Introduction
Diabetic foot is a common complication of diabetes.
In patients with diabetic foot ulcers, numerous factors can lead to
the slow growth of the local wound granulation tissue, such as
increased blood glucose (locally and systemically), inefficient
wound angiogenesis and fibrous tissue deposition (1,2).
Clinical and animal experiments have indicated that local treatment
with insulin may improve wound healing in diabetes (3–5). A
previous animal study demonstrated that insulin could reduce
inflammation and increase collagen deposition, thus inducing
accelerated burn wound healing (6).
In addition, insulin injected diffusely into the wound can
accelerate wound re-epithelialization (7–10). This
may be caused by insulin promoting protein synthesis and suggests
that insulin may play a role in the process of wound healing. Local
use of insulin in the treatment of refractory wounds has been
widely studied; however, the effective concentration and the safe
dose of insulin are not clear.
The disorder and loss of function of angiogenesis in
diabetic ulcer wounds are considered to be the dominating factors
leading to poor wound healing (11–13).
Restoring the function and structure of the vasculature and
improving angiogenesis are currently the key problems to be solved
for wound healing in patients. CD34 is a type-I phosphorylated
transmembrane glycoprotein and a marker of vascular endothelial
cells. Due to its high expression levels in new blood vessels, CD34
is additionally an important indicator of angiogenesis. Anti-CD34
antibody can be used to successfully distinguish new blood vessels
from mature vessels (14).
Microvessel density (MVD), which is calculated based on the
expression of CD34, represents a quantitative indicator of
angiogenesis. As a result, curative effects in cases of diabetic
foot can be assessed by detecting the expression of CD34 and
calculating the MVD.
The aim of the present study was to investigate the
effect of local insulin injection on granulation tissue formation
in the wounds of patients with diabetic foot ulcer. The curative
effects and safe dose of local insulin injection were also
evaluated.
Materials and methods
Patients
The 32 patients enrolled in this study were
hospitalized in the Department of Burns of the People's Hospital of
Xinjiang Uygur Autonomous Region (Urumchi, China) between June 2010
and June 2013. Among these patients were 22 men and 10 women. The
age of the patients ranged from 42 to 83 years, with the mean age
of 67.12±2.65 years. The patients all had diabetes, and the
duration of diabetes was 5–20 years (mean, 7.52±1.33 years). The
fasting fingertip blood glucose level, as determined by the
OneTouch® blood glucose meter (Johnson & Johnson, Rochester,
NY, USA), ranged from 5.7 to 8.6 mmol/l (mean, 6.66±1.19 mmol/l).
The duration of ulcers (gangrene) was 12–160 days (mean,
122.36±34.5 days). Certain cases were complicated by diabetic
nephropathy, retinopathy and cardiovascular disease (such as
coronary heart disease, hypertension and cerebral infarction). The
inclusion criteria for the patients were as follows: i) Patients
who were diagnosed with diabetic foot according to the 2010 Edition
of the Clinical Practice Guidelines for the Prevention and
Management of Diabetes Foot Complications (edited by the American
Diabetes Association) (6); ii)
voluntary participants who were able and willing to participate in
the study; iii) patients who had relatively stable blood glucose
levels, without the influence of diet, exercise, infection, stress
or other factors that could affect systemic blood glucose; and iv)
patients who exhibited yellow wounds without significant growth of
granulation tissue. The exclusion criteria were as follows: i)
Patients who succumbed during the treatment; ii) patients who
exhibited extensive and complete necrosis in the body and required
immediate amputation at the time of admission to hospital; iii)
patients who were discharged early or discontinued the therapy. Six
patients were excluded from the present study. Written informed
consent was obtained from all patients enrolled in the study prior
to them undergoing the examination. The study protocol was approved
by the Ethics Committee of the People's Hospital of Xinjiang Uygur
Autonomous Region.
Wound treatment
The eschar and necrotic tissue attached to the wound
was removed. As a support for late repair, the tendons and nerves
without obvious liquefactive necrosis were reserved, and soft
tissues were retained to the greatest extent possible. To avoid the
effect of the drug on the local blood glucose level, all the wounds
were cleaned with physiological saline.
