Introduction
Liver abscess is type of liver suppurative lesion
caused by microorganisms such as bacteria, fungus or Entamoeba
histolytica. The mortality rate may reach 10–30% if liver
abscess patients fail to receive timely treatment (1). Generally, liver abscesses are
catalogued into three types: Bacterial liver abscess, mixed
infection by numerous kind of bacterial, comprise ~80% of liver
abscess cases; E. histolytica-induced abscesses account for
10% of cases; and fungus-induced liver abscesses account for
<10% of cases (2,3). Approximately 8–16/100,000 of the total
number of people who were admitted to hospital are caused by liver
abscess (4). The majority of liver
abscess patient are 60–70 years old. Similar rates of liver
abscesses are exhibited by males and females; however, female
patients typically have an improved prognosis compared with males.
The most common causes of fatality in patients with liver abscess
include septicopyemia, multiple organ failure and liver failure.
Treatment options for bacterial liver abscesses include
antibiotics, alone or in combination with percutaneous catheter
drainage, surgical drainage or surgical resection. Treatment
options for E. histolytica and fungus liver abscesses may
conservatively include anti-amoeba and anti-fungal medication, or
treatment measures similar to those for bacterial liver abscess.
Hepatic abscesses are relatively common in Asian countries
(5). However, the report of a
typical ‘bull's eye’ sign hepatic abscess caused by
Acinetobacter baumannii in a tumor patient is rare and could
easily be to misdiagnosed as hepatic metastasis. During real-time
contrast-enhanced ultrasonography (CEUS), lesions disappear with an
intense and prolonged enhancement after contrast media injection.
Typical contrast agents are microbubbles containing gas which are
injected intravenously into the circulation. Ultrasonic imaging
using microbubble contrast agents enhances the ultrasound
backscatter, reflection of the ultrasound waves, in order to
produce a sonogram with increased contrast due to the increased
echogenicity difference (6–8). Once diagnosed, patients with hepatic
abscesses typically recover following conservative surgical
treatment or anti-inflammatory drainage therapy, and the
characteristic ‘bull's eye’ sign in the liver gradually disappears
(9,10).
Case report
A 51-year-old male patient presented at the Zhongnan
Hospital of Wuhan University (Wuhan, China) in October 2013 for
treatment due to flatulence in the right upper abdomen and two days
of fever. The patient experienced pain in the right upper abdomen
due to the pressure. The patient had previously undergone a radical
surgical operation for carcinoma of the stomach and
pancreaticoduodenectomy. Written informed consent was obtained from
the patient. Upon physical examination, the patient complained of
deep tenderness in the right upper abdomen; however, no obvious
masses were detected. Laboratory examinations (Liaison Analyzer;
DiaSorin Deutschland GmbH, Germany) demonstrated that the patient's
hepatic and renal functions and other biochemical indicators were
normal; however, alpha-fetoprotein (AFP) and carcinoembryonic
antigen (CEA) levels were higher than normal.
Conventional and color Doppler ultrasonography were
conducted using a GE E9 ultrasonography machine (GE Healthcare Life
Sciences, Little Chalfont, UK) with an ultrasonography probe
(probe, C1-C5; frequency, 2.0–5.0 MHz; mechanical index, 0.11).
These examinations revealed several slightly low and slightly
strong echoic masses in the liver with a surrounding low echo halo,
representing a ‘bull's eye’ sign. The profile was clear, whereas
the internal echoes were not; the size of one echo was 3.5×2.5 cm
and no obvious blood flow activity was demonstrated. These results
did not indicate the presence of metastatic tumors.
