Introduction
Pilocytic astrocytoma (PA) is a rare, slow-growing
glioma, which is classified as grade I by the World Health
Organization and typically occurs in children and young adults
(1). PA is the most common glial
neoplasm in children. Only one-third of PA patients are >18
years of age and only 17% are >30 years of age, with 50% of
tumors being supratentorial in adults (2). The most common occurrence sites include
the region around the third ventricle and the cerebellum. However,
the entire neuraxis can be affected, with prevalence in the
hypothalamus, thalamus, optical chiasma and nerve, brainstem,
cerebellum, cerebral hemispheres and basal ganglia (3–5).
Cervicomedullary PA has been rarely reported, and the disease is
frequently misdiagnosed due to its rarity. There are no clinical
features that are unique to PA. Signs and symptoms usually persist
for a number of months, and may differ depending on the size,
location and presence of associated hydrocephalus. Patients with PA
typically exhibit an extremely high survival rate of >90% at 10
years of age (6). The present study
reported the case of a 48-year-old patient with cervicomedullary PA
that was successfully treated. The study aims to share our clinical
experience on this disease. In addition, this patient may be the
eldest PA case ever reported.
Case report
A 48-year-old woman was admitted to the Shanghai
10th People's Hospital (Shanghai, China) in May 2014, complaining
of numbness and pain of the right limbs that persisted for >10
years and was aggravated for 1 month. No significant medical
history was reported, such as any head traumas, and the patient's
family history was unremarkable. Physical examination demonstrated
that the myodynamia of the right limbs was approximately of grade 5
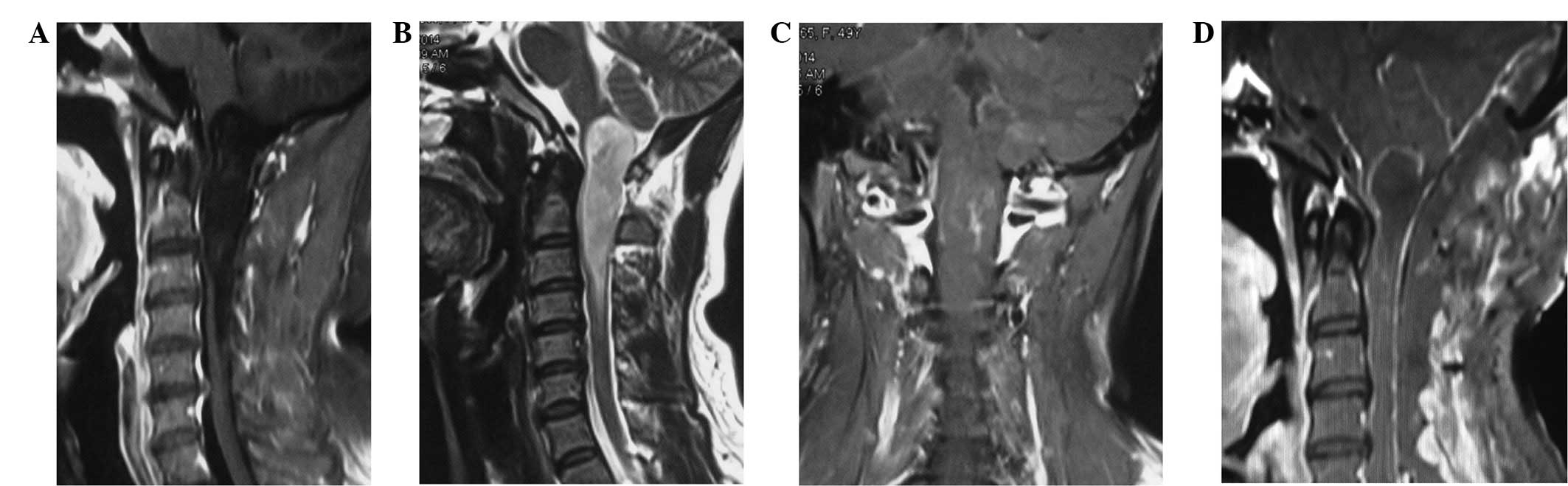
according to the Lovett Standard (7). A magnetic resonance imaging (MRI)
examination showed a sharp cervicomedullary mass extending from the
lower medulla to the cervical vertebra C3 level. The mass was
hypointense on T1-weighted images (Fig.
1A), compared with the grey or white matter, and hyperintense
on T2-weighted images (Fig. 1B). In
addition, the mass was enhanced heterogeneously subsequent to
contrast agent administration (Fig.
1C). All laboratory tests performed, including blood, urine and
coagulation analyses, along with biochemical serum analyses
(electrolytes, protein levels, urea, creatinine, glucose,
cholesterol and liver enzymes), were found to be normal. In
addition, a chest X-ray scan appeared to be normal. Written
informed consent was obtained from the patients family.
The evident clinical symptoms and a definite mass
lesion in the cervicomedulla, with a primary diagnosis being glioma
of low grade, indicated that surgical excision was required.
