Introduction
In 1983, Anderson and Parrish (1) found that specific optical radiation
could damage pigmental structure. Theoretically, this effect could
be applied to target tissues. In 1995, Latina and Park (2) applied this concept and were the first
to conduct laser-selective treatment of the pigment-containing
trabecular meshwork. They showed that a specific wavelength laser
could selectively hit the pigment-containing trabecular cells.
Selective laser trabeculoplasty (SLT) uses the Q-switch doubling
frequency 532 nm neodymium-doped yttrium aluminium garnet (Nd:YAG)
laser with a pulse time of 3 nsec and a diameter of 400 µm to
irradiate the trabecular meshwork. SLT selectively targets the
pigmental trabecular cells, while the non-pigmental trabecular
cells and the surrounding tissues are not affected by the laser
energy. The high selectivity and extremely short laser pulse time
can reduce the damage to the surrounding non-pigmented trabecular
tissues. In a previous study, no coagulation due to thermal damage
was observed in the tissues following SLT; however, pigment
granules were disintegrated within trabecular cells and there was
destruction of pigmental trabecular cells (3). By contrast, the surrounding cells and
tissues that did not contain the pigments showed no changes.
Therefore, SLT treatment is safe. In 2001, the Food and Drug
Administration approved the clinical use of SLT and this provided a
novel therapeutic approach for primary open-angle glaucoma (POAG)
(4).
SLT has been widely used in clinical treatment since
2002. Studies have shown that SLT can be used as one of the initial
treatments of patients with POAG or in combination therapy when the
maximum-tolerated medical therapy does not obtain satisfactory
therapeutic effects (5–8). SLT can also be used as a therapeutic
method to reduce the effective dose of anti-glaucoma drugs
(9,10). However, there have not been any
reports on the use of SLT as a treatment of post-trabeculectomy
patients with POAG.
Trabeculectomy is still considered the mainstay for
medically uncontrolled glaucoma (11). Studies have shown that, even when
anti-metabolic drugs are applied during surgery, the five-year
success rate of trabeculectomy is 60–80% (12) and the 15-year success rate is 52–59%
(13,14). The postoperative filtering bleb
scarring is the most important reason for surgical failure
(15). The application of
antimetabolites (such as mitomycin C) can reduce the scarring
caused by filtering blebs and improve the surgical success rate,
but certain patients remain who, due to a number of reasons, fail
the surgeries. Trabeculectomy failure normally needs further laser
or surgical intervention if the maximum medical therapy is
insufficient. The difficulty of repeat trabeculectomy in these
patients is significant. It is widely acknowledged that prior
incisional surgery decreases the success rate of subsequent surgery
for glaucoma (16). This is the most
difficult issue in the treatment of glaucoma. For patients with
advanced glaucoma whose target intraocular pressure (IOP) (≤18
mmHg) cannot be achieved with filtering surgery and the
administration of anti-glaucoma medications, the re-filtering
surgery is a significant challenge for the patients and the
physicians. SLT can reduce the IOP of patients with POAG, with no
significant difference identified in the angle structure of these
patients. Therefore, as a noninvasive treatment method, SLT
provides a novel treatment option for patients with POAG who would
normally require further IOP control following glaucoma
surgery.
Materials and methods
Patients
Patients who were diagnosed with POAG and who
underwent one or more trabeculectomies between May and December
2012 in the Zhongshan Ophthalmic Center, Sun Yat-sen University
(Guangzhou, China) were selected for this study. Following the
surgery, 16 patients (18 eyes) could not obtain the target IOP
following the application of one or several anti-glaucoma drugs.
This included 14 males (15 eyes) and two females (three eyes). The
follow-up period was 6–9 months (Table
I). This study was conducted in accordance with the Declaration
of Helsinki and with approval from the Ethics Committee of Sun
Yat-sen University. Written informed consent was obtained from all
participants.
 | Table I.Basic information for the patients
post-trabeculectomy but pre-selective laser trabeculoplasty. |
Table I.