Grouping and sample collection
The 32 patients enrolled in this study were randomly
allocated to either the insulin group (n=18) or the control group
(n=14). In the insulin group, one-half of the calculated dose of
isophane protamine biosynthetic human insulin (premixed 30:70; Novo
Nordisk Pharmaceutical Industries, Inc., Clayton, NC, USA) was
diluted with physiological saline to a total volume of 1 ml and was
then injected diffusely into the base of the diabetic foot ulcer.
The remaining half dose of insulin was subcutaneously injected into
the abdominal wall. The insulin injection was performed twice a
day. In the control group, the calculated dose of human insulin was
subcutaneously injected into the abdominal wall and 1 ml normal
saline was subcutaneously injected into the base of the diabetic
foot ulcer. The injection was performed twice a day. Both groups
received injections for 7 consecutive days.
On days 0, 5, 7 and 12 after injection, wound tissue
measuring 0.5×0.5 cm was collected from each patient. The wound
tissues were fixed with 10% formaldehyde for immunohistochemical
assay. The observation period ended 12 days after injection.
Blood glucose measurement
Following debridement, the fasting fingertip blood
glucose levels of the two groups were measured using the OneTouch
blood glucose meter (Johnson & Johnson). At 0.5, 1.0, 2.0 and
4.0 h after injection each day, the fasting fingertip blood glucose
levels of the two groups were also determined, and the measurements
and injections were conducted for 7 days.
Granulation tissue assessment
The degree of granulation tissue growth was
evaluated according to a method described in a previous study
(15). Briefly, prior to treatment,
the original ulcer wound areas of the two groups were recorded
using transparent tracing paper. The wound size was traced with the
same method following treatment. The growth of the granulation
tissue was calculated using Photoshop CS 8.0 software (Adobe
Systems, Inc., San Jose, CA, USA). The formula used was as follows:
Granulation tissue growth = (Original wound area - wound area
without granulation coverage)/original wound area × 100%.
Immunohistochemical staining
All specimens were fixed with 10% paraformaldehyde
for 48 h and embedded in paraffin. Paraffin-embedded tissue was
sliced continuously into 4-µm sections and stained with hematoxylin
and eosin. To achieve this, slides were deparaffinized and
rehydrated. Endogenous peroxidase was blocked with 3% hydrogen
peroxide in methanol for 10 min at 37°C. Subsequently, the sections
were washed with distilled water, and antigen retrieval was
performed by boiling with antigen retrieval solution (GeneTex,
Inc., Irvine, CA, USA for 1–4 min. Nonspecific binding was blocked
by incubating the slides with goat serum for 30 min at 37°C.
Primary rabbit anti-CD34 antibody (1:500; cat. no. D&M-2038R:
Beijing Bioss Biological Technology Co., Ltd., Beijing, China) was
added for incubation overnight at 4°C. The sections were then
washed with Tris-buffered saline containing 0.1% Tween and
incubated with biotin-labeled secondary antibodies for 30 min at
room temperature, and horseradish peroxidase-labeled streptavidin
was added for incubation for 30 min at 37°C. Immunoreactivity was
visualized using the chromogen 3,3′-diaminobenzidine and terminated
with distilled water. The sections were then counterstained with
hematoxylin, differentiated with hydrochloric acid ethanol,
dehydrated with gradient alcohol and xylene and mounted onto
coverslips. In the negative control, phosphate buffer was used
instead of the primary antibody. Samples were observed under a
light microscope. Cells with brown staining in the cytoplasm, the
nucleus or both were considered to be positive. The Axioskop 2 Plus
microscopy and image analysis system (Carl Zeiss Microscopy GmbH,
Jena, Germany) was used for the analysis of CD34 expression, and
the method of Pareek et al (14) was used for MVD calculation. Briefly,
at each time-point, 3 sections per groups were taken and observed
under the microscope. Cells with brown granules were considered to
be positive for CD34. Brown-stained single endothelial cells or
cell clusters were considered as a vessel count. The 3 regions with
highest MVD at low magnification (×40) and 5 regions with the
highest MVD at high magnification (×200) were taken and the average
number was used as the MVD value.
