Introduction
Growing evidence from experimental studies in
animals and clinical observations indicates that hepatic failure
remains a most important cause of mortality following hepatic
resection and transplantation (1–3). Hepatic
ischemia and reperfusion (I/R) injury plays an active role in this
process (4). Disordered
glycometabolism is a common phenomenon in patients with liver
disease (5). In severe cases, this
is accompanied by diabetes. The reduction of I/R injury in patients
with liver disease and diabetes is necessary. Routine strategies,
such as controlling hepatic blood flow, ischemic preconditioning
and the application of protecting agents are available (6–8).
However, the identification of a novel approach that is able to
reduce I/R injury in these patients is imperative.
Diabetic microvascular complications characterized
by barrier dysfunction and increased permeability have been linked
to the activation of protein kinase Cs (PKCs) (9). PKCs are serine/threonine kinases that
participate in cellular signal transduction in diabetes-mediated
vascular damage. Once activated, PKC is phosphorylated and
translocated to the membrane, resulting in an elevated expression
of PKC at the membrane. Ruboxistaurin (Rx) is a PKC-β inhibitor
that is highly selective for the PKC-βII isoform. Rx has been shown
to normalize endothelial function and prevent microvascular
complications (10,11). While the effects of PKC-βII
activation and the role of Rx are well understood in myocardial I/R
(12), they remain unclear in liver
I/R.
Therefore, in the present study the aims were to: i)
evaluate the effectiveness of Rx in attenuating the liver damage
and hepatic apoptotic injury induced by I/R in an rat model of
diabetes; ii) elucidate whether Rx is able to attenuate liver
microvascular dysfunction and attenuate inflammatory factor
release; and iii) investigate the mechanism(s) by which Rx may
modulate the liver damage and hepatic apoptotic injury induced by
I/R in a rat model of diabetes with a focus on PKC-βII-dependent
signaling.
Materials and methods
Animal preparation
All animal procedures were performed in accordance
with the National Institutes of Health Guidelines on the Use of
Laboratory Animals, and the study was approved by the Ethics
Committee on Animal Care of Tianjin Third Central Hospital
(Tianjin, China). Diabetes was induced in 40 male Sprague-Dawley
rats (weight 250–280 g) by a single intraperitoneal injection of
streptozotocin (STZ; 50 mg/kg in 0.9% saline; Sigma-Aldrich, St.
Louis, MO, USA). Blood glucose levels were measured after 24 h and
then daily for a total of 5 days. Animals with glucose levels ≥16.5
mmol/l were classified as diabetic. The diabetic rats were
randomized into two groups. These were an untreated group, which
did not receive any treatment (n=10) and a treatment group (n=10),
orally treated with Rx (Eli Lilly, Indianapolis, IN, USA) at a dose
of 5 mg/kg/day for 2 weeks.
Hepatic I/R
Hepatic I/R procedures were performed in the rats of
the two groups. In brief, rats were anesthetized with 3%
pentobarbital (30 mg/kg intraperitoneally) after fasting for 12 h.
Laparotomy via a middle incision exposed the liver lobes. Following
surgical exposure of the portal vein, the rats were injected with
heparin (100 U/kg) via the tail vein to prevent the formation of
blood clots during the ischemia period. The portal vein and hepatic
artery were occluded for 60 min with a metallic clamp to induce
hepatic ischemia. Blood samples were collected from the vena cava
before and 1, 3 and 5 h after I/R, prior to rapid excision of the
liver. Portions of liver tissue were fixed in 10% neutralized
formalin for histological evaluation or snap frozen in liquid
nitrogen and maintained at −80°C.
Hepatic enzyme assays
Serum levels of aspartate transaminase (AST) and
lactate dehydrogenase (LDH) were analyzed using a commercially
available diagnostic kit (BD Biosciences, Franklin Lakes, NJ, USA)
and automatic biochemical equipment (Abbott C800; Abbott
Diagnostics, Santa Clara, CA, USA). The serum levels of tumor
necrosis factor-α (TNF-α) and intercellular adhesion molecule 1
(ICAM-1) were measured using commercial enzyme-linked immunosorbent
assay (ELISA) kits (BD Biosciences) according to the manufacturer's
instructions.