Following sufficient preoperative preparation, the patient
underwent a surgical treatment. Intraoperatively, the medulla and
upper cervical cord (between cervical vertebra C1 and C3) were
found to be well-stacked. Immediately after ingression into the
spinal cord along the dorsal median sulcus, the tumor mass was
detected. The mass had a gray fish-like appearance, moderate blood
supply and a clear boundary. After intratumoral decompression,
total excision was achieved (Fig.
1D).
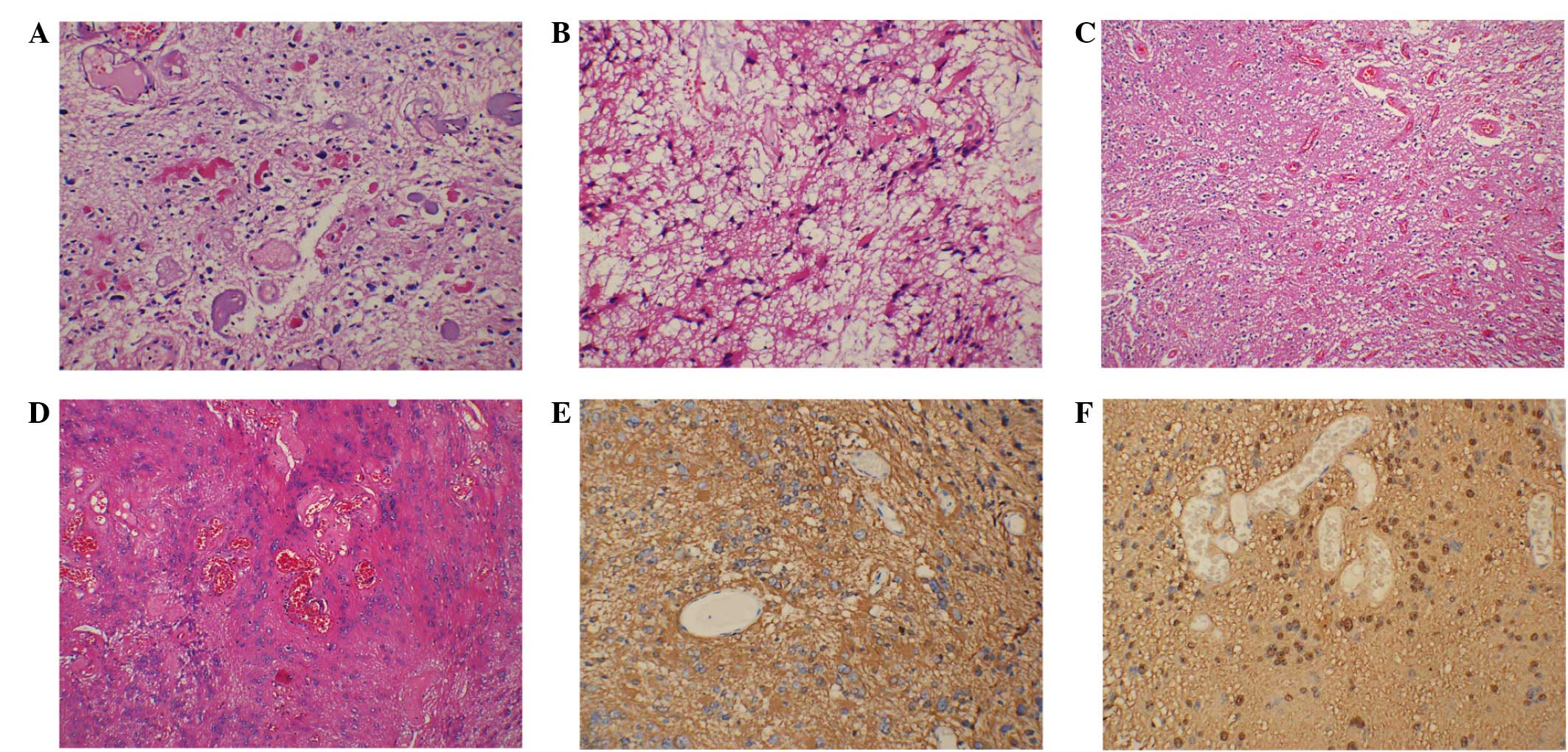
Following histopathological examination, the tumor
was confirmed to be PA. At high magnification, typical histology
characteristics, including Rosenthal fibers, a loose area, an
oligodendroglioma-like honeycomb cell area and braid-like vessels,
were evident (8).
Immunohistochemical staining was performed and the tumor cells were
found to be positive for glial fibrillary acidic protein and S-100
protein (Fig. 2).
Postoperatively, the vital signs of the patient were
closely monitored, particularly the patient's breathing. The
tracheal intubation was removed only after the breathing was
confirmed to be stable and vigorous, and the cough reflex was
nearly normal (~24 h after surgery). Following discharge, the
patient did not suffer from any symptoms at the lower cranial
nerves. As PA is a benign type of lesion, no postoperative
radiotherapy or chemotherapy was required. At 3 months after the
operation (August 2014), the myodynamia of the right limbs was
comparable to that prior to the operation.