Statistical analysis
The statistical analyses were performed using SPSS
version 10.0 (SPSS Inc., Chicago, IL, USA) for Windows. The t-test
was conducted to calculate the statistical significance between the
groups. P<0.01 was considered to indicate a statistically
significant difference.
Results
Changes in fingertip blood glucose
levels in the groups at different time-points after insulin
injection
To determine the effect of local insulin injection
on the systemic blood, fingertip blood glucose detection was
performed. As shown in Table I, the
fasting blood glucose levels in the two groups were maintained at
6.7–12.1 mmol/l (mean 9.95±2.21 mmol/l) before and after insulin
injection. No significant difference in blood glucose level was
found between the two groups before the injection or at 0.5, 1.0,
2.0 and 4.0 h after injection. Local insulin injection in the wound
had a marked effect on the systemic blood glucose levels: The blood
glucose showed a notable decrease 1–2 h after the injection of
insulin and then gradually returned to the pre-injection level at 4
h after injection (Table I). This
indicated that local wound insulin injection had a marked effect on
systemic blood glucose and could achieve the purpose of lowering
blood glucose.
 | Table I.Changes in the fingertip blood glucose
level in the two groups prior to and following insulin
injection. |
Table I.
Changes in the fingertip blood glucose
level in the two groups prior to and following insulin
injection.
|
|
| Blood glucose after
insulin injection (mmol/l) |
|---|
|
|
|
|
|---|
| Group | Blood glucose before
insulin injection (mmol/l) | 0.5 h | 1.0 h | 2.0 h | 4.0 h |
|---|
| Insulin, n=18 |
11.38±0.96a |
11.06±0.65b |
9.76±0.57c |
6.65±0.18d |
11.51±0.26e |
| Control, n=14 | 12.06±0.61 | 9.34±0.19 | 9.28±0.27 | 6.66±0.30 | 11.49±0.32 |
The growth of granulation tissue
To assess the situation of wound angiogenesis,
granulation tissue growth was examined. As shown in Table II, growth of granulation tissue in
the insulin group was more marked on day 7 after injection
(24.87±0.24). Patients with this type of granulation tissue were
ready to undergo surgical treatment. Compared with the control
group at this time-point (18.6±0.45), the growth in the insulin
group was significantly different (P<0.01) (Figs. 1 and 2). This result indicated that the wound bed
preparation time of the treatment group was shorter than that of
the control group, and the wound healing of the treatment group was
enhanced.
 | Table II.Comparison of the growth of
granulation tissue in the two groups. |
Table II.
Comparison of the growth of
granulation tissue in the two groups.