Histological studies
Fixed liver specimens were embedded in paraffin,
sectioned at 4-µm thickness, and stained with hematoxylin and eosin
(H&E) for the evaluation of liver injury. Photomicrographs were
taken with a digital camera under a microscope (CKX41; Olympus
Corporation, Tokyo, Japan).
Examination of liver tissue with a
scanning electron microscope (SEM)
After fixing, tissue samples were examined via
scanning electron microscopy to assess the microvascular integrity
of the liver. After liver tissue was collected, regular
pretreatments in accordance with standard protocols were employed,
including dehydration, desiccation and gilding (13). Prepared samples were subsequently
examined with an SEM (S-3400N; Hitachi, Ltd., Tokyo, Japan).
Western blot analysis
Proteins from ischemic liver tissue were extracted
using Protein Extraction Reagent kit (Pierce Biotechnology, Inc.,
Rockford, IL, USA) for western blot analysis. Protein homogenates
were separated on 10% SDS-PAGE gels, transferred to nitrocellulose
membranes, and western blotting with mouse anti-human monoclonal
antibodies against nuclear factor-κB (NF-κB p65; 1:1,000; cat. no.
610869, BD Biosciences) and caspase 3 (1:1,000; cat. no. 9664, Cell
Signaling Technology, Inc., Danvers, MA, USA) was performed at 4°C
overnight. Nitrocellulose membranes were then incubated with Texas
Red AffiniPure goat anti-mouse immunoglobulin G (ZSGB-BIO, Beijing,
China) secondary antibodies for 2 h at room temperature, and the
blots were developed with a SuperSignal chemiluminescence detection
kit (Pierce Biotechnology, Inc.). The resulting immunoblotting was
visualized with an Image Station 400 (Kodak, Tokyo, Japan).
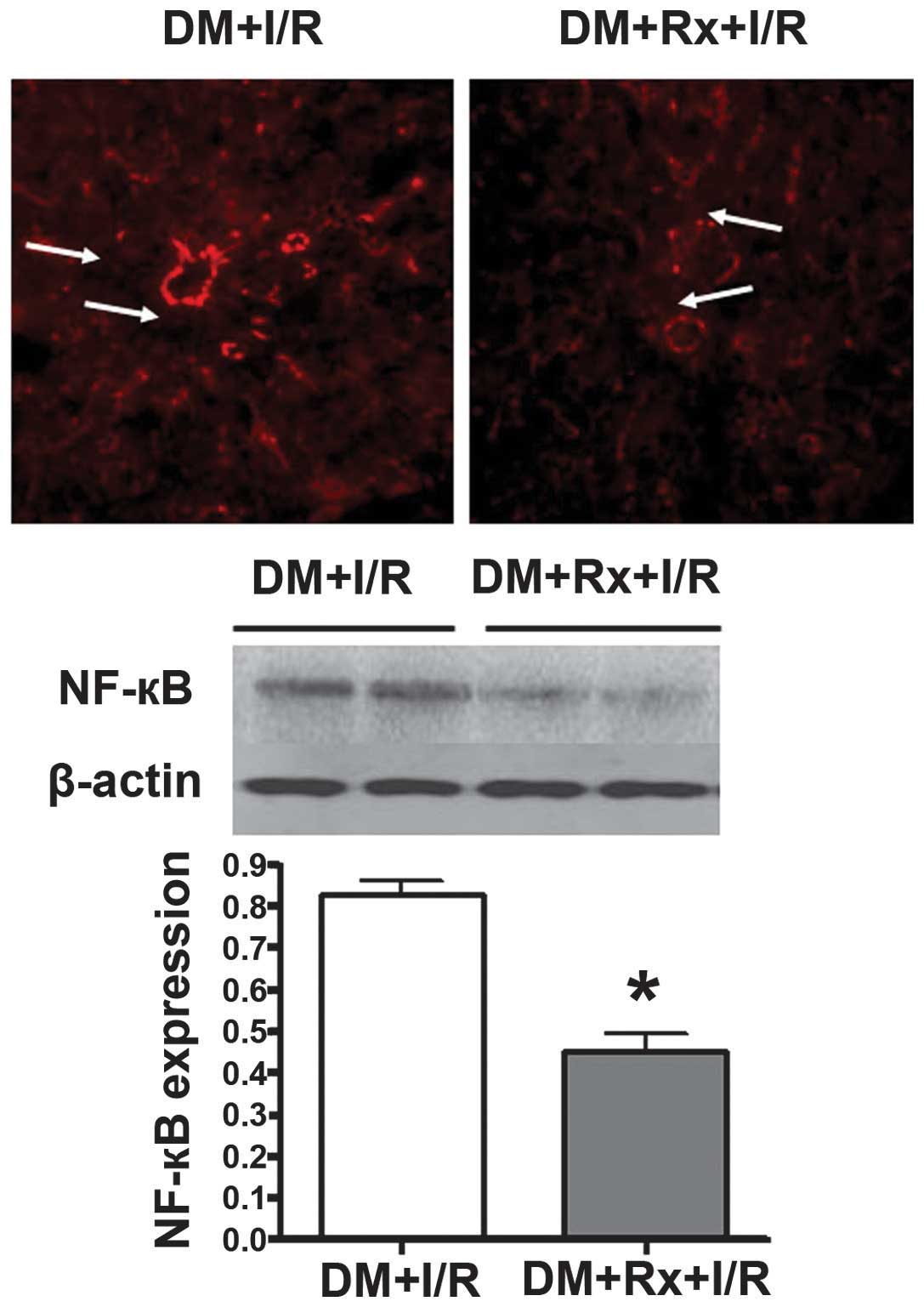
Detection of NF-κB p65 expression
To reveal the location of NF-κB p65 expression in
ischemic liver tissue, immunohistochemical staining was performed.
Paraformaldehyde-fixed liver tissues were cut into 4–5-µm semi-thin
sections and underwent antigen retrieval. Briefly, the sections
were incubated in a water bath at 80°C for 30 min in 50 mM sodium
citrate (pH 8.5–9.5). Subsequently, the sections were stained with
