Introduction
Extracranial carotid artery aneurysm (ECAA) is an
uncommon type of aneurysm, accounting for 0.4–4% of all peripheral
artery aneurysms (1–3). Atherosclerosis is considered to be the
primary cause of aneurysm formation. In addition, dysplastic,
traumatic or infectious lesions, neck irradiation and other factors
are infrequently reported (4–6). The
spontaneous rupture of an ECAA is rare (7). Neurological abnormalities are the most
common manifestation of an ECAA, whereas hemorrhages or nerve
compression as a result of giant aneurysms are rarely observed
(7). Prevention of thromboembolic
events is the primary aim of ECAA treatments (8).
Existing treatments for ECAA involve surgical
procedures, such as resection with end-to-end anastomosis or
grafting, internal carotid artery ligation or extracranial to
intracranial bypass (8), and
endovascular stenting (9). It has
been reported that endovascular intervention for ECAA is an
emerging alternative treatment that has yielded promising results
(10). Due to the limited number of
large studies, the safety and efficacy in surgical and
interventional management of ECAA is unclear. The optimum treatment
has not been clearly defined (11).
The present study reports four cases of ECAA, with the aim of
describing experience gained in the surgical and interventional
management of ECAA. This study was approved by the ethic committee
of Xuanwu Hospital. Written informed consent was obtained from all
of the patients.
Case reports
Case 1
The patient was a 69-year-old woman that presented
with a left-sided cervical mass for 9 years and complained of pain
for weeks. The mass gradually increased in size for 2 years. The
patient denied having any history of trauma, infection or previous
surgical intervention. Physical examination revealed a pulsatile
mass in the left-sided cervical region. Angiography and ultrasound
examinations indicated that the mass was a pseudoaneurysm (size,
4.0×3.1 cm). The patient received a carotid artery stent; however,
the surgery was unsuccessful and the pseudoaneurysm ruptured.
Subsequently, two balloons (Balt Extrusion, Montmorency, France)
were used to occlude the internal carotid artery and common carotid
artery. The thrombus relocated to the distal end of the left middle
cerebral artery, resulting in cerebral infarction.
Case 2
The patient was an 82-year-old woman that presented
with left-sided cervical swelling and complained of hoarseness and
dysphagia for the preceding year. The patient possessed no history
of trauma, infection or any previous surgical intervention.
Physical examination revealed the presence of a pulsatile mass in
the left-sided cervical region, a weak pharyngeal reflex, and uvula
to the right side. Angiography examination indicated that the mass
was a pseudoaneurysm (size, 5.8×3.7 cm). Subsequently, angioplasty
was performed by implanting one Wallstent 10–37 mm and two
Wallstent 10–31 mm (Boston Scientific Corporation, Natick, MA,
USA). However, the mass continued to increase in size gradually.
After 2 months, the patient received a further angioplasty, and the
implantation of two Wallgraft 10–50 mm, one Wallgraft 8–50 mm and
one Wallgraft 12–50 mm (Boston Scientific Corporation). Subsequent,
ultrasound examination detected no blood flow to the
pseudoaneurysm. After 2 months, the mass was ulcerated and the
patient was rehospitalized for ulceration. One month subsequent to
this, the patient succumbed to a skin ulcer located on the
neck.
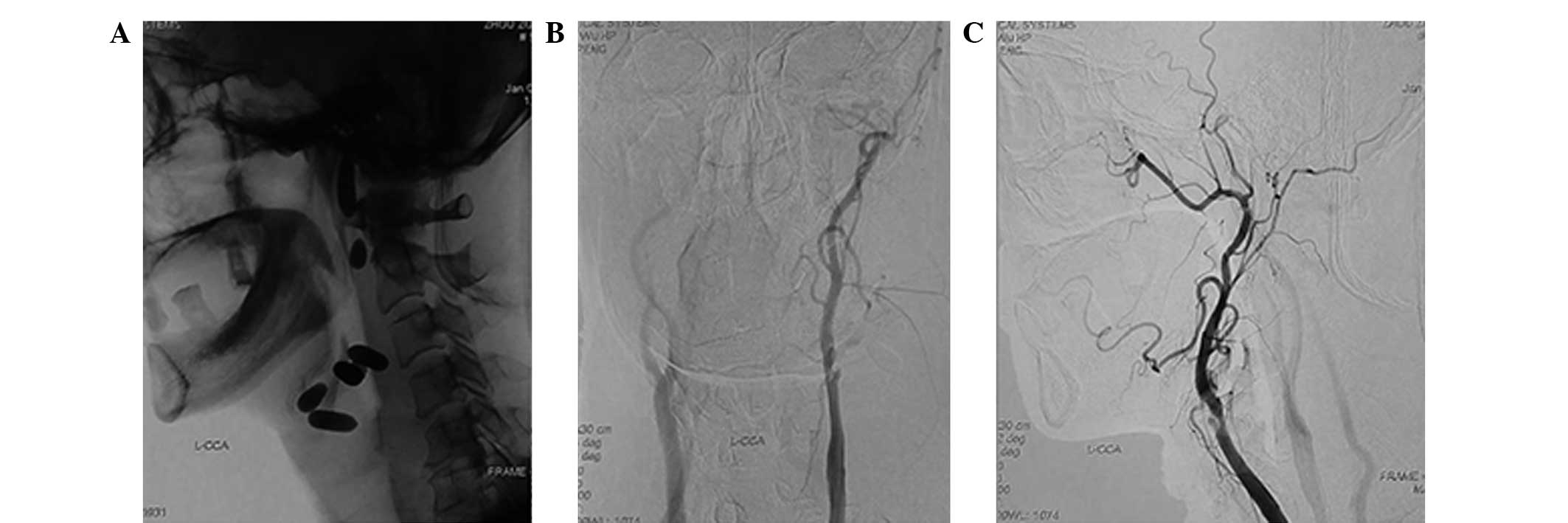
Case 3
The patient was a 59-year-old man that presented
with a left-sided cervical mass and complained of hoarseness for 1
month. The patient had no history of trauma, infection or any
previous surgical intervention. Physical examination revealed a