| Group | 0 days (%) | 5 days (%) | 7 days (%) | 12 days (%) |
|---|
| Insulin, n=18 |
7.45±0.18a |
13.38±0.36b |
24.87±0.24c |
59.06±1.58d |
| Control, n=14 |
8.20±0.28 |
12.98±0.45 |
18.66±0.45 |
23.61±1.57 |
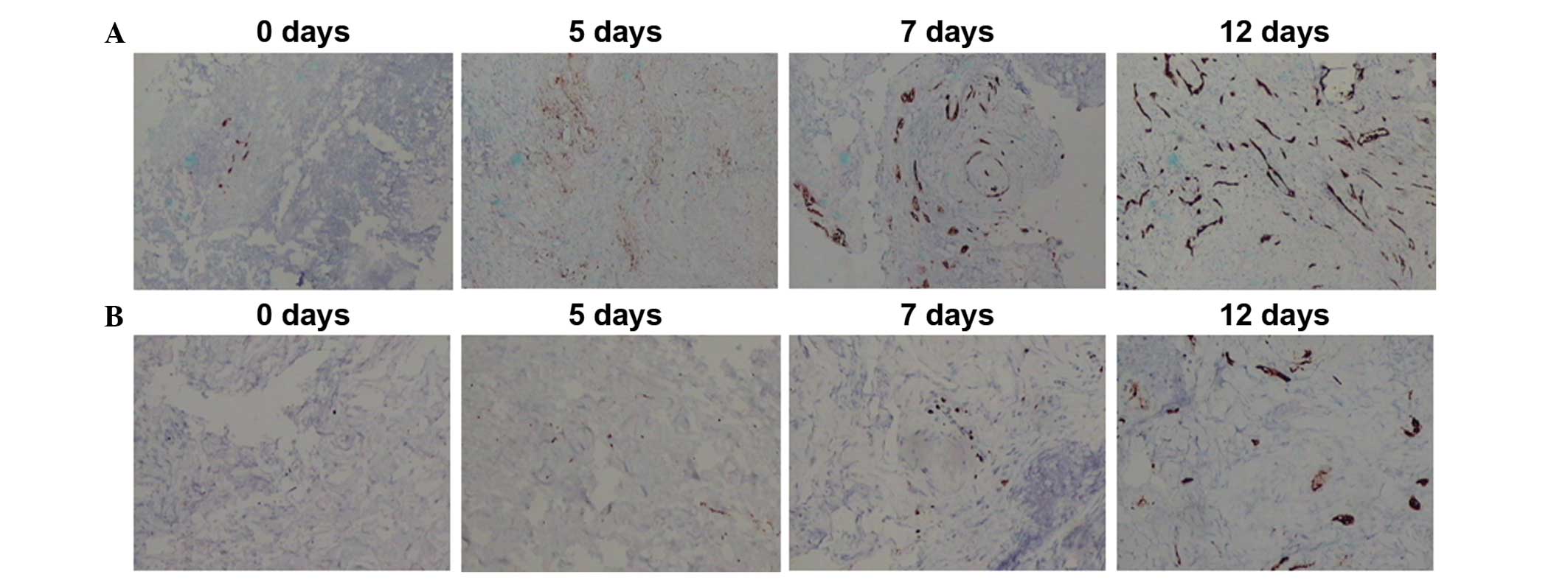
CD34 detection and MVD counting
To assess the curative effects of local insulin
injection on diabetic foot, the expression of CD34 following
insulin injection in the two groups was detected by
immunohistochemistry, and the results are shown in Fig. 3. New vessels were observed in the
insulin group at 5 days after insulin injection. The MVD was
calculated as previously described. No significant difference in
MVD was initially found between the two groups (P>0.05)
(Table III). In the insulin group,
the MVD increased rapidly from 5 days after injection, and a
significant difference was found between the two groups
(P<0.01). This result indicated that the local injection of
insulin in diabetic foot ulcers could promote the growth of
granulation tissue.
 | Table III.Comparison of microvessel density in
the two groups at different time-points (number/HP). |
Table III.
Comparison of microvessel density in
the two groups at different time-points (number/HP).
| Group | 0 days | 5 days | 7 days | 12 days |
|---|
| Insulin, n=18 | 0 |
3.45±0.19a |
8.34±0.48b |
11.22±0.97c |
| Control, n=14 | 0 |
3.43±0.14 |
4.42±0.14 |
5.44±1.13 |
Discussion
Insulin has numerous functions, such as protection
of the vascular endothelium, vascular dilation, myocardial
protection and anti-platelet aggregation and anti-atherosclerosis
effects (16,17). The local use of insulin (local wet
dressing or injection) is reported to be effective in the treatment
of refractory diabetic wounds (5);
however, the results have been obtained in animal experiments and
the insulin doses used lack a theoretical basis (18). Thus, the safety of the local use of
insulin in humans is not clear. Obstructive factors, such as the
poor permeability of insulin, wound surface exudation and tissue
necrosis, make it difficult for insulin wet packing to achieve the
desired effect. Local injection of insulin in the local wound is
more effective due to its maintenance of a high concentration and
its long duration of efficacy. In the present study, the blood
glucose level decreased significantly 1–2 h after the injection of
one-half the calculated dose of insulin. Two patients showed
symptoms of hypoglycemia, including palpitations, dizziness, pale
appearance and cold sweats. The result demonstrated that the local
injection of insulin into the wound could reduce the body blood
glucose, similar to other clinical treatments, and the injection
had a marked effect on the systemic blood glucose. This result also
suggested that local use of insulin should be individualized, in
case of the onset of systemic hypoglycemia.