a mouse anti-human monoclonal antibody against NF-κB p65 (1:250; BD
Biosciences) at 4°C for 24 h. An IX71 confocal microscope (Olympus
Corporation, Tokyo, Japan) was used to examine the images.
Assessment of apoptosis in the liver
tissue
The liver tissue was collected following I/R injury.
Apoptosis was detected by a DNA ladder assay and the analysis of
cleaved caspase 3 expression. DNA was extracted from the ischemic
liver tissue by repeated cell disruption in 0.15 M NaCl and
SDS-proteinase K (Beyotime Biotechnology, Shanghai, China),
followed by purification with hydroxybenzen-chloroform-isoamyl
alcohol (14). The DNA was incubated
with protein enzyme K (Guangzhou Dongsheng Biotech Co., Ltd.,
Guangzhou, China) for 10 h in a 37°C environment and then
precipitated using ethanol. DNA ladders were subjected to gel
electrophoresis on a 2% agarose gel using a voltage of 50 V.
Western blotting with a monoclonal antibody against cleaved caspase
3 (1:250; Cell Signaling Technology, Inc.) was performed.
Statistical analysis
Data expressed as mean values ± standard error of
the mean were evaluated by analysis of variance (ANOVA) and the
Newman-Keuls tests for multiple comparisons among groups. P<0.05
was considered to indicate a statistically significant result.
Results
Effect of treatment with PKC-β
inhibitor on serum AST and LDH levels
As shown in Tables I
and II, as the time after hepatic
I/R was prolonged, marked increases in serum AST and LDH levels
occurred. Treatment with the PKC-β inhibitor markedly decreased the
serum AST and LDH levels at each time-point. It appeared that
treatment with the PKC-β inhibitor provided protection against I/R
injury. These findings are consistent with the histological
observations shown in Fig. 1.
 | Figure 1.Pathological changes in liver tissue.
Hepatic cell and microvascular injury were observed under a light
microscope and scanning electron microscope (SEM). With hematoxylin
and eosin staining, disordered hepatic lobules, swelling cells and
vacuoles in liver specimens were exhibited in each group, which
implied hepatic I/R injury. As compared with (A) the untreated
group, I/R injury was ameliorated in the (B) Rx treatment group.