Basic information for the patients
post-trabeculectomy but pre-selective laser trabeculoplasty.
| Parameter | Value |
|---|
| Age, years | 37.5±11.2
(18–64) |
| Preoperative IOP,
mmHg | 21.3±3.4 (17–32) |
| Corneal thickness,
µm | 527.1±27.1
(485–568) |
| Refraction, D | −2.8±2.1 (0–7.0) |
| Preoperative
medication types, n | 2.8±0.8 (2–4) |
| BCVA | 0.3±0.3
(0.4–1.0) |
| Cup/disc ratio | 0.86±0.10
(0.8–0.9) |
| Initial energy
(mJ) | 0.6±0.1
(0.4–0.7) |
| Treatment energy
(mJ) | 60.9±11.6
(50–83) |
Inclusion criteria
Patients had to meet the diagnostic criteria of POAG
established by the International Society of Geographical and
Epidemiological Ophthalmology (17).
As such, the patient had to i) have lost the majority of his/her
vision with only a 5–10° central or temporal vision island and have
an eyeground exhibiting the typical depression of glaucomatous
optic papilla and a cup/disc (C/D) area ratio of ≥0.8, with a mean
deviation of <-12 dB; ii) have undergone one or more trabecular
surgeries, and been prescribed one or more anti-glaucoma drugs
without obtaining the target IOP; iii) have a previous history
without other ocular surgery; iv) have a previous history without
diabetes and hypertension; v) not plan to become pregnant during
the treatment and observation period; vi) be able to be followed-up
on schedule; and vii) continue their medication for at least three
months before SLT.
Exclusion criteria
The exclusion criteria were as follows: i) Other
types of open-angle glaucoma; ii) achievement of the target IOP
following the trabeculectomy; iii) the patient had previously
undergone argon laser trabeculoplasty or other eye surgeries; iv)
the other eye of the patient was blind; v) systemic or ocular
disease requiring corticosteroid therapy; and vi) the patient was
<18 years old.
Treatment termination indicator
If the intra-experimental IOP reached 30 mmHg for
>4 h, the IOPs of two post-treatment consecutive re-checks were
higher than those prior to the treatment or serious complications
occurred, the experiment was terminated.
Criteria for successful treatment
The treatment was considered to be successful if i)
the IOP following the laser treatment was reduced by >20%
compared with the baseline IOP prior to the treatment, and ii)
there were no serious complications.
Observation parameters and evaluation
indicators
The best corrected visual acuity (BCVA) was
determined with the international standard vision chart. Slit-lamp
examination was performed by observing the cornea, anterior chamber
depth, lens and vitreous body. The Goldman IOP was checked each
time. The ultrasonic corneal pachymeter (DGH 1000; DGH Technology,
Inc., Exton, PA, USA) was used to measure the central corneal
thickness three times, and the average was calculated. IOP
determination was performed using the Goldman applanation tonometer
(AT 900 R®, Haag-Streit USA, Inc., Mason, OH, USA); the IOP was
measured three times and the average IOP was calculated. The
Goldman applanation tonometer (AT 900 R®,Haag-Streit USA, Inc.
Mason, OH, USA) detection time-points were 8:00 a.m., 10:00 a.m.,
12:00 a.m., 2:00 p.m. and 5:00 p.m. These detection time-points are
referred to as IOP fluctuation during day time. The detection
time-point for each measurement of IOP after the follow-up visit
was 10:00±1 h in the morning. Each measurement refers to the
measurement of IOP for the follow up after 1, 3, 7 days and after 1
month. Daytime IOP curve tracing was performed by checking the
daytime IOP curves prior to the treatment and those three, six and
nine months after the treatment. The daytime IOP fluctuation was
equal to the highest daytime IOP measured minus the minimum daytime
IOP measured. The main postoperative complications were observed,
the eyeground was examined by direct ophthalmoscopy and the C/D
ratio was recorded.