The occurrence of diabetic foot is a consequence of
multiple factors, such as high glucose levels, vascular disease,
neuropathy and infections (19).
Currently, the establishment of an animal model of diabetic foot is
not completely successful. Diabetic angiopathy is a manifestation
of diabetic foot, and the artery system is the most commonly
affected organ (20). The
manifestations in the affected artery system show as plaque,
intimal thickening, stenosis and occlusion. The vein and lymphatic
systems are often normal or with minor disease signs, without
obvious obstacles in local limb blood flow. As a result, the
insulin that is locally injected into the ulcer wound can be
absorbed into the blood circulation perfectly, as if it were
injected into other parts of the body. Insulin plays the role of
lowering blood glucose, which may underlie the effect of the local
injection of insulin on systemic blood glucose (21,22).
The results of the present study showed that at 5
days after local insulin injection, the expression of CD34 and the
MVD in the insulin group began to increase; however, compared with
the control group, there was no significant difference in MVD
(P>0.05). Furthermore, no significant difference was found in
the granulation tissue growth between the two groups. Growth of
granulation tissue in the insulin group was more marked on day 7
after injection (24.87±0.24). The necrotic tissue had been shed,
and partially exposed bone and tendon had become gradually covered
by granulation tissue. These represented essential processes for
wound bed preparation. The MVD of the insulin group showed a rapid
increase at day 7 (8.34±0.48), which showed the consistency of the
histology and gross observation results.
The biological effects of local insulin injection
have been suggested to be associated with several molecular
mechanisms. First, insulin reduces the local wound blood glucose
concentration, thus reducing the damage resulting from the
accumulation of high levels of glucose metabolic intermediates
(21). Secondly, insulin is the
inhibitor of three major proinflammatory transcription factors:
Nuclear factor-κB, activator protein-1 and early growth response-1
(EGR-1). The expression of regulating monocyte chemotactic protein
1, intercellular adhesion molecule-1, matrix metalloproteinase
(MMP)-2, MMP-9, tissue factor and plasminogen activator
inhibitor-1, which are regulated by these three transcription
factors, is also inhibited by insulin (23,24).
These proteins are important components of NADPH oxidase, which
produces superoxide radicals with potent oxidative effects
(23–26), leading to the damage of the tissue
cells. In addition, insulin inhibits the transcription of three key
proinflammatory factors induced by hyperglycemia, thus inhibiting
the inflammatory response and local oxidative stress (25,27). A
third potential mechanism is that, by reducing the inflammatory
cell factor level and increasing the inflammatory cytokine level
following trauma, insulin relieves the inflammatory response and
prevents an excessive inflammatory reaction (3). Furthermore, insulin inhibits the
degradation of immune cell proteins, thus enhancing immune activity
(3). Another mechanism has been
suggested to involve the insulin-induced entry of extracellular
amino acids and K+ into the cells, which increases
protein synthesis (28), greatly
reduces the bacterial survival environment, enhances the ability of
local inflammation and thus promotes local wound healing. Insulin
additionally increases the synthesis and release of nitric oxide
(NO). Endothelial NO plays an important role in neovascularization.
Neovascularization is promoted by vascular endothelial growth
factors (VEGFs), while VEGF promotes angiogenesis (29). Finally, insulin can activate
myofibroblasts, advance the cell cycle and promote collagen
deposition, thus accelerating the wound healing process.
In the present study, it was found that local wound
insulin injection could reduce the blood glucose level, suggesting
a significant effect on systemic blood glucose by local injection.