Scale bar, 30 µm. Under the SEM, red blood cells were observed to
be blocked, clustered and conglutinated in capillary vessels, and
normal hepatic plates were not evident in (C) the untreated group.
(D) The situation was improved in the treated group. Scale bar, 10
µm. Arrows indicate: (A) impaired cells; (B) mildly impaired cells;
(C) conglutinated red blood cells in capillary vessels; (D) lack of
conglutinated red blood cells in capillary vessels. DM, diabetes
mellitus; I/R, ischemia/reperfusion; Rx, ruboxistaurin. |
 | Table I.Effect of treatment with Rx on serum
AST levels in diabetic rats at different time-points following
hepatic I/R injury (U/l). |
Table I.
Effect of treatment with Rx on serum
AST levels in diabetic rats at different time-points following
hepatic I/R injury (U/l).
| Groups | 1 h | 3 h | 5 h |
|---|
| DM + I/R | 83.2±27.1 |
92.8±26.5a |
145.8±25.3b |
| DM + Rx + I/R |
64.3±24.6c |
83.2±20.9a,d |
122.1±23.8b,c |
 | Table II.Effect of treatment with Rx on serum
LDH levels in diabetic rats at different time-points following
hepatic I/R injury (U/l). |
Table II.
Effect of treatment with Rx on serum
LDH levels in diabetic rats at different time-points following
hepatic I/R injury (U/l).
| Groups | 1 h | 3 h | 5 h |
|---|
| DM + I/R | 123.2±36.1 |
284.5±41.5a |
360.8±32.1b |
| DM + Rx + I/R |
114.8±27.9c |
135.6±38.6a,d |
213.2±34.5b,d |
Serum TNF-α and ICAM-1 levels in
diabetic rats with hepatic I/R injury
Serum TNF-α levels in untreated diabetic rats
increased as the time following the hepatic I/R procedure was
prolonged before reaching a peak at 3 h, and then decreasing at 5
h. The TNF-α levels in the rats treated with the PKC-β inhibitor
were significantly lower than those in the untreated rats at all
time-points (P<0.01; Table
III). Serum ICAM-1 levels in the untreated diabetic rats
gradually increased as the time following the hepatic I/R procedure
was prolonged. The ICAM-1 levels in the rats treated with the PKC-β
inhibitor were significantly lower than those in the untreated rats
at all time-points (P<0.01; Table
IV).
 | Table III.Effect of treatment with Rx on serum
TNF-α levels in diabetic rats at different time-points following
hepatic I/R injury (ng/l). |
Table III.
Effect of treatment with Rx on serum
TNF-α levels in diabetic rats at different time-points following
hepatic I/R injury (ng/l).
| Groups | 1 h | 3 h | 5 h |
|---|
| DM + I/R | 1260±128 | 1862±145a | 1567±132b |
| DM + Rx + I/R | 1026±114c | 1326±152a,c | 1307±148b,c |
 | Table IV.Effect of treatment with Rx on serum
ICAM-1 levels in diabetic rats at different time-points following
hepatic I/R injury (ng/l). |
Table IV.
Effect of treatment with Rx on serum
ICAM-1 levels in diabetic rats at different time-points following
hepatic I/R injury (ng/l).
| Groups | 1 h | 3 h | 5 h |
|---|
| DM + I/R | 263.3±38.2 |
465.7±31.4a |
689.3±37.8b |
| DM + Rx + I/R |
189.1±31.8c |
326.4±26.7a,c |
495.2±29.4b,c |
Expression of NF-κB in the liver
tissue of diabetic rats with hepatic I/R injury
The expression of NF-κB in the liver tissue was
examined by immunohistochemical staining of the tissue with an
antibody against NF-κB p65. Proteins from the ischemic liver tissue
of the two groups were collected in order to perform western blot
analysis with a monoclonal antibody against NF-κB p65. The
immunohistochemical staining results revealed that the activation
and expression of NF-κB, mainly located in the hepatic sinusoids
and portal area, was present in the two groups of rats at 5 h after
I/R. The staining was intense in the untreated group, and that in
the treatment group was markedly lower (arrows in Fig. 2). Similarly, the activation and
expression of NF-κB p65 in the nuclear extracts from the liver
tissue were identified to be significantly lower in the Rx
treatment group compared with those in the untreated group by
western blot analysis (0.46±0.10 vs. 0.82±0.09, respectively;
P<0.01).