SLT treatment
The 360° SLT treatment was performed by the same
physician for all patients in this study. The Ellex SOLO® SLT
Nd:YAG laser treatment apparatus (Ellex Medical Pty Ltd., Adelaide,
Australia) was used. The doubling frequency Q-switch Nd:YAG laser
had a single pulse of visible light, a wavelength of 532 nm, a
pulse width of 3 nsec, a facula spot diameter of 400 µm and an
energy range of 0.3–2.6 mJ. The initial energy of the laser was set
to 0.8 mJ, with 0.1 mJ as the amplitude value when increasing or
decreasing the laser energy. When the bubbles formed, the laser
energy was reduced by 0.1 mJ for the treatment. The single and
non-repeated laser spot treatment was performed towards the
trabecular meshwork along the nasal or temporal side. The
treatments in each quadrant were performed ~25 times, with a 360°
chamber angle.
Statistical analysis
The SPSS 18.0 statistical package (SPSS, Inc.,
Chicago, IL, USA) was used to analyze the data for significance.
The continuous variables with normal distribution were assessed
using the bilateral Student's t-test or t-matching test, while the
variables that did not meet the normal distribution were analyzed
using the Mann-Whitney U test.
Results
The preoperative age, IOP, BCVA, refraction, corneal
thickness and C/D ratio are shown in Table I. The average number of trabecular
surgeries received by all the patients was 1.7±0.5 (range, 1–3).
The post-glaucoma surgery time was 2.4±1.1 years and the average
follow-up time was 6.3 months.
Preoperative medication
The average number of preoperative medications
prescribed per patient was 2.8±0.8. A total of 22.2% of the
patients used four anti-glaucoma eye drop medications, 38.9% of the
patients used three anti-glaucoma eye drop medications and 38.9% of
the patients used two anti-glaucoma eye drop medications.
IOP
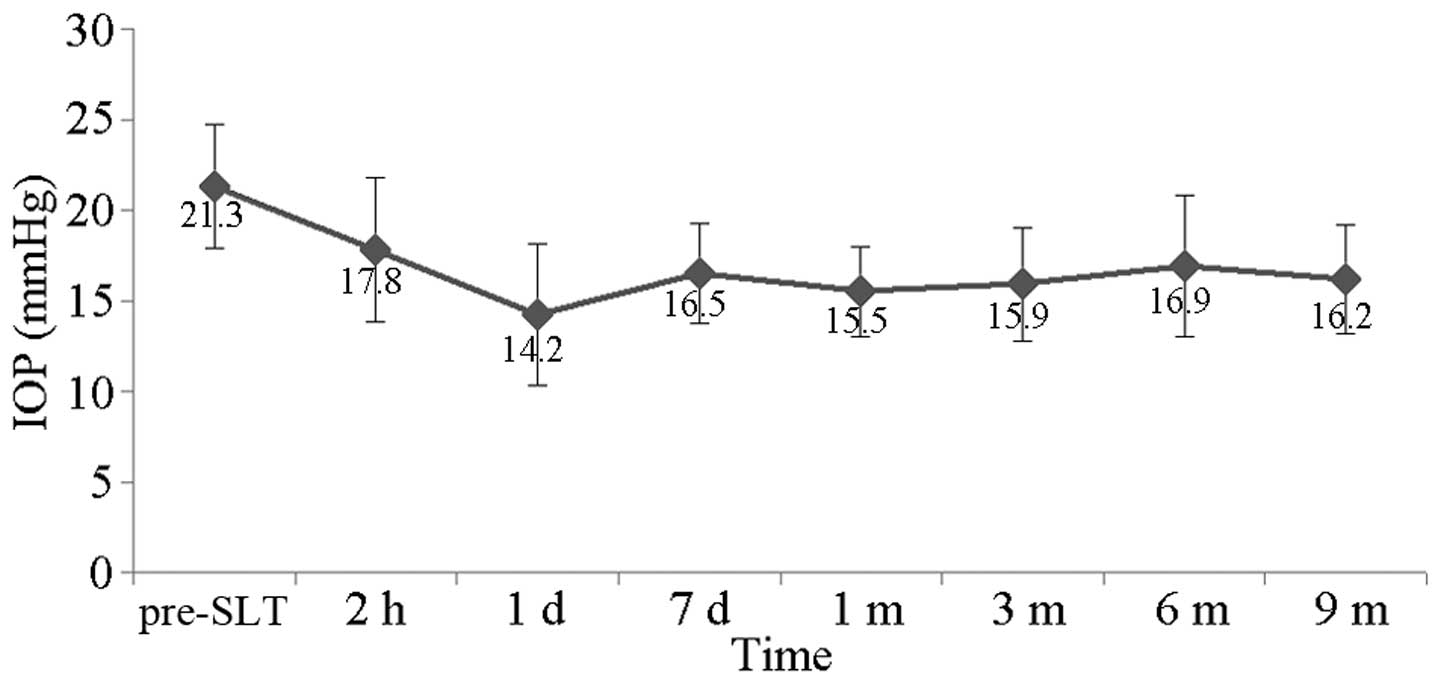