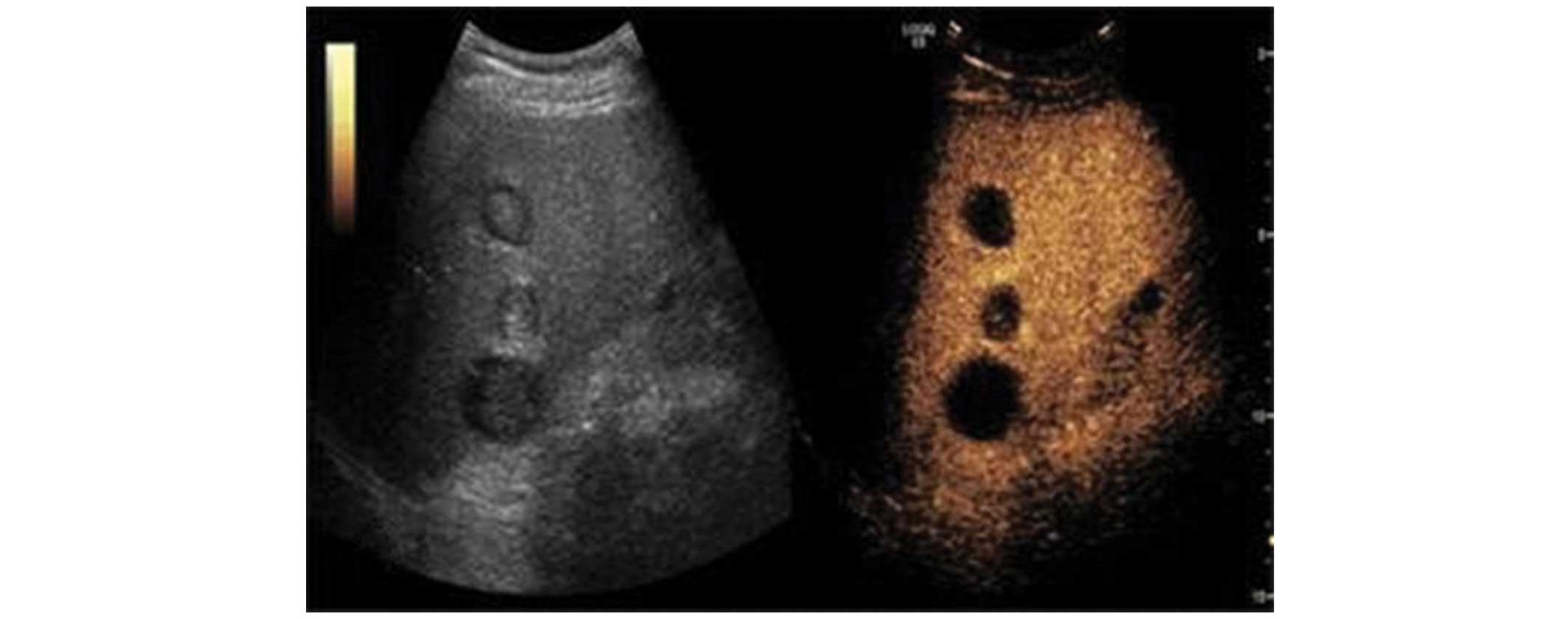
Real-time CEUS was conducted using sulfur
hexafluoride (SF6; SonoVue) as a contrast agent, with a mean
microbubble diameter of 2.5 mm of the phospholipid microcyst.