Cell apoptosis in the liver
tissue
Apoptosis was evaluated by DNA ladder assay and the
analysis of cleaved caspase 3 expression. DNA agarose
electrophoresis revealed the presence of DNA degradation in the
liver tissue in the two groups of rats following I/R. DNA segments,
at regular lengths of 180–200 bp, appearing as a DNA ladder, were
more evident in the untreated group compared with the treatment
group. (Fig. 3A) The expression of
caspase 3 in the liver tissue was revealed to be significantly
lower in the treatment group than in the untreated group by western
blot analysis (0.52±0.09 vs. 1.36±0.12, respectively; P<0.01;
Fig. 3B).
Pathological changes in liver
tissue
Hepatic cell and hepatic microvascular injury were
observed by light microscopy and scanning electron microscopy. With
H&E staining, disordered hepatic lobules, swelling cells and
vacuoles in the liver specimens were visible in each group, which
implied that hepatic I/R injury had occurred. The I/R injury was
ameliorated in the treatment group. Under the SEM, it was observed
that red blood cells were blocked, clustered and conglutinated in
capillary vessels, and normal hepatic plates were not evident. The
situation was observed to be improved in the treatment group
(arrows in Fig. 1).
Discussion
Diabetic microvascular complications characterized
by barrier dysfunction have been linked to the activation of PKC-β
(15), with disordered endothelial
function and the subsequently increased transport of
injury-associated factors as characteristics. Increased
permeability of proteins and macromolecules has been observed in
tissues of the retina, kidney and arterial aorta in diabetic
animals (16). Activation of PKC-β
is commonly considered as an important initial cause of
microvascular damage. Correspondingly, microvascular complications
induced by the activation of PKC-β in target organs, such as
increased glomerular filtration rate and retinal edema, could be
diminished by treatment with the PKC-β inhibitor Rx (17).
The activation and expression of NF-κB plays a
specific role in the development of I/R injury in the heart, brain,
liver, kidney and other organs, which is described as cyclic
activation (18,19). NF-κB regulates the genetic expression
of ICAM-1 of the adhesion molecule family, the proinflammatory
factor TNF-α and P-selectin. These inflammatory factors promote the
activation of NF-κB (20,21).
Apoptosis of hepatocytes is the detrimental
consequence of the elevated release of inflammatory factors and
overexpression of adhesion molecules (22,23), and
significantly contributes to hepatic I/R injury. Reperfusion of the
ischemic liver has been reported to activate Kupffer cells,
increase the release of TNF-α, trigger apoptotic genes, activate
caspase and cause degradation, leading to the emergence of DNA
fragments and apoptotic bodies (24). Previous investigators have documented
that liver endotheliocyte damage, microvascular dysfunction and the
activation of Kupffer cells are involved in caspase-mediated
apoptosis (25–27). These observations provide an
explanation for the results of the present study.
The results of the present study documented that
serum AST, LDH, TNF-α and ICAM-1 levels exhibited marked increases
in the untreated I/R group and clear reductions in the group
treated with the PKC-β inhibitor Rx. Pathological damage observed
under a light microscope and TEM, and NF-κB expression detected by
immunohistochemical staining, were attenuated in the treatment
group. These results indicate that the activation of PKC-β in
diabetic rats may result in damage to the hepatic microvascular
barrier, thereby increasing the transport of injury-associated
factors in liver tissues, leading to the activation of NF-κB.
Conversely, NF-κB stimulates the genetic transcription of TNF-α and
ICAM-1. Elevated expression of TNF-α and ICAM-1 has been documented
to induce apoptosis mediated by caspase, accelerate hepatocellular
apoptosis and aggravate pathological damage during hepatic I/R
injury (28). The present results
are consistent with previous studies (29,30). Xu
et al (31) provided
definitive evidence of the activation of NF-κB and expression of
TNF-α and ICAM-1 mRNA in whole liver extracts during hepatic I/R
injury; the activity of NF-κB was elevated in a time-dependent
manner. This is a vicious circle, which may be inhibited with PKC-β
inhibitor treatment.