These results provided the theoretical basis for treatment of
diabetic foot via local insulin injection; however, the association
between the dosages of insulin and the growth of granulation
tissue, together with the exact mechanism of this action, remains
to be investigated further.
Acknowledgements
This study was supported by a program of the Natural
Science Foundation Committee of Xinjiang Uygur Autonomous Region
(no. 2012211A090).
References
|
1
|
Aalaa M, Malazy OT, Sanjari M, Peimani M
and Mohajeri-Tehrani M: Nurses' role in diabetic foot prevention
and care; a review. J Diabetes Metab Disord. 11:242012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Alavi A, Sibbald RG, Mayer D, Goodman L,
Botros M, Armstrong DG, Woo K, Boeni T, Ayello EA and Kirsner RS:
Diabetic foot ulcers, Part II. Histopathology. J Am Acad Dermatol.
70:212014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Madibally SV, Solomon V and Mitchell RN:
VanD e Water L, Yarmush ML and Toner M: Influence of insulin
therapy on burn wound healing in rats. J Surg Res. 109:92–100.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lima MH, Caricilli AM, de Abreu LL, Araújo
EP, Pelegrinelli FF, Thirone AC, Tsukumo DM, Pessoa AF, dos Santos
MF, de Moraes MA, et al: Topical insulin accelerates wound healing
in diabetes by enhancing the AKT and ERK pathways: A double-blind
placebo-controlled clinical trial. PLoS One. 7:e369742012.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Martínez-Jiménez MA, Aguilar-García J,
Valdés-Rodríguez R, Metlich-Medlich MA, Dietsch LJ, Gaitán-Gaona
FI, Kolosovas-Machuca ES, González FJ and Sánchez-Aguilar JM: Local
use of insulin in wounds with diabetic patients Higher temperature,
fibrosis, and angiogenesis. Plast Reconstr Surg. 32:1015e–1019e.
2013.
|
|
6
|
American Diabetes: Association: S tandards
of medical care in diabetes - 2010. Diabetes Care. 33((Suppl 1)):
S11–S61. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhang XJ and Chinkes DL: SadagopaR
amanujam VM and Wolfe RR: Local injection of insulin-zinc
stimulates DNA synthesis in skin donor site wound. Wound Repair
Regen. 15:258–265. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zhang XJ, Wu X, Wolf SE, Hawkins HK,
Chinkes DL and Wolfe RR: Local insulin-zinc injection accelerates
skin donor site wound healing. J Surg Res. 142:90–96. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Liu Y, Zhang X, Zhang Z, Fang PY and Xu
WS: Effects of topical application of insulin on the wound healing
in scalded rats. Zhonghua Shao Shang Za Zhi. 20:98–101. 2004.(In
Chinese). PubMed/NCBI
|
|
10
|
Liu Y, Zhang X, Zhang Z and Xu WS: The
influence of topical application of insulin on the formation of
basement membrane in scalded rats. Zhonghua Shao Shang Za Zhi.
21:445–447. 2005.(In Chinese). PubMed/NCBI
|
|
11
|
Schramm JC, Dinh T and Veves A:
Microvascular change in the diabetic foot. Int J Low Extrem Wounds.
5:149–159. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Martin A, Komada MR and Sane DC: Abnormal
angiogenesis in diabetes mellitus. Med Res Rev. 23:117–145. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cho CH, Sung HK, Kim KT, Cheon HG, Oh GT,
Hong HJ, Yoo OJ and Koh GY: COMP-angiopoietin-1 promotes wound
healing through enhanced angiogenesis, lymphangiogenesis and blood
flow in a diabetic mouse model. Proc Natl Acad Sci USA.
103:4946–4951. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Pareek G, Shevchuk M, Armenakes NA,
Vasjovic L, Hochberg DA, Basillote JB and Fracchia JA: The effect
of finasteride on the expression of vascular endothelial growth
factor and microvessel density, A possible mechanism for decreased
prostatic bleeding in treated patients. J Urol. 169:20–23. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Li DL, Li QX and Peng DZ: Wound size
measurement using digital camera and Photoshop software. Zhong Hua
Shao Shang Za Zhi. 26:482010.(In Chinese).
|
|
16
|
Dandona P, Mohanty P, Chaudhuri A, Garg R
and Aljada A: Insulin infusion in acute illness. J Clin Invest.
