Introduction
Ectopic splenic autotransplantation (ESAT) following
splenectomy or trauma may occasionally be encountered in clinical
practice; however, clinicians or general radiology practitioners
often find the diagnosis of this condition challenging (1–4). The
majority of ESAT cases have no clinical symptoms and it is
difficult to diagnose the exact incidence rate. Computed tomography
(CT), ultrasound or magnetic resonance imaging are not specifically
designed for the diagnosis of ESAT, and certain patients are
misdiagnosed and undergo surgery. However, radionuclide spleen
imaging has the potential of being a more specific diagnostic
method for ESAT and may avert surgery. The present study reports a
case of ESAT, which was diagnosed using radionuclide splenic
imaging. Written informed consent was obtained from all
participants.
Case report
A 41-year-old male patient was admitted to the
General Hospital of Guangzhou Military Command (Guangzhou, China)
due to upper abdominal pain persisting for 12 h. The patient had
been involved in a traffic collision and had undergone a splenic
resection 10 years prior, which were hypothesized to have been
associated with the symptoms. Physical examination revealed a 15-cm
longitudinal and transverse operational incision scar, abdominal
tenderness and rebound tenderness, with a negative Murphys
sign.
Laboratory examination
The laboratory examination results were as follows:
White blood cell count, 2.1×1010 cells/l; neutrophils,
84.6%; serum amylase, 246 U/l; serum lipase, 407 U/l;
carcinoembryonic antigen, 2.27 g/ml; α-fetoprotein, 6.17 mg/l; and
CA199, 22.47 U/ml. These results were within normal ranges,
indicating that it was unlikely that the patients symptoms were
tumor-related.
Positron emission tomography (PET)/CT
scanning
The CT scan showed that the patient suffered from
acute pancreatitis, severe fatty liver and small gallstones, and
there were foci in S3 and S6 of the liver and multiple
space-occupying foci in the ascending colon. The PET/CT scan showed
the following: i) Multiple soft-tissue shadows in the abdominal
cavity, peritoneum and Glisson's capsule, which were suggested to
be benign lesions, since no metabolic disorder was observed; ii) a
small area of low-density shadows near the tail of the pancreas,
which was considered to be inflammation, since the metabolic
activity was mildly increased in that area; iii) multiple shadows
of enlarged lymph nodes around the porta hepatis and pancreas, with
a mildly increased metabolic activity; iv) absence of the spleen,
since splenectomy had been performed (Fig. 1).
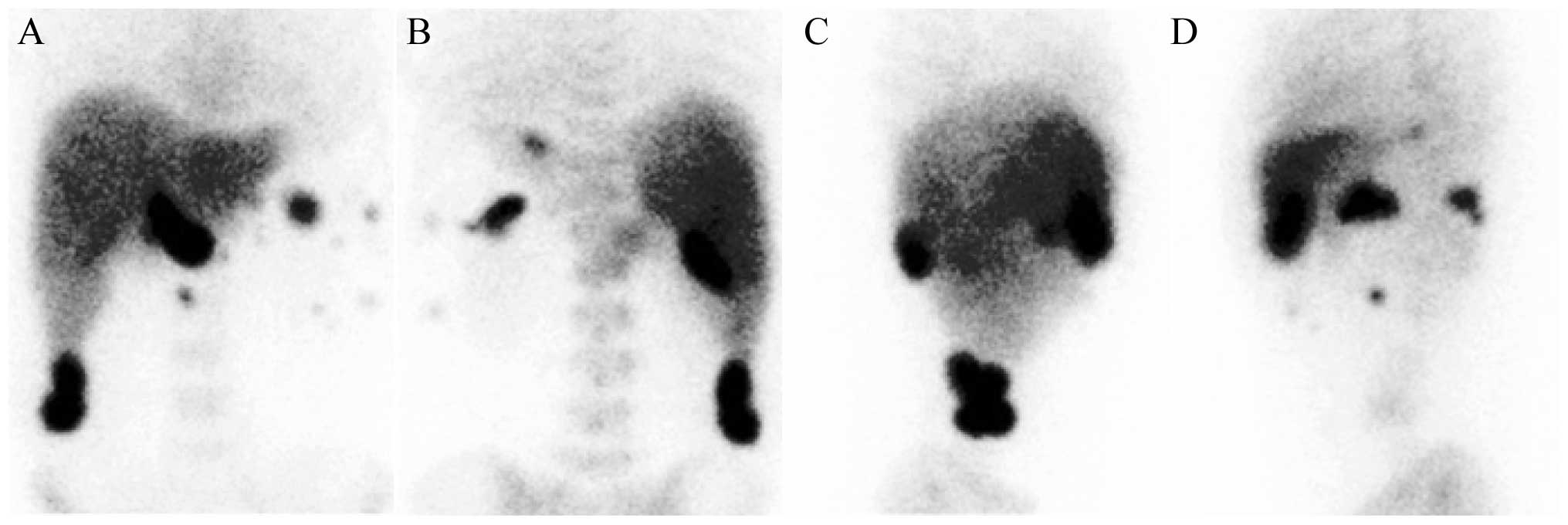