The preoperative IOP in this patient population
ranged between 17 and 32 mmHg, with the average at 21.3±3.4 mmHg.
The postoperative 2-h IOP ranged between 12 and 27 mmHg, with the
average at 17.8±4.0 mmHg. The postoperative one-day IOP was 8–24
mmHg, with the average at 14.2±3.9 mmHg. The postoperative
seven-day IOP was 12–22 mmHg, with the average at 16.5±2.8 mmHg.
The postoperative one-month IOP was 11–20 mmHg, with the average at
15.5±2.5 mmHg. The postoperative three-month IOP ranged between 10
and 24 mmHg, with the average at 15.9±3.1 mmHg. The postoperative
six-month IOP ranged between 11 and 26 mmHg, with the average at
16.9±3.9 mmHg. The postoperative nine-month IOP ranged between 11
and 19 mmHg, with the average at 16.2±3.0 mmHg. The IOP time curve
is shown in Fig. 1. The
postoperative IOP decreased significantly when compared with the
preoperative IOP (t=5.820, P<0.001). The IOP of all the patients
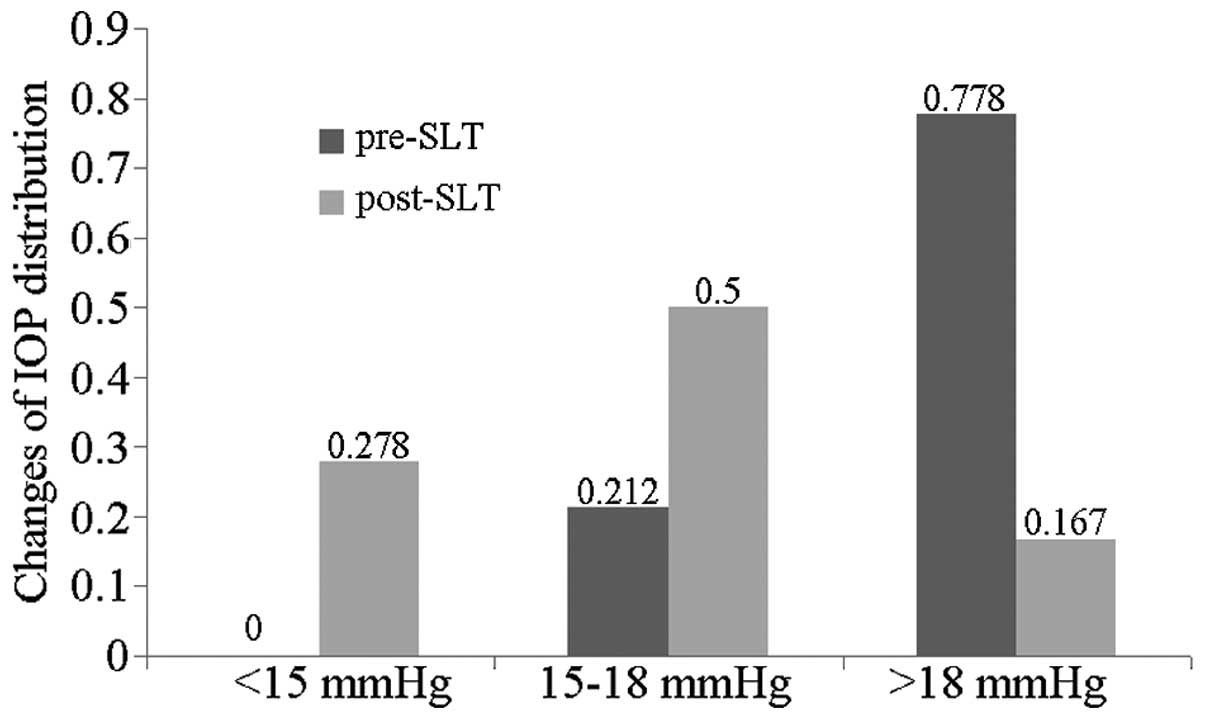
prior to SLT was >15 mmHg and the IOP of 77.8% of the patients
was >18 mmHg, with the average follow-up period of 6.3 months.
The IOP of 27.8% of the patients was <15 mmHg, and the patients
with an IOP >18 mmHg saw a reduction in their IOP by 16.7%. The
changes in IOP distribution prior and subsequent to SLT are shown
in Fig. 2. Three patients failed the
treatment, one patient was prescribed anti-glaucoma medication, and
two patients received the second anti-glaucoma surgery.
Success rate
The reduction in IOP in all the patients (100%) was
>20% one day after the treatment. In the last follow-up, 77.7%
of the patients had a reduction in their IOP of ≥20%.
Effect of SLT on IOP fluctuation
The average IOP fluctuation prior to SLT was 4.1±1.4
mmHg, and the postoperative IOP fluctuation was 2.6±1.1 mmHg
(t=3.424, P=0.003).
Adverse reactions
The most common postoperative adverse reactions were
mild anterior chamber inflammation, mild eye pain, fuzzy vision and