pulsatile mass in the left-sided cervical region (Fig. 1). The patient was diagnosed with an
aneurysm in the carotid artery using preoperative computed
tomography angiography (Fig. 2).
Angiography revealed that the mass was a pseudoaneurysm (size,
5.4×4.6 cm) and a balloon occlusion test (BOT) was negative. Two
detachable balloons (Balt Extrusion) were implanted in the distal
internal carotid artery, and three detachable balloons were
implanted in the pseudoaneurysm. However, the mass continued to
increase in size gradually. After 1 month, the patient received
balloon occlusion in the proximal portion of the external carotid
artery and common carotid artery (Fig.
3). Ultrasound examination indicated no blood flow into the
pseudoaneurysm; 1 month later, the mass was ulcerated (Fig. 4).
Case 4
The patient was an 82-year-old woman that presented
with a left-sided cervical mass and complained of hoarseness for 1
month. The patient reported no history of trauma, infection or any
previous surgical intervention. Physical examination revealed a
pulsatile mass in the left-sided cervical region. Angiography and
ultrasound examination indicated that the mass was a pseudoaneurysm
(size, 4.0×2.8 cm). Subsequently, a total aneurysmectomy with
end-to-end oblique anastomosis was performed under general
anesthesia. Subsequently, the patient made an uneventful
postoperative recovery.
Discussion
Cooper reported the first treatment for ECAA by
proximal ligation in 1808 (9).
However, the rates of stroke and mortality for this procedure were
found to be ~25 and 20%, respectively (6). In 1956, the first successful resection
of an aneurysm combined with reconstruction of the parent artery
was conducted and accepted as the standard treatment (12,13).
Subsequently, the rates of mortality and neurological incidence
reduced to 2.2–6.0% and 5.5–10%, respectively (1,11,14).
To date, the ideal method of open surgery or
endovascular stenting for ECAA has not been identified. Open
surgery is generally accepted to be the preferred method of
treatment for an extracranial carotid aneurysm, in order to prevent
thromboembolic events. However, it is considered to have a high
co-morbidity of cranial nerve deficit, of 2.2–44% (7,14).
Therefore, numerous studies have investigated the use of less
invasive therapies, including coil embolization, implantation of
uncovered stents and stent-grafts, and have advocated the use of
endovascular therapy as an alternative treatment (15–17). Li
et al (18) reviewed 224
patients and observed that the rate of procedure success was 92.8%,
the incidence of stroke was 1.8% and in-hospital mortality was
4.1%. Li et al concluded that endovascular stenting was
technically feasible, with high procedure success and a relatively
low complication rate in patients with ECAA. Endovascular stenting
is minimally invasive, thus avoiding general anesthesia and cranial
nerve deficit. Furthermore, the treatment is not limited by the
location of the aneurysm, as surgical interventions may be.
However, endovascular stenting is associated with a high rate of
complications, including early thrombosis, late stenosis and the
occlusion of the stent graft. For example, Li et al
(18) reported that occlusion
occurred in 6.3% of the examined patients.
Occlusion of the carotid artery using ligation
results in high morbidity and mortality during follow-up (6). In the presently described cases, 3
patients underwent occlusion with detachable balloons. One patient
had cerebral infarction, which led to hemiplegia. Two patients
developed ulcers on the skin of the neck, and one of these patients
succumbed to this condition. One patient was treated by surgical
repair with end-to-end anastomosis.