Real-time CEUS demonstrated that the arterial, portal vein and
prolonged phases were not enhanced in the focal zone of the liver
(Fig. 1). The ultrasound detected
several cystic masses in the liver of the patient. These were
considered to be benign lesions or hepatic abscesses, and a plain
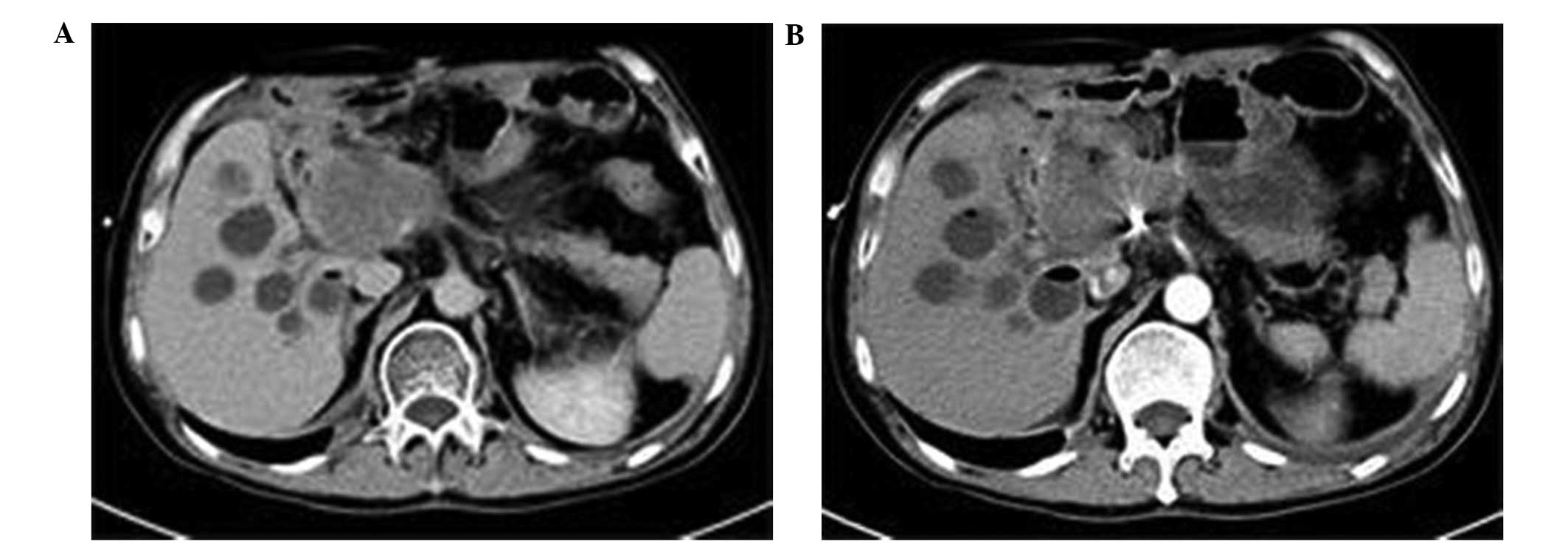
computed tomography (CT) scan (Spiral CT; Siemens, Munich, Germany)
detected several low echo nodules in the liver (Fig. 2A). A number of nodules were detected;
however, no obvious enhancement of the low echo nodule was observed
following completion of an enhanced CT scan (Fig. 2B).
In order to make a definitive diagnosis, a sample
was drawn from the liver by puncture with the guidance of
traveling-wave ultrasonic sounds. A cytologic examination was
completed on the grass green turbid liquid sample, which
demonstrated that the sample contained Acinetobacter
baumannii. Therefore, the final diagnosis was of hepatic
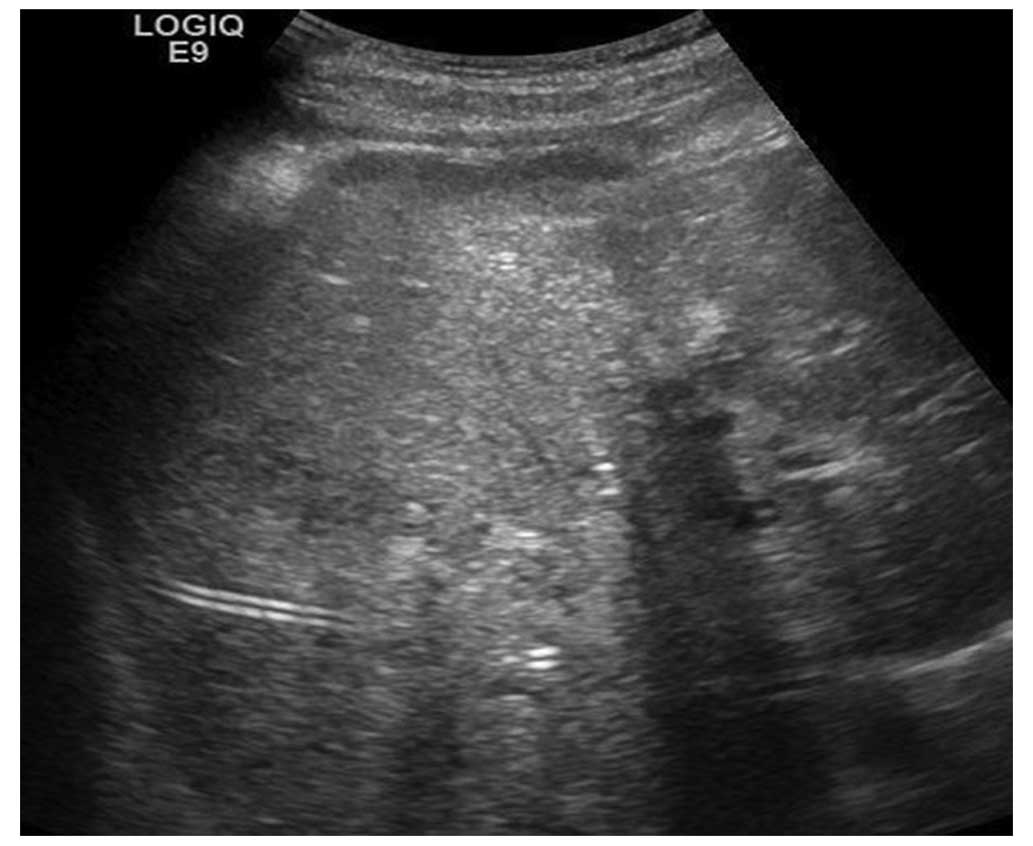
abscess. Anti-inflammatory therapy was subsequently administered
for 5 days, and liquefaction was detected in parts of the low echo
nodule in the liver (Fig. 3). The
therapy comprised of the intravenous administration of 3.0 g
sulperzone and 0.9% normal saline every 8 h, 100 ml metronidazole
every 12 h and two tablets of tigecydine every 12 h. Minimal blood
flow was exhibited around the low echo nodule and, following 30
days of drainage and anti-inflammatory therapy, the characteristic
‘bull's eye’ sign in the liver disappeared. The hepatic tissue
repaired and the patient gradually recovered (Fig. 4). AFP and CEA levels gradually
returned to normal at a 5-month follow-up examination.
Discussion
Hepatic abscesses are common and are usually
straightforward to clinically diagnose. In images generated through
a conventional ultrasonic examination, a typical hepatic abscess
presents as an even or uneven round low echo area with visible
internal masses or spots (11,12).
However, following the increased consumption of clinical drugs, the
manifestations of hepatic abscesses are increasingly atypical
(13). Treatment for bacterial liver
abscess may be conducted as follows: Prior to bacterial culture and
drug sensitivity testing, intensified and large doses
broad-spectrum antibiotic should be to eliminate gram-positive and
gram-negative bacteria. In addition, anaerobion infection may
occur, so anti-anaerobic agents should be applied regularly.
Treatment for E. histolytica may be conducted as follows:
Drugs to eliminate E. histolytica in the inner organs are
commonly used, assisted by radical treatment drugs for the
treatment of intestinal amebiasis (3,14).