115:2069–2072. 2005. View
Article : Google Scholar : PubMed/NCBI
|
|
17
|
Langouche L, Vanhorebeek I, Vlasselaers D,
Vander Perre S, Wouters PJ, Skogstrand K, Hansen TK and Van den
Berghe G: Intensive insulin therapy protects the endothelium of
critically ill patients. J Clin Invest. 115:2277–2286. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhang XJ, Meng C, Chinkes DL and Herndon
DN: Beneficial effects of insulin on cell proliferation and protein
metabolism in skin donor site wound. J Surg Res. 168:e155–e161.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Adam KM, Mahmoud SM, Mahadi SI, Widatalla
AH, Shawer MA and Ahmed ME: Extended leg infection of diabetic foot
ulcers, Risk factors and outcome. J Wound Care. 20:440–444. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Abolfotouh MA, Alfaifi SA and Al-Gannas
AS: Risk factors of diabetic foot in central Saudi Arabia. Saudi
Med J. 132:708–713. 2011.
|
|
21
|
Zhang ZX, Liu XL, Lü L, Zhang L, Ji DL and
Liu LH: Effect of insulin by local injection on the level of
systemic blood glucose and granulation tissue formation of wound in
patients with diabetic foot ulcer. Zhonghua Shao Shang Za Zhi.
27:451–455. 2011.(In Chinese). PubMed/NCBI
|
|
22
|
Sinwar PD: The diabetic foot management -
recent advance. Int J Surg. 15:27–30. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Dandona P, Aljada A, Mohanty P, Ghanim H,
Hamouda W, Assian E and Ahmad S: Insulin inhibits intranuclear
nuclear factor kappaB and stimulates IkappaB in mononuclear cells
in obese subjects, Evidence for an anti-inflammatory effect? J Clin
Endocrinol Metab. 86:3257–3265. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Aljada A, Ghanim H, Mohanty P, Kapur N and
Dandona P: Insulin inhibits the pro-inflammatory transcription
factor early growth response gene-1 (Egr)-1 expression in
mononuclear cells (MNC) and reduces plasma tissue factor (TF) and
plasminogen activator inhibitor-1 (PAI-1) concentrations. J Clin
Endocrinol Metab. 87:1419–1422. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Chaudhuri A, Janicke D, Wilson MF,
Tripathy D, Garg R, Bandyopadhyay A, Calieri J, Hoffmeyer D, Syed
T, Ghanim H, et al: Anti-inflammatory and profibrinolytic effect of
insulin in acute ST-segment-elevation myocardial infarction.
Circulation. 109:849–854. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Aljada A, Ghanim H, Mohanty P, Syed T,
Bandyopadhyay A and Dandona P: Glucose intake induces an increase
in activator protein 1 and early growth response 1 binding
activities, in the expression of tissue factor and matrix
metalloproteinase in mononuclear cells, and in plasma tissue factor
and matrix metalloproteinase concentrations. Am J Clin Nutr.
80:51–57. 2004.PubMed/NCBI
|
|
27
|
Wang L, Zhao X, Wei BY, Liu Y, Ma XY, Wang
J, Cao PC, Zhang Y, Yan YB, Lei W and Feng YF: Insulin improves
osteogenesis of titanium implants under diabetic conditions by
inhibiting reactive oxygen species overproduction via the PI3K-Akt
pathway. Biochimie. 108:85–93. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kimball SR, Vary TC and Jeferson LS:
Regulation of protein synthesis by insulin. Annu Rev Physiol.
56:321–348. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Papapetropoulos A, García-Cardeña G, Madri
JA and Sessa WC: Nitric oxide production contributes to the
angiogenic properties of vascular endothelial growth factor in
human endothelial cells. J Clin Invest. 100:3131–3139. 1997.
View Article : Google Scholar : PubMed/NCBI
|