pink eye, which returned to normal 24–48 h after the procedure.
None of the patients appeared to have transient ocular
hypertension. The gonioscopy was performed in the late follow-up
and revealed no formation of peripheral anterior synechia (Table II).
 | Table II.Post-selective laser trabeculoplasty
adverse reactions. |
Table II.
Post-selective laser trabeculoplasty
adverse reactions.
| Adverse reaction | n (%) |
|---|
| Transient ocular
hypertension | 0 (0.0) |
| Pink eye | 10 (55.6) |
| Fuzzy vision | 6
(33.3) |
| Mild eye pain | 4
(22.2) |
Discussion
Clinically, glaucoma treatment has focused on
reducing IOP. It has been recognized that reducing IOP to normal
levels is insufficient in the control of IOP in patients with
advanced glaucoma (18). The
different disease course of glaucoma and the different degrees of
optic nerve damage can result in a different tolerance of retinal
ganglion cells and lamina cribrosa towards IOP. Therefore, the
target IOP specific to each patient with glaucoma must be
determined. The concept of a target IOP is not only dependent upon
the ‘individual tolerance pressure’, but is also determined by the
threshold pressure. The threshold pressure is the IOP under which
there would be no further damage to the glaucomatous optic nerve
during treatment or follow-up. Under this IOP, the loss rate of
retinal ganglion cells would not be greater than that induced by
age, and the optic neuropathy may be decelerated or even
terminated. Practice has proven that IOP reduction can effectively
control the damage to the visual field in glaucomatous patients,
and can delay the progression speed of glaucomatous optic
neuropathy. Furthermore, fewer fluctuations in IOP can reduce the
glaucomatous visual impairment. Patients with advanced glaucoma
require reduced IOP to protect the already-damaged optic nerves
(19,20).