Discussion
A lesion located in the cervicomedullary junction
affects the brainstem, the cervical cord or both regions, depending
on its extent and pathology. Involvement of the brainstem is
manifested as cranial nerve palsies, decreased respiratory drive
and long tract signs, which may result in the tumor being
unresectable (8). However, the
pathological nature of a cervicomedullary tumor has a great
influence on the disease prognosis. For instance, in the case of a
PA tumor, complete resection is often curative. Therefore, careful
study of preoperative MRI scans is required. In general, the cystic
part of PA lesions displays hypointensity on T1-weighted images and
hyperintensity in T2-weighted MRI images. In the solid part of PA,
MRI scans reveal a T1-weighted isointense or slightly hypointense
signal, with or without contrast enhancement; by contrast, on
T2-weighted scans, the lesions exhibit slight hyperintensity or
mixed signals (9). Absence of
peritumoral edema is one of the characteristics of PA. Combining
these radiological characteristics and the slow onset of the
disease, a diagnosis of PA may be considered. Surgical resection
remains the first choice of treatment against PA.
In the present case, the tumor mass was carefully
removed intraoperatively under a microscope through intratumoral
depression, with the least disturbance of the surrounding nerve
tissue. During surgery, PA patients are at a high risk of
developing bradycardia, and thus monitoring of cardiovascular and
respiratory parameters is advocated to detect changes in brainstem
function that may result from surgical handling (10). The nucleus tractus solitarius (NTS)
and the reticular formation situated in the caudal dorsal medulla
are responsible for the cardiac rhythm unsteadiness (11). Even light stimulation of these
structures by bipolar forceps during surgery can result in acute
hypotension and bradycardia. The middle and caudal regions of the
NTS have been reported to represent the sites where afferent nerves
mediating cardiovascular and respiratory reflexes make their
primary synapse (12). All these
regions should be monitored and treated with care during surgery.
For patients with a residual tumor, additional management
approaches are required, including observation and a combination of
surgery, chemotherapy and radiotherapy.
Acknowledgements
The current research was supported by a grant from
the National Natural Science Foundation of China (no.
81101909).
References
|
1
|
Tibbetts KM, Emnett RJ, Gao F, Perry A,
Gutmann DH and Leonard JR: Histopathologic predictors of pilocytic
astrocytoma event-free survival. Acta Neuropathol. 117:657–665.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Burkhard C, Di Patre PL, Schüler D,
Schüler G, Yaşargil MG, Yonekawa Y, Lütolf UM, Kleihues P and
Ohgaki H: A population-based study of the incidence and survival
rates in patients with pilocytic astrocytoma. J Neurosurg.
98:1170–1174. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Forsyth PA, Shaw EG, Scheithauer BW,
OFallon JR, Layton DD Jr and Katzmann JA: Supratentorial pilocytic
astrocytomas: A clinicopathologic, prognostic, flow cytometric
study of 51 patients. Cancer. 72:1335–1342. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Katsetos CD and Krishna L: Lobar pilocytic
astrocytomas of the cerebral hemispheres: I. Diagnosis and
nosology. Clin Neuropathol. 13:295–305. 1994.PubMed/NCBI
|
|
5
|
Brat DJ and Burger PC: Cerebral pilocytic
astrocytoma: Distinction from infiltrating fibrillary astrocytomas.
Pathol Case Rev. 3:290–295. 1998. View Article : Google Scholar
|
|
6
|
Cyrine S, Sonia Z, Mounir T, Badderedine
S, Kalthoum T, Hedi K and Moncef M: Pilocytic astrocytoma: A
retrospective study of 32 cases. Clin Neurol Neurosurg.
115:1220–1225. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dyck PJ, Boes CJ, Mulder D, Millikan C,
Windebank AJ, Dyck PJ and Espinosa R: History of standard scoring,
notation, and summation of neuromuscular signs. A current survey
and recommendation. J Peripher Nerv Syst. 10:158–173. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nair AP, Mehrotra A, Das KK, Srivastava
AK, Sahu RN and Kumar R: Clinico-radiological profile and nuances
in the management of cervicomedullary junction intramedullary
tumors. Asian J Neurosurg. 9:21–28. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chourmouzi D, Papadopoulou E,
Konstantinidis M, Syrris V, Kouskouras K, Haritani A, Karkavelas G
and Dresvelegas A: Manifestations of pilocytic astrocytoma: A
pictorial review. Insights Imaging. 5:387–402. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Endo T, Sato K, Takahashi T and Kato M:
Acute hypotension and bradycardia by medulla oblongata compression
in spinal surgery. J Neurosurg Anesthesiol. 13:310–313. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lawrence AJ and Jarrott B: Neurochemical
modulation of cardiovascular control in the nucleus tractus
solitarius. Prog Neurobiol. 48:21–53. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Horiuchi J, Potts PD, Polson JW and
Dampney RA: Distribution of neurons projecting to the rostral
ventrolateral medullary pressor region that are activated by
sustained hypotension. Neuroscience. 89:1319–1329. 1999. View Article : Google Scholar : PubMed/NCBI
|