for CD1a
(Fig. 3C). A diagnosis of CRDD was
made two weeks after the patient was admitted to the clinic
(Beijing Hospital, Beijing, China). The patient received oral
prednisone (30 mg/day) for one month, and achieved mild remission
but ultimately treatment was discontinued due to concerns about the
side effects of glucocorticoids and the cost of further therapies.
Informed consent was received from the patient.
Discussion
Pure CRDD has been regarded as a distinct clinical
entity from typical RDD with lymphadenopathy and/or internal organ
involvement with regard to its different epidemiology and the lack
of systemic involvement, even with long-term follow-up (6). The disease tends to affect older
Caucasian women and Asians, with the mean onset age of ~45 years
(4). The clinical manifestations of
CRDD include single or multiple, usually asymptomatic, yellow-red
to brown or purple papules, nodules and/or plaques, which most
frequently affect the face (4). The
most common presentation is papulonodular clusters coalescing into
verrucous plaques with surrounding satellite lesions (4). The diagnosis of CRDD rests on
histopathological findings; varying numbers of polymorphous
histiocytes may be observed to be embedded in a mixed inflammatory
infiltrate composed of lymphocytes, plasma cells and/or
neutrophils. A small number of eosinophils in the present case
appeared to show reactive proliferation; however, the significance
of a prominent eosinophilic infiltrate has not been elucidated
(7). Representative histiocytes have
abundant, lightly eosinophilic cytoplasm and vesicular nuclei, and
are positive for S-100 but negative for CD1a. The presence of
histiocytes with intact, phagocytosed lymphocytes, plasma cells or
neutrophils (emperipolesis) is not very common in pure CRDD
(8). The etiology of CRDD has been
putatively linked to infectious agents, including human herpes
virus 6, Epstein-Barr virus or herpes zoster virus, and
immunological triggers, such as autoimmune diseases, pneumococcal
vaccination and scars associated with previous surgery (9). The clinical course of the disease
varies, with certain cases spontaneously resolving after months or
years and others persisting despite multiple treatment efforts.
Therapeutic options include surgery, radiotherapy (10), cryotherapy (11), retinoids (12), dapsone (75 mg/day) (13) or high-dose thalidomide (300 mg/day)
(14), oral or intralesional
corticosteroids (15), low-dose
methotrexate (5,16) and imatinib (17).
The patient in the present study was a middle-aged
man who exhibited the typical clinical manifestations of CRDD. The
condition was slow in growth and without any indication of
regression. Even though the patient showed only a marginal response
to a month of low-dose prednisone (30 mg/day), he may have had a
significant improvement if he was treated with retinoids or
high-dose thalidomide.
References
|
1
|
Rosai J and Dorfman RF: Sinus
histiocytosis with massive lymphadenopathy: A newly recognized
benign clinicopathologic entity. Arch Pathol. 87:63–70.
1969.PubMed/NCBI
|
|
2
|
Foucar E, Rosai J and Dorfman R: Sinus
histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease):
Review of the entity. Semin Diagn Pathol. 7:19–73. 1990.PubMed/NCBI
|
|
3
|
Pitamber HV and Grayson W: Five cases of
cutaneous Rosai-Dorfman disease. Clin Exp Dermatol. 28:17–21. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lu CI, Kuo TT, Wong WR and Hong HS:
Clinical and histopathological spectrum of cutanous Rosai-Dorfman
disease in Taiwan. J Am Acad Dermatol. 51:931–939. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sun NZ, Galvin J and Cooper KD: Cutaneous
Rosai-Dorfman disease successfully treated with low-dose
methotrexate. JAMA Dermatol. 150:787–788. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Brenn T, Calonje E, Granter SR, et al:
Cutaneous Rosai-Dorfman disease is a distinct clinical entity. Am J
Dermatopathol. 24:385–391. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cangelosi JJ, Prieto VG and Ivan D:
Cutaneous Rosai-Dorfman disease with increased number of
eosinophils: Coincidence or histologic variant? Arch Pathol Lab
Med. 135:1597–1600. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Molina-Garrido MJ and Guillén-Ponce C:
Extranodal Rosai-Dorfman disease with cutaneous and periodontal
involvement: A rare presentation. Case Rep Oncol. 4:96–100. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bassis AV, Fairley JA, Ameln RT and Swick
BL: Cutaneous Rosai-Dorfman disease following pneumococcal
vaccination. J Am Acad Dermatol. 65:890–892. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bunick CG, Leffell D, Bosenberg M, et al:
Cutaneous Rosai-Dorfman disease of the right ear responsive to
radiotherapy. J Am Acad Dermatol. 67:e225–e226. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Fumerton R, Ball N and Zhou Y: Refractory
cutaneous Rosai-Dorfman disease responsive to cryotherapy. Cutis.
87:296–299. 2011.PubMed/NCBI
|
|
12
|
Fening K, Bechtel M, Peters S, et al:
Cutaneous Rosai-Dorfman disease persisting after surgical excision:
Report of a case treated with acitretin. J Clin Aesthet Dermatol.
3:34–36. 2010.PubMed/NCBI
|
|
13
|
Chang HS, Son SJ, Cho KH and Lee JH:
Therapeutic challenge of dapsone in the treatment of purely
cutaneous Rosai-Dorfman disease. Clin Exp Dermatol. 36:420–422.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tjiu JW, Hsiao CH and Tsai TF: Cutaneous
Rosai-Dorfman disease: Remission with thalidomide treatment. Br J
Dermatol. 148:1060–1061. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Oka M, Kamo T, Goto N, et al: Successful
treatment of Rosai-Dorfman disease with low-dose oral
corticosteroid. J Dermatol. 36:237–240. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Nadal M, Kervarrec T, Machet MC, et al:
Cutaneous Rosai-Dorfman disease located on the breast: Rapid
effectiveness of methotrexate after failure of topical
corticosteroids, acitretin and thalidomide. Acta Derm Venereol. Jan
29–2015.(Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gebhardt C, Averbeck M, Paasch U, et al: A
case of cutaneous Rosai-Dorfman disease refractory to imatinib
therapy. Arch Dermatol. 145:571–574. 2009. View Article : Google Scholar : PubMed/NCBI
|