The tolerance of optic nerves in patients with
advanced glaucoma towards IOP is significantly decreased and, in
order to prevent further glaucomatous damage, it is best to reduce
the IOP to <15 mmHg (21,22). All the patients in this study were
patients with advanced POAG, and the average post-glaucoma surgery
time was 2.4 years. The patients had received anti-glaucoma surgery
1.7 times, on average, and the average number of anti-glaucoma
medications received by each patient was 2.8. The average
preoperative IOP was 21.3 mmHg. During the final post-SLT
follow-up, the mean postoperative IOP decreased to 16.2 mmHg, with
the success rate at 77.7%. In this study, the IOP of all the
patients was >15 mmHg prior to SLT, and the IOP of 77.8% of the
patients was >18 mmHg. Following SLT, the IOP of 27.8% of the
patients was <15 mmHg, and 83.3% of the patients had an IOP of
≤18 mmHg. The average reduction amplitude of SLT in the patients
with advanced POAG that had received the filtering surgery was ~5.1
mmHg, which was the same as the therapeutic results of those who
had not received the filtering surgery (4). A previous study showed that each 1 mmHg
reduction in IOP in patients with advanced glaucoma reduced their
vision loss by 10% (18,23). Studies of advanced glaucoma therapy
have also shown that the level of IOP is positively correlated with
the visual field damage (24,25).
During the six-year follow-up, the patients with an average IOP of
<18 mmHg had little or no vision loss, while those with an IOP
>18 mmHg exhibited clear and progressive vision damage. The SLT
decreased the IOP of 83.3% of the patients to <18 mmHg (22,23).
Therefore, in patients with advanced glaucoma, SLT can further
reduce the IOP of the patient based on the application of
anti-glaucoma drugs, helping the patient achieve or approach the
target IOP. This would be an important factor in the protection of
the optic nerve in patients with advanced glaucoma.
During the IOP reduction in the patients with
advanced POAG, it is also necessary to further reduce the IOP
fluctuations. The normal IOP fluctuation range is 3–6 mmHg, while
the IOP fluctuation of patients with POAG would be significantly
higher, 2–3-fold that of the IOP fluctuation in the normal
population. In patients with POAG, the IOP fluctuation should be
strictly controlled, and a number of studies have emphasized the
importance of regulating these fluctuations (24,25). In
the present study, SLT could not only further reduce the IOP of the
patients, which could not be achieved through post-trabeculectomy
medication, but it could also reduce the post-trabeculectomy IOP
fluctuation in patients with advanced glaucoma. Kóthy et al
(26) reported that SLT could reduce
the daytime IOP fluctuation of patients with POAG. Nouri-Mahdavi
et al (27) performed the
Advanced Glaucoma Intervention Study (AGIS) and found through
regression analysis that the IOP fluctuation (daytime or
intra-follow-up) could predict the glaucomatous visual field
progression. IOP fluctuations were more important than the average
IOP, and only when the IOP fluctuation was excluded was the average
IOP value meaningful. Every additional 1 mmHg in IOP fluctuation
[standard deviation (SD)] resulted in a 30% increased risk of
visual field progression. The five-year observation results of the
AGIS showed that the long-term IOP fluctuation of ≤3 mmHg (SD)
caused significant visual field progression, while the IOP
fluctuation of <3 mmHg helped to reduce the visual field
progression. The patients with a long-term IOP fluctuation of
<3.1 mmHg were found to have a 2.89-fold greater risk of visual
field progression than patients with a 2 mmHg fluctuation (28). The study by Hong et al
(29) in 2007 revealed that an IOP
fluctuation of >2 mmHg would also increase the risk of visual
field damage progression, even if the IOP was <18 mmHg. An IOP
fluctuation of <2 mmHg would be better able to prevent the
vision damage. Thus, in the treatment of advanced glaucoma, one
would not only need to control the IOP at levels below the target
IOP, but also reduce the glaucomatous visual field damage caused by
the IOP fluctuation.