Each type of treatment exhibits advantages and
disadvantages. The endovascular intervention consists of carotid
artery stenting and balloon occlusion. The advantage of carotid
artery stenting is that it facilitates the maintenance of blood
flow. However, the clinical cure rate associated with this
treatment is low, which may lead to subsequent difficulty in
resecting the aneurysm. Furthermore, this method is not able to
restore nervous system function. For example, the case 2 patient
was implanted with 7 stents. Unfortunately, the aneurysm retained
blood flow. Prior to balloon occlusion, the results of a BOT should
be negative. Few studies have investigated the effect of the timing
of resection of an aneurysm on patient outcome, immediately resect
it or after vessel wall and balloon growing together. The advantage
of open surgery is that the surgical repair with end-to-end
anastomosis is conducted under direct observation. However, the
control of bleeding remains a challenge for surgeons. Therefore,
the proximal and distal ends of aneurysm require direct
observation.
Acknowledgements
This study was supported by a grant from the
National 12th Five-Year Science and Technology Support Plan Project
(no. 2011BAI08B00).
References
|
1
|
El-Sabrout R and Cooley DA: Extracranial
carotid artery aneurysms: Texas Heart Institute experience. J Vasc
Surg. 31:702–712. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
McCollum CH, Wheeler WG, Noon GP and
DeBakey ME: Aneurysms of the extracranial carotid artery.
Twenty-one years' experience. Am J Surg. 137:196–200. 1979.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Welling RE, Taha A, Goel T, Cranley J,
Krause R, Hafner C and Tew J: Extracranial carotid artery
aneurysms. Surgery. 93:319–323. 1983.PubMed/NCBI
|
|
4
|
Tabata M, Kitagawa T, Saito T, Uozaki H,
Oshiro J, Miyata T and Shigematsu H: Extracranial carotid aneurysm
in Takayasu's arteritis. J Vasc Surg. 34:739–742. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Smith BL, Munschauer CE, Diamond N and
Rivera F: Ruptured internal carotid aneurysm resulting from
neurofibromatosis: Treatment with intraluminal stent graft. J Vasc
Surg. 32:824–8. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
McCann RL: Basic data related to
peripheral artery aneurysms. Ann Vasc Surg. 4:411–414. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rosset E, Albertini JN, Magnan PE, Ede B,
Thomassin JM and Branchereau A: Surgical treatment of extracranial
internal carotid artery aneurysms. J Vasc Surg. 31:713–723. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Szopinski P, Ciostek P, Kielar M, Myrcha
P, Pleban E and Noszczyk W: A series of 15 patients with
extracranial carotid artery aneurysms: Surgical and endovascular
treatment. Eur J Vasc Endovasc Surg. 29:256–261. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cooper A: Account of the first successful
operation performed on the common carotid artery for aneurysm, in
the year 1808, with the post-mortem examination in the year 1821.
Guys Hosp Rep. 1:53–59. 1836.
|
|
10
|
Zhou W, Lin PH, Bush RL, Peden E, Guerrero
MA, Terramani T, Lubbe DF, Nguyen L and Lumdsen AB: Carotid artery
aneurysm: Evolution of management over two decades. J Vasc Surg.
43:493–497. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Srivastava SD, Eagleton MJ, O'Hara P,
Kashyap VS, Sarac T and Clair D: Surgical repair of carotid artery
aneurysms: A 10-year, single-center experience. Ann Vasc Surg.
24:100–105. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Dimtza A: Aneurysms of the carotid
arteries; report of two cases. Angiology. 7:218–227. 1956.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Longo GM and Kibbe MR: Aneurysms of the
carotid artery. Semin Vasc Surg. 18:178–183. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Radak D, Davidović L, Vukobratov V,
Ilijevski N, Kostić D, Maksimović Z, Vucurević G, Cvetkovic S and
Avramov S: Carotid artery aneurysms: Serbian multicentric study.
Ann Vasc Surg. 21:23–29. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Patel JV, Rossbach MM, Cleveland TJ,
Gaines PA and Beard JD: Endovascular stent-graft repair of
traumatic carotid artery pseudoaneurysm. Clin Radiol. 57:308–311.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Klein GE, Szolar DH, Raith J, Frühwirth H,
Pascher O and Hausegger KA: Posttraumatic extracranial aneurysm of
the internal carotid artery: Combined endovascular treatment with
coils and stents. AJNR Am J Neuroradiol. 18:1261–1264.
1997.PubMed/NCBI
|
|
17
|
Smith BL, Munschauer CE, Diamond N and
Rivera F: Ruptured internal carotid aneurysm resulting from
neurofibromatosis: Treatment with intraluminal stent graft. J Vasc
Surg. 32:824–828. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Li Z, Chang G, Yao C, Guo L, Liu Y, Wang
M, Liu D and Wang S: Endovascular stenting of extracranial carotid
artery aneurysm: A systematic review. Eur J Vasc Endovasc Surg.
42:419–426. 2011. View Article : Google Scholar : PubMed/NCBI
|