The results obtained in the present study support
the hypothesis that treatment with a PKC-β inhibitor may play a key
role in controlling the microvascular injury induced by the
activation of PKC-β, by attenuating damage to the barrier function
and endothelial cells as well as by reducing the transport of TNF-α
and the adhesion of ICAM-1 during hepatic I/R injury. This should
break the vicious circle caused by the activation of NF-κB and the
overexpression of TNF-α. Accordingly, the success rate of hepatic
surgery in diabetic patients is likely to be improved as a result
of decreased hepatic apoptosis and pathological injury during
hepatic I/R injury. Confirmation of the hypothesis that PKC-β
inhibitor treatment prior to hepatic surgery will improve clinical
outcomes in diabetic patients with liver disease requires
evaluation in further studies.
Intriguing points remain for research in our ongoing
studies. The details of the correlation of PKC-β activation with
diabetic hepatic microvascular injury may be determined with
co-immunoprecipitation. Hepatic I/R injury is precisely regulated
by a variety of proteins and phosphorylated proteins; the specific
proteins involved in this pathology may be further explored.
Acknowledgements
This study was supported by grants from the National
Natural Science Foundation of China (NSFC; no. 81200158), Science
Foundation of Tianjin Health Bureau (no. 2013KZ011) and Key
Research Projects of Tianjin Health Bureau (no. 13KG115).
References
|
1
|
Rahbari NN, Reissfelder C, Koch M, et al:
The predictive value of postoperative clinical risk scores for
outcome after hepatic resection: a validation analysis in 807
patients. Ann Surg Oncol. 18:3640–3649. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Karatzas T, Neri AA, Baibaki ME and Dontas
IA: Rodent models of hepatic ischemia-reperfusion injury, time and
percentage-related pathophysiological mechanisms. J Surg Res.
191:399–412. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Rahbari NN, Garden OJ, Padbury R, et al:
Posthepatectomy liver failure: a definition and grading by the
International Study Group of Liver Surgery (ISGLS). Surgery.
149:713–724. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Schmidt R: Hepatic organ protection: from
basic science to clinical practice. World J Gastroenterol.
16:6044–6045. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Su AP, Cao SS, Le Tian B, et al: Effect of
transjugular intrahepatic portosystemic shunt on glycometabolism in
cirrhosis patients. Clin Res Hepatol Gastroenterol. 36:53–59. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Çekın AH, Gür G, Türkoğlu S, et al: The
protective effect of L-carnitine on hepatic ischemia-reperfusion
injury in rats. Turk J Gastroenterol. 24:51–56. 2013.PubMed/NCBI
|
|
7
|
Yang J, Sun H, Takacs P, et al: The effect
of octreotide on hepatic ischemia-reperfusion injury in a rabbit
model. Transplant Proc. 45:2433–2438. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jin LM, Liu YX, Zhou L, et al: Ischemic
preconditioning attenuates morphological and biochemical changes in
hepatic ischemia/reperfusion in rats. Pathobiology. 77:136–146.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Clarke M and Dodson PM: PKC inhibition and
diabetic microvascular complications. Best Pract Res Clin
Endocrinol Metab. 21:573–586. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wei L, Yin Z, Yuan Y, et al: A PKC-beta
inhibitor treatment reverses cardiac microvascular barrier
dysfunction in diabetic rats. Microvasc Res. 80:158–165. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Budhiraja S and Singh J: Protein kinase C
beta inhibitors: a new therapeutic target for diabetic nephropathy
and vascular complications. Fundam Clinical Pharmacol. 22:231–240.