In the present study, when patients received the
post-trabeculectomy SLT, the average IOP fluctuation was reduced
from the preoperative value of 4.1 mmHg to the postoperative value
of 2.6 mmHg, and this difference was significant (P<0.05). The
results revealed that SLT could not only reduce the
post-trabeculectomy mean IOP in patients with advanced glaucoma,
but could also control the daytime IOP fluctuation. In glaucomatous
patients with advanced visual field changes, the reduction in IOP
fluctuation would exhibit positive effects towards the protection
of the visual function of the patient.
With regard to the three patients who failed the
treatment, two received additional anti-glaucoma drugs and one
underwent filtering surgery treatment. All the patients exhibited
an IOP reduction, with the greatest reduction observed one day
after the surgery. None of the patients exhibited serious
complications, such as transient high IOP, peripheral anterior
synechia or uveitis.
The chamber angular structure of the patients with
POAG was not changed following the trabeculectomy, which provided
the conditions for the SLT treatment. In terms of the validity of
SLT as a method to further reduce IOP following trabeculectomy, our
study showed that SLT safely, effectively and easily reduced the
IOP, with few side-effects, and provided a viable alternative for
treating patients with advanced POAG. The follow-up of these
patients should be further extended, and a control study should
also be conducted to observe the effects of SLT on IOP
fluctuations.
References
|
1
|
Anderson RR and Parrish JA: Selective
photothermolysis: precise microsurgery by selective absorption of
pulsed radiation. Science. 220:524–527. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Latina MA and Park C: Selective targeting
of trabecular meshwork cells: in vitro studies of pulsed and CW
laser interactions. Exp Eye Res. 60:359–371. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kramer TR and Noecker RJ: Comparison of
the morphologic changes after selective laser trabeculoplasty and
argon laser trabeculoplasty in human eye bank eyes. Ophthalmology.
108:773–779. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Realini T: Selective laser
trabeculoplasty: a review. J Glaucoma. 17:497–502. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hirn C, Zweifel SA, Töteberg-Harms M and
Funk J: Effectiveness of selective laser trabeculoplasty in
patients with insufficient control of intraocular pressure despite
maximum tolerated medical therapy. Ophthalmologe. 109:683–690.
2012.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Koucheki B and Hashemi H: Selective laser
trabeculoplasty in the treatment of open-angle glaucoma. J
Glaucoma. 21:65–70. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Klamann MK, Maier AK, Gonnermann J and
Ruokonen PC: Adverse effects and short-term results after selective
laser trabeculoplasty. J Glaucoma. 23:105–108. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Bovell AM, Damji KF, Hodge WG, Rock WJ,
Buhrmann RR and Pan YI: Long term effects on the lowering of
intraocular pressure: selective laser or argon laser
trabeculoplasty? Can J Ophthalmol. 46:408–413. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Francis BA, Ianchulev T, Schofield JK and
Minckler DS: Selective laser trabeculoplasty as a replacement for
medical therapy in open-angle glaucoma. Am J Ophthalmol.
140:524–525. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Abdelrahman AM and Eltanamly RM: Selective
laser trabeculoplasty in Egyptian patients with primary open-angle
glaucoma. Middle East Afr J Ophthalmol. 19:299–303. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wells AP, Bunce C and Khaw PT: Flap and
suture manipulation after trabeculectomy with adjustable sutures:
titration of flow and intraocular pressure in guarded filtration
surgery. J Glaucoma. 13:400–406. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Law SK, Shih K, Tran DH, Coleman AL and
Caprioli J: Long-term outcomes of repeat vs initial trabeculectomy
in open-angle glaucoma. Am J Ophthalmol. 148:685–695. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Suzuki R, Dickens CJ, Iwach AG, Hoskins HD
Jr, Hetherington J Jr, Juster RP, Wong PC, Klufas MT, Leong CJ and
Nguyen N: Long-term follow-up of initially successful
trabeculectomy with 5-fluorouracil injections. Ophthalmology.