Currently, metronidazole is the preferred antibiotic agent. A
typical ‘bull's eye’ sign of hepatic abscess caused by A.
baumannii may be observed in tumor patients, although this is
considered an atypical hepatic abscess. Clinically, it is becoming
increasingly difficult to decipher between atypical hepatic abscess
and hepatic malignant tumors by conventional ultrasonic
examination. As was demonstrated in the present case report,
hepatic abscesses may exhibit a typical ‘bull's eye’ sign; however,
in patients with a medical history of gastric carcinoma and
colorectal cancer this may easily be misdiagnosed as metastatic
colorectal cancer in the liver when using conventional ultrasonic
examination. In the present case report, real-time CEUS was
applied, as a supplement to the conventional ultrasonic
examination, and this determined that the hepatic abscess exhibited
no obvious enhancement in the arterial, portal vein or prolonged
phases, which was inconsistent with the fast-in-fast-out imaging of
hepatic malignant tumors. Furthermore, blood perfusion was observed
on a real-time basis and the structure of the focal zone was
clearly indicated. Based on these manifestations of real-time CEUS,
an accurate ultrasonic diagnosis was achieved in this case.
Therefore, the present case report demonstrated that real-time CEUS
may provide great value for the definitive diagnosis of atypical
hepatic abscesses, particularly in patients with a history of
cancer, and also provides an important reference tool for
differential diagnoses in clinical surgery.
Acknowledgements
This study was supported by the Youth Science Fund
of Wuhan University (grant no. 2014A12).
References
|
1
|
Kuo SH, Lee YT, Li CR, Tseng CJ, Chao WN,
Wang PH, Wong RH, Chen CC, Chen SC and Lee MC: Mortality in
Emergency Department Sepsis score as prognostic indicator in
patients with pyogenic liver abscess. Am J Emerg Med. 31:916–921.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sharma MP and Ahuja V: Amoebic Liver
Abscess. JIACM. 4:107–111. 2003.
|
|
3
|
Sahoo AK and Rauta S: A clinical study on
amoebic liver abscess. Bangladesh J Med Sci. 14:49–52. 2015.
|
|
4
|
Huang CJ, Pitt HA, Lipsett PA, Osterman
FA, Lillemoe KD, Cameron JL and Zuidema GD: Pyogenic hepatic
abscess.Changing trends over 42 years. Ann Surg. 223:600–609. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Rajagopalan S and Langer V: Hepatic
abscesses. Med J Armed Forces India. 68:271–275. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhou K and Chen Z: MRI of Body. Shanghai:
Shanghai Medical University Press. 888–892. 2000.
|
|
7
|
Claudon M, Cosgrove D, Albrecht T, Bolondi
L, Bosio M, Calliada F, Correas JM, Darge K, Dietrich C, D'Onofrio
M, et al: Guidelines and good clinical practice recommendations for
contrast enhanced ultrasound (CEUS) - update 2008. Ultraschall Med.
29:28–44. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Feinstein SB, Coll B, Staub D, Adam D,
Schinkel AF, ten Cata FJ and Thomenius K: Contrast enhanced
ultrasound imaging. J Nucl Cardio. 17:106–115. 2010. View Article : Google Scholar
|
|
9
|
Khanna S, Chaudhary D, Kumar A and Vij JC:
Experience with aspiration in cases of amebic liver abscess in an
endemic area. Eur J Clin Microbiol Infect Dis. 24:428–430. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rajak CL, Gupta S, Jain S, Chawla Y,
Gulati M and Suri S: Percutaneous treatment of liver abscesses:
needle aspiration versus catheter drainage. AJR Am J Roentgenol.
170:1035–1039. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Donovan AJ, Yellin AE and Ralls PW:
Hepatic abscess. World J Surg. 15:162–169. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ryan RS, Al-Hashimi H and Lee MJ: Hepatic
abscesses in elderly patients mimicking metastatic disease. Ir J
Med Sci. 170:251–253. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Brown KT, Gandhi RT, Covey AM, Brody LA
and Getrajdman GI: Pylephlebitis and liver abscess mimicking
hepatocellular carcinoma. Hepatobiliary Pancreat Dis Int.
2:221–225. 2003.PubMed/NCBI
|
|
14
|
Cerwenka H: Pyogenic liver abscess:
Differences in etiology and treatment in Southeast Asia and Central
Europe. World J Gastroenterol. 16:2458–2462. 2010. View Article : Google Scholar : PubMed/NCBI
|