Radionuclide imaging
The spleen was absent from its normal position
(following splenectomy), but abnormal phagocytosis of multiple red
blood cells was observed in the abdomen, which was considered to be
ESAT (Fig. 2).
Clinical diagnosis
The patient was diagnosed with acute pancreatitis,
cholecystitis with gallstones, fatty liver and ESAT following
splenectomy. The patient subsequently recovered well after
receiving antipyretic analgesics and rehydration therapy..
Discussion
ESAT refers to the spontaneous transplantation of
splenic tissue following injury or splenectomy. ESAT may occur in
various sites, such as the chest, pelvic cavity or subcutaneous
tissue, but is mainly found in the abdominal cavity (5–7). In the
majority of cases, ESAT is asymptomatic and does not affect any
physiological function; therefore, intervention is usually not
required (8). In the present case,
the patient presented with acute pancreatitis and ESAT was detected
accidentally; it did, however, affect clinical diagnosis to a great
extent, as ESAT is easily misdiagnosed as a tumor. Conventional
radionuclide splenic imaging is a method specific for the diagnosis
of ESAT, and in the present case it proved to be more
diagnostically significant compared with PET/CT.
References
|
1
|
Oda J, Tachikawa N and Suda T: A solid
mass in pelvic region. Gastroenterology. 137:e9–e10. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wallace S, Herer E, Kiraly J, Valikangas E
and Rahmani R: A wandering spleen: Unusual cause of a pelvic mass.
Obstet Gynecol. 112:478–480. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Fiquet-Francois C, Belouadah M, Ludot H,
et al: Wandering spleen in children: Multicenter retrospective
study. J Pediatr Surg. 45:1519–1524. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bouassida M, Sassi S, Chtourou MF, et al:
A wandering spleen presenting as a hypogastric mass: Case report.
Pan Afr Med. J11:312012.
|
|
5
|
Di Crosta I, Inserra A, Gil CP, Pisani M
and Ponticelli A: Abdominal pain and wandering spleen in young
children: The importance of an early diagnosis. J Pediatr Surg.
44:1446–1449. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dirican A, Burak I, Ara C, Unal B, Ozgor D
and Meydanli MM: Torsion of wandering spleen. Bratisl Lek Listy.
110:723–725. 2009.PubMed/NCBI
|
|
7
|
Tseng CA and Chou AL: Images in clinical
medicine. Pelvic spleen. N Engl J Med. 361:12912009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dillman JR and Strouse PJ: Clinical image.
The ‘wandering’ spleen. Pediatr Radiol. 40:2312010. View Article : Google Scholar : PubMed/NCBI
|