2008. View Article : Google Scholar
|
|
12
|
Wei L, Sun D, Yin Z, et al: A PKC-beta
inhibitor protects against cardiac microvascular ischemia
reperfusion injury in diabetic rats. Apoptosis. 15:488–498. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yin Z, Fan L, Wei L, et al: FTY720
protects cardiac microvessels of diabetes: a critical role of
S1P1/3 in diabetic heart disease. PLoS One. 7:e429002012.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Goldenberger D, Perschil I, Ritzler M and
Altwegg M: A simple “universal” DNA extraction procedure using SDS
and proteinase K is compatible with direct PCR amplification. PCR
Methods Appl. 4:368–370. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gutterman DD: Vascular dysfunction in
hyperglycemia: is protein kinase. C the culprit? Circ Res. 90:5–7.
2002.PubMed/NCBI
|
|
16
|
Geraldes P and King GL: Activation of
protein kinase C isoforms and its impact on diabetic complications.
Circ Res. 106:1319–1331. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Joy SV, Scates AC, Bearelly S, et al:
Ruboxistaurin, a protein kinase C beta inhibitor, as an emerging
treatment for diabetes microvascular complications. Ann
Pharmacother. 39:1693–1699. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Galloway E, Shin T, Huber N, et al:
Activation of hepatocytes by extracellular heat shock protein 72.
Am J Physiol Cell Physiol. 295:C514–C520. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wang H, Li ZY, Wu HS, et al: Endogenous
danger signals trigger hepatic ischemia/reperfusion injury through
toll-like receptor 4/nuclear factor-kappa B pathway. Chin Med J
(Engl). 120:509–514. 2007.PubMed/NCBI
|
|
20
|
Zhang W, An J, Jawadi H, et al:
Sphingosine-1-phosphate receptor-2 mediated NFκB activation
contributes to tumor necrosis factor-α induced VCAM-1 and ICAM-1
expression in endothelial cells. Prostaglandins Other Lipid Mediat.
106:62–71. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhu YP, Shen T, Lin YJ, et al: Astragalus
polysaccharides suppress ICAM-1 and VCAM-1 expression in
TNF-α-treated human vascular endothelial cells by blocking NF-κB
activation. Acta Pharmacol Sin. 34:1036–1042. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Chen X, Ding WX, Ni HM, et al:
Bid-independent mitochondrial activation in tumor necrosis factor
alpha-induced apoptosis and liver injury. Mol Cell Biol.
27:541–553. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hatano E: Tumor necrosis factor signaling
in hepatocyte apoptosis. J Gastroenterol Hepatol. 22((Suppl 1)):
S43–S44. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Martin J, Romanque P, Maurhofer O, et al:
Ablation of the tumor suppressor histidine triad nucleotide binding
protein 1 is protective against hepatic ischemia/reperfusion
injury. Hepatology. 53:243–252. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Giakoustidis DE, Giakoustidis AE, Iliadis
S, et al: Attenuation of liver ischemia/reperfusion induced
apoptosis by epigallocatechin-3-gallate via down-regulation of
NF-kappaB and c-Jun expression. J Surg Res. 159:720–728. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Huet PM, Nagaoka MR, Desbiens G, et al:
Sinusoidal endothelial cell and hepatocyte death following cold
ischemia-warm reperfusion of the rat liver. Hepatology.
39:1110–1119. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Teoh NC and Farrell GC: Hepatic ischemia
reperfusion injury: pathogenic mechanisms and basis for
hepatoprotection. J Gastroenterol Hepatol. 18:891–902. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Guo JY, Yang T, Sun XG, et al: Ischemic
postconditioning attenuates liver warm ischemia-reperfusion injury
through Akt-eNOS-NO-HIF pathway. J Biomed Sci. 18:792011.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Taki-Eldin A, Zhou L, Xie HY, et al:
Triiodothyronine attenuates hepatic ischemia/reperfusion injury in
a partial hepatectomy model through inhibition of proinflammatory
cytokines, transcription factors, and adhesion molecules. J Surg
Res. 178:646–656. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Coito AJ: Leukocyte transmigration across
endothelial and extracellular matrix protein barriers in liver
ischemia/reperfusion injury. Curr Opin Organ Transplant. 16:34–40.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Xu J, Xie J, Bao M, et al:
NF-kappaB/I-kappaB pathway during ischemia reperfusion injury of
rat liver. Chin Med J (Engl). 116:1146–1149. 2003.PubMed/NCBI
|