109:1921–1924. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chen TC, Wilensky JT and Viana MA:
Long-term follow-up of initially successful trabeculectomy.
Ophthalmology. 104:1120–1125. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Picht G and Grehn F: Classification of
filtering blebs in trabeculectomy:biomicroscopy adn functionality.
Curr Opin Ophthalmol. 9:2–8. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Olali C, Rotchford AP and King AJ: Outcome
of repeat trabeculectomies. Clin Experiment Ophthalmol. 39:658–664.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Foster PJ, Buhrmann R, Quigley HA and
Johnson GJ: The definition and classification of glaucoma in
prevalence surveys. Br J Ophthalmol. 86:238–242. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Leske MC, Heijl A, Hussein M, Bengtsson B,
Hyman L and Komaroff E: Early Manifest Glaucome Trial Group.
Factors for glaucoma progression and the effect of treatment: the
early manifest glaucoma trial. Arch Ophthalmol. 121:48–56. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hong S, Seong GJ and Hong YJ: Long-term
intraocular pressure fluctuation and progressive visual field
deterioration in patients with glaucoma and low intraocular
pressures after a triple procedure. Arch Ophthalmol. 125:1010–1013.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Inatani M, Iwao K, Inoue T, Awai M, Muto
T, Koga T, Ogata-Iwao M, Hara R, Futa R and Tanihara H: Long-term
relationship between intraocular pressure and visual field loss in
primary open-angle glaucoma. J Glaucoma. 17:275–279. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Shirakashi M, Iwata K, Sawaguchi S, Abe H
and Nanba K: Intraocular pressure-dependent progression of visual
field loss in advanced primary open-angle glaucoma: a 15-year
follow-up. Ophthalmologica. 207:1–5. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
No authors listed. The Advance Glaucoma
Intervention Study (AGIS): 7. The relationship between control of
intraocular pressure and visual field deterioration. AGIS
Investigators. Am J Ophthalmol. 130:429–440. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
AGIS Investigators: The Advanced Glaucoma
Intervention Study (AGIS): 12. Baseline risk factors for sustained
loss of visual field and visual acuity in patients with advanced
glaucoma. Am J Ophthalmol. 134:499–512. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Konstas AG, Hollo G, Astakhov YS, Teus MA,
Akopov EL, Jenkins JN and Stewart WC: Factors associated with
long-term progression or stability in exfoliation glaucoma. Arch
Ophthalmol. 122:29–33. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Heijl A, Leske MC, Bengtsson B, Bengtsson
B and Hussein M: Early Manifest Glaucoma Trial Group: Measuring
visual field progression in the Early Manifest Glaucoma Trial. Acta
Ophthalmol Scand. 81:286–293. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kóthy P, Tóth M and Holló G: Influence of
selective laser trabeculoplasty on 24-hour diurnal intraocular
pressure fluctuation in primary open-angle glaucoma: a pilot study.
Ophthalmic Surg Lasers Imaging. 41:342–347. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Nouri-Mahdavi K, Hoffman D, Coleman AL,
Liu G, Li G, Gaasterland D and Caprioli J: Advanced Glaucoma
Intervention Study: Predictive factors for glaucomatous visual
field progression in the Advanced Glaucoma Intervention Study.
Ophthalmology. 111:1627–1635. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Asrani S, Zeimer R, Wilensky J, Gieser D,
Vitale S and Lindenmuth K: Large diurnal fluctuations in
intraocular pressure are an independent risk factor in patients
with glaucoma. J Glaucoma. 9:134–142. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Hong S, Seong GJ and Hong YJ: Long-term
intraocular pressure fluctuation and progressive visual field
deterioration in patients with glaucoma and low intraocular
pressures after a triple procedure. Arch Ophthalmol. 125:1010–1013.
2007. View Article : Google Scholar : PubMed/